What Is Portal Vein Thrombosis?
Portal vein thrombosis (PVT) happens when a blood clot blocks the portal vein - the main vessel that carries blood from your intestines to your liver. It’s not rare, especially in people with liver disease, cancer, or inherited blood clotting disorders. The clot can be partial or complete, and it can show up suddenly (acute) or build up over time (chronic). Acute PVT is more treatable. Chronic PVT often leads to complications like portal hypertension, where pressure builds up in the liver’s blood vessels, causing fluid buildup, enlarged veins in the esophagus, and even life-threatening bleeding.
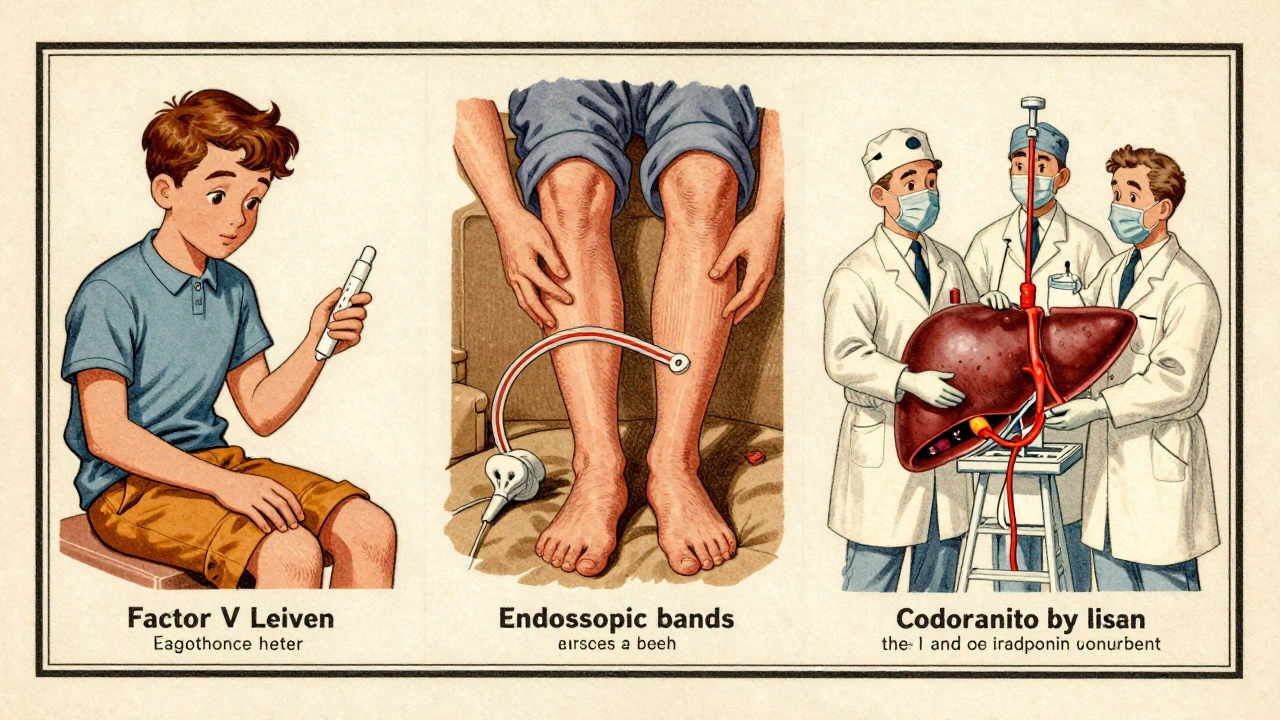
First described in 1868, PVT follows the same rules as other clots: blood flows too slowly, the vessel lining gets damaged, or the blood becomes too sticky. Today, we know that up to 30% of non-cirrhotic PVT cases are tied to genetic clotting disorders like Factor V Leiden. In cirrhotic patients, the clot often forms because the liver can’t make enough clotting regulators anymore.
How Is It Diagnosed?
Ultrasound is the first test doctors reach for. It’s cheap, safe, and catches portal vein clots in 89-94% of cases. A Doppler ultrasound doesn’t just show the clot - it shows if blood is still flowing through or if it’s completely blocked. If the ultrasound is unclear, a CT or MRI scan with contrast gives a clearer picture. These scans can also spot if the body has started building new blood vessels around the blocked vein - a sign called cavernous transformation. That usually means the clot has been there for months or years.
Doctors don’t just look at the clot. They check your liver function with Child-Pugh and MELD scores. These scores tell them how badly your liver is damaged and how risky treatment might be. If you have cirrhosis, they’ll also do an endoscopy to check for varices - swollen veins in your esophagus or stomach that could burst if you start anticoagulation. You might also get blood tests for clotting disorders, especially if you’re young, have no obvious liver disease, or the clot keeps coming back.
When Is Anticoagulation Needed?
For most people with acute PVT, anticoagulation isn’t optional - it’s essential. Studies show that if you start treatment within six weeks, you have a 65-75% chance of the clot dissolving completely. If you wait, that drops to 16-35%. The goal isn’t just to clear the clot. It’s to stop it from spreading to your intestines, which can cause bowel death, and to prevent long-term liver damage.
Guidelines from the American Association for the Study of Liver Diseases (AASLD) and the European Association for the Study of the Liver (EASL) now say: if you don’t have active bleeding or severe liver failure, you should be on anticoagulation. This applies even if you have cirrhosis - as long as it’s not advanced. The biggest mistake? Waiting until symptoms like belly pain or vomiting blood show up. By then, it’s often too late to reverse damage.
What Anticoagulants Are Used?
There are three main types, and which one you get depends on your liver health and risk of bleeding.
- Low Molecular Weight Heparin (LMWH): Often the first choice, especially for cirrhotic patients. It’s given as a daily injection under the skin. Dosing is based on weight - usually 1 mg per kg twice a day. It’s stable, doesn’t need constant blood tests, and works well even when the liver is damaged. In Child-Pugh A or B patients, it clears the clot in 55-65% of cases.
- Warfarin (VKA): An older pill that requires regular INR blood tests to keep levels between 2.0 and 3.0. It’s cheaper but harder to control, especially in cirrhosis. Recanalization rates are lower - around 30-40% - and bleeding risk is higher.
- Direct Oral Anticoagulants (DOACs): These include rivaroxaban, apixaban, and dabigatran. They’re easier to use - no blood tests, fixed doses. In non-cirrhotic patients, they outperform warfarin, with 65-75% clot clearance rates. But they’re not approved for Child-Pugh C cirrhosis. New data from 2024 shows they’re safe in Child-Pugh B7 patients, making them a top choice for many.
The 2024 AASLD update officially added DOACs as an option for compensated cirrhosis, based on the CAVES trial showing they work just as well as LMWH. That’s a big shift from just a few years ago.

How Long Do You Need Treatment?
It’s not one-size-fits-all.
- If your PVT was triggered by something temporary - like recent surgery, infection, or a broken bone - you’ll typically take anticoagulants for 6 months. After that, if the trigger is gone and the clot cleared, you may stop.
- If you have an inherited clotting disorder (like Factor V Leiden), you’ll likely need lifelong treatment. About 25-30% of non-cirrhotic patients fall into this group.
- If you have cancer, anticoagulation continues as long as the cancer is active. PVT can be the first sign of hidden cancer, so doctors will screen for it.
Stopping too early is dangerous. In one study, patients who stopped after 3 months had a 40% chance of the clot returning within a year.
What Are the Risks?
The biggest fear is bleeding. In people with cirrhosis and varices, anticoagulation can trigger a life-threatening bleed from swollen veins in the esophagus. That’s why endoscopic banding is often done before starting anticoagulants. At UCLA, doing this first cut major bleeding from 15% down to 4%.
Other risks:
- Low platelets (below 50,000/μL) make bleeding more likely. Some centers give platelet transfusions to raise counts above 30,000 before starting treatment.
- Ascites (fluid in the belly) increases pressure and bleeding risk. If you have uncontrolled ascites, anticoagulation is delayed.
- Child-Pugh C cirrhosis is a hard stop. DOACs are banned here, and even LMWH is risky. These patients need a liver transplant evaluation instead.
Major bleeding happens in 5-12% of cirrhotic patients versus 2-5% in non-cirrhotic ones. But the risk of not treating - intestinal ischemia, worsening liver failure, death - is often higher.
What If Anticoagulation Doesn’t Work?
If the clot doesn’t shrink after 3-6 months of treatment, or if you develop complications like severe portal hypertension or bowel ischemia, other options exist.
- TIPS (Transjugular Intrahepatic Portosystemic Shunt): A metal tube is placed inside the liver to reroute blood around the blocked vein. It works in 70-80% of cases, but 15-25% of patients develop hepatic encephalopathy - confusion from toxins the liver can’t clear.
- Surgical shunts: Rare now, but used in young patients with no transplant options. High complication rates.
- Thrombectomy: A catheter is threaded in to physically remove the clot. It’s done in specialized centers and clears the vein in 60-75% of cases immediately. But it’s not a long-term fix - you still need anticoagulation afterward.
These are last-resort options. Anticoagulation is still the foundation.
Special Cases: Liver Transplant Candidates
PVT used to be a reason to deny liver transplant. Now, it’s a reason to treat aggressively. Studies show that patients with PVT who get anticoagulation before transplant have an 85% one-year survival rate. Those who don’t get treated? Only 65%. That’s a huge difference.
Transplant centers now routinely screen for PVT in all candidates. If it’s found, they start anticoagulation right away - even if the patient has mild cirrhosis. The goal: clear the clot so the new liver gets good blood flow from day one.
What’s New in 2025?
The field is moving fast.
- Andexanet alfa: Now approved to reverse DOACs in emergencies. This makes doctors more comfortable prescribing them, even in higher-risk patients.
- Abelacimab: A new experimental drug in phase 2 trials. It targets a different part of the clotting system and may work better in liver disease.
- Genetic testing: If you have Factor V Leiden or the prothrombin mutation, you’re 80% more likely to fully recanalize with extended anticoagulation. Testing is becoming standard in non-cirrhotic cases.
- DOAC adoption: Academic centers now use DOACs in 65% of non-cirrhotic cases. Community hospitals are catching up - but slowly.
By 2027, targeted clot-busting drugs and new antifibrinolytics may become options. But for now, anticoagulation is still the gold standard.
What Should You Do If You’re Diagnosed?
Don’t panic. But don’t wait either.
- Get a Doppler ultrasound to confirm the clot and how much of the vein is blocked.
- See a hepatologist - not just a general doctor. PVT management requires expertise.
- Get an endoscopy to check for varices. If they’re there, get them banded before starting anticoagulants.
- Ask for clotting disorder testing if you’re under 50 and have no liver disease.
- Start anticoagulation ASAP if you’re not bleeding. LMWH or a DOAC (if appropriate) is better than warfarin.
- Follow up with imaging at 3 and 6 months to track clot resolution.
Most people who get treated early go on to live normal lives. The key is acting before the clot becomes chronic - and before the liver gets more damaged.
Common Misconceptions
- "I have cirrhosis, so I can’t be treated." False. Many cirrhotic patients - especially Child-Pugh A and B - benefit greatly from anticoagulation. The risk of not treating is often greater.
- "It’s just a clot - it’ll dissolve on its own." No. Without treatment, chronic PVT leads to irreversible liver damage and portal hypertension.
- "I’m on blood thinners for atrial fibrillation, so I’m protected." Not necessarily. PVT needs specific, targeted treatment. The dose and type matter.
Can portal vein thrombosis be cured?
Yes, in many cases. With early anticoagulation, 65-75% of patients achieve complete or near-complete recanalization of the portal vein. Success depends on how soon treatment starts, the underlying cause, and liver health. Chronic PVT is harder to reverse but can still be managed to prevent complications.
Is anticoagulation safe if I have cirrhosis?
It can be - but only if your cirrhosis isn’t advanced. For Child-Pugh A and B patients, LMWH and newer DOACs are safe and effective when used carefully. Endoscopic banding of varices before starting treatment reduces bleeding risk dramatically. But if you’re Child-Pugh C, anticoagulation is usually avoided due to high bleeding risk.
Do I need lifelong anticoagulation for PVT?
Only if you have a permanent risk factor - like an inherited clotting disorder, active cancer, or recurrent PVT. For triggered cases (like after surgery or infection), 6 months is usually enough. Your doctor will reassess based on follow-up scans and your overall health.
Can I take a DOAC if I have liver disease?
Yes - but only if your liver function is mild to moderate. DOACs like rivaroxaban and apixaban are now approved for Child-Pugh A and B7 patients based on 2024 guidelines. They’re not safe for Child-Pugh C. Always check your liver function before starting, and avoid them if you have severe ascites or active bleeding.
What happens if I don’t treat PVT?
Untreated PVT can lead to serious complications: intestinal ischemia (dead bowel tissue), worsening portal hypertension, variceal bleeding, liver failure, and death. In one study, patients who didn’t get anticoagulation had a 22% mortality rate if they developed mesenteric ischemia. Early treatment cuts that risk by more than half.
Final Thoughts
Portal vein thrombosis isn’t something you can ignore. It’s not a one-time event - it’s a warning sign. Whether you have cirrhosis, cancer, or no liver disease at all, the message is the same: get diagnosed early, start anticoagulation promptly, and stay on it as long as needed. The tools are better than ever. The data is clear. The stakes? High. But with the right care, most people don’t just survive - they thrive.






Comments
pvt? i thought it was just a typo for pvt lunch. turns out its a blood clot thing. wow. i had no idea. thanks for the info.
This is actually super useful. I’ve got a cousin with cirrhosis and they just found a clot. I’m sharing this with her doctor.
As a hepatology nurse, I’ve seen too many patients delayed because someone thought "liver disease = can’t anticoagulate." The data is clear: early LMWH or DOACs in Child-Pugh A/B save lives. The real risk is inaction.
The way this post dismantles the myth that cirrhosis is a blanket contraindication is nothing short of revolutionary. It’s not just medical knowledge-it’s a moral imperative. We’ve been burying patients under outdated dogma while the science marched ahead. The CAVES trial alone should’ve changed practice overnight.
I’ve been pushing for DOACs in my clinic since the 2024 update. The biggest barrier isn’t evidence-it’s inertia. Docs still default to warfarin because "that’s what they learned." We need better education, not just guidelines. Also, genetic testing for Factor V Leiden should be standard in anyone under 50 with unexplained PVT. It changes everything.
The recanalization rates for DOACs in non-cirrhotics are statistically significant, yes-but the real-world adherence is abysmal. Patients forget pills. LMWH is inconvenient but reliable. Also, "Child-Pugh B7" is not a real classification. It’s B7 as in MELD? Or Child-Pugh score 7? Ambiguous terminology undermines clinical utility.
I’ve been saying this for years: American medicine is too slow. Europe’s been using DOACs for PVT since 2022. We’re still debating whether to use them in Child-Pugh B? Come on. We have the data. We have the drugs. We have the outcomes. We just don’t have the courage to change.
I’m from Singapore and we’ve had similar shifts here. DOACs are now first-line for non-cirrhotic PVT. The real challenge? Access. In rural areas, patients still get warfarin because labs can’t monitor INR reliably. Telehealth and home INR kits could bridge that gap. Also, the mention of Abelacimab? That’s the future. I’m watching phase 3 trials closely.
I’m a patient with Factor V Leiden and PVT. I started rivaroxaban 6 months ago. My ultrasound at 3 months showed 70% recanalization. I’m not a doctor, but this post got me to ask the right questions. Thank you.
You know what’s worse than a clot? The medical system that treats you like a statistic until you’re bleeding out. I had PVT after a C-section. They dismissed my pain as "postpartum cramps." Two weeks later, I was in ICU with mesenteric ischemia. If this post saves one person from being ignored, it’s worth it.
STOP WAITING. If you’ve been diagnosed, start anticoagulation TODAY. Not tomorrow. Not next week. TODAY. Your liver doesn’t care about your insurance approval. Your intestines don’t care if you’re scared. Act now. Live longer. You got this 💪
Who says we need anticoagulation at all? Maybe the body knows best. Maybe the clot is a protective mechanism. Maybe we’re just over-medicalizing everything. What if the liver is trying to heal itself? Why rush to dissolve it? Evolution didn’t design veins to be anticoagulated.
This is the kind of post that makes me want to throw my stethoscope out the window. All this jargon, all these percentages, and yet we still lose people because someone didn’t get an endoscopy in time. We need less PowerPoint and more bedside presence. The real cure is listening-not lab values.
I’ve been reading everything I can about this since my dad’s diagnosis. I just found out he has a prothrombin mutation. I’m so glad I saw this. I’m printing it out and bringing it to his next appointment. Also, I’m crying now. Thank you.
The notion that anticoagulation is "safe" in cirrhosis is a dangerous oversimplification. The CAVES trial excluded patients with platelets below 50,000, uncontrolled ascites, and active variceal bleeding. Yet clinicians are now prescribing DOACs to Child-Pugh B patients with platelets at 32,000 and 4+ liters of ascites. This is not evidence-it’s wishful thinking dressed in guidelines.