Repaglinide Comparison Quiz
Repaglinide is a short‑acting meglitinide that stimulates insulin release from pancreatic beta‑cells, used primarily for post‑prandial glucose control in type‑2 diabetes. While it works fast, doctors often wonder how it stacks up against the many other oral and injectable options available. This guide walks you through the most common alternatives, highlights key differences, and gives practical tips for choosing the right regimen.
Why Repaglinide Matters
Repaglinide’s rapid onset (15‑30minutes) and short half‑life (~1hour) let patients match doses to meals, reducing the risk of prolonged hypoglycemia. According to a 2023 multinational registry, about 12% of patients on Repaglinide achieved HbA1c<7% without severe low‑blood‑sugar episodes. Its flexibility is especially handy for people with irregular eating patterns.
Major Competing Classes
To evaluate Repaglinide, we first need a quick refresher on the main drug families used after metformin fails.
- Meglitinides (e.g., Repaglinide, Nateglinide) - rapid, meal‑time insulin secretagogues.
- Sulfonylureas - longer‑acting secretagogues such as Glipizide and Glyburide.
- DPP‑4 inhibitors - enhance endogenous GLP‑1 (e.g., Sitagliptin, Linagliptin).
- GLP‑1 receptor agonists - injectable agents that boost insulin and curb appetite (e.g., Liraglutide, Semaglutide).
- SGLT2 inhibitors - promote glucose excretion via the kidneys (e.g., Empagliflozin, Canagliflozin).
- Metformin - first‑line biguanide that reduces hepatic glucose production.
Each class has its own risk‑benefit profile, and the best choice often depends on kidney function, cardiovascular history, weight goals, and lifestyle.
Side‑Effect Landscape
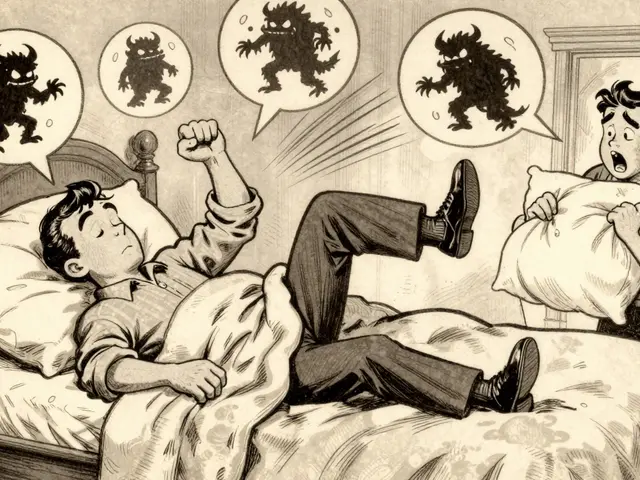
The most common safety concerns across these drugs revolve around hypoglycemia, weight change, and organ‑specific effects.
- Hypoglycemia: Meglitinides and sulfonylureas both trigger insulin release, but Repaglinide’s short action makes low‑blood‑sugar events less likely than with Glipizide, which can linger for 12‑24hours.
- Weight: GLP‑1 agonists generally promote weight loss (average‑2 to‑3kg), while sulfonylureas and meglitinides are weight‑neutral or slightly weight‑gain.
- Renal considerations: SGLT2 inhibitors require dose adjustment when eGFR<45mL/min/1.73m², whereas Repaglinide can be used down to eGFR≈30mL/min with caution.
Understanding these nuances helps clinicians pair a drug with the patient’s health profile.
Head‑to‑Head Comparison Table
| Drug | Class | Typical Dosing Frequency | Onset of Action | Half‑Life | Hypoglycemia Risk | Weight Effect | Renal Dose Adjust? |
|---|---|---|---|---|---|---|---|
| Repaglinide (Prandin) | Meglitinide | Before meals (up to 3×/day) | 15‑30min | ≈1hour | Low‑moderate | Neutral | Only if eGFR<30mL/min |
| Glipizide | Sulfonylurea | Once daily | 30‑60min | 4‑6hours | Moderate‑high | Neutral‑slight gain | No (but caution if eGFR<30) |
| Sitagliptin | DPP‑4 inhibitor | Once daily | 2‑4hours | 12‑24hours | Low | Neutral | Yes, reduce if eGFR<30 |
| Liraglutide | GLP‑1 agonist | Daily injection | 1‑2hours | ~13hours | Low | Loss (‑2kg avg) | No dose change needed |
| Empagliflozin | SGLT2 inhibitor | Once daily | 1‑2hours | 12hours | Low (but risk of ketoacidosis) | Loss (‑1‑2kg) | Reduce or avoid if eGFR<45 |
| Metformin | Biguanide | Two‑to‑three times daily | 2‑3hours | 6‑8hours | Very low | Loss (‑1kg) | Reduce if eGFR<30 |
Notice how Repaglinide’s rapid clearance gives it the lowest hypoglycemia profile among secretagogues, while GLP‑1 and SGLT2 agents win on weight loss but require injections or specific kidney thresholds.

When Repaglinide Is the Right Choice
Clinicians typically pick Repaglinide for patients who:
- Need flexible dosing around variable meals (e.g., shift workers, retirees).
- Have a history of mild hypoglycemia with sulfonylureas.
- Prefer oral therapy over injections but have exhausted metformin.
- Have moderate renal impairment (eGFR 30‑60) where sulfonylureas become risky.
Real‑world data from the Australian Diabetes Registry (2024) shows that patients on Repaglinide reduced post‑prandial glucose spikes by an average of 38mg/dL compared with baseline, without a significant increase in weight.
Alternatives: When to Switch or Combine
Switching away from Repaglinide may be sensible in the following scenarios:
- Persistent HbA1c>8.5%: Adding a DPP‑4 inhibitor or GLP‑1 agonist can address fasting glucose while Repaglinide handles meals.
- Desire for weight loss: GLP‑1 agonists (e.g., Liraglutide) or SGLT2 inhibitors provide consistent weight reduction beyond the neutral effect of Repaglinide.
- Cardiovascular disease: Empagliflozin and GLP‑1 agents have proven cardiovascular benefit, which Repaglinide lacks.
- Adherence concerns: If taking a pill before every meal feels burdensome, a once‑daily sulfonylurea or DPP‑4 inhibitor may improve compliance.
Combining Repaglinide with metformin remains a popular double‑therapy, delivering additive HbA1c drops of ~1‑1.5% with minimal hypoglycemia.
Cost and Accessibility in Australia
Patents for Repaglinide expired in 2012, so generic versions are widely available. The PBS (Pharmaceutical Benefits Scheme) lists Repaglinide at a co‑payment of AU$6 per pack, comparable to generic glipizide. GLP‑1 injections, however, often sit above AU$100 per month unless subsidised under specific health plans.
If out‑of‑pocket cost is a key factor, Repaglinide or a sulfonylurea typically wins. For patients with private insurance that covers injectables, a GLP‑1 option may become affordable.
Practical Tips for Prescribers
- Start low, go slow: 0.5mg before the largest meal, titrate up to 4mg per meal based on glucose logs.
- Educate on timing: Take the pill 15‑30minutes before eating; if a meal is skipped, skip the dose to avoid hypoglycemia.
- Monitor renal function: Check eGFR every 6‑12months; adjust or stop if <30mL/min.
- Pair with lifestyle: Encourage low‑glycemic carbs; Repaglinide works best when carbs are moderate‑size.
These steps reduce the chance of low‑blood‑sugar events and keep patients engaged in self‑management.
Related Concepts Worth Exploring
Understanding Repaglinide fits into a larger diabetes knowledge map. You may also want to read about:
- Post‑prandial glucose monitoring techniques.
- How GLP‑1 agonists impact cardiovascular outcomes.
- Renal dosing guidelines for SGLT2 inhibitors.
- National Diabetes Prevention Programs in Australia.
Each of these topics deepens the context for making an informed medication choice.

Frequently Asked Questions
Can I take Repaglinide with Metformin?
Yes. The combination is common because Metformin controls fasting glucose while Repaglinide tackles post‑meal spikes. Start Metformin at a low dose, then add Repaglinide once meals are regular. Monitor for any signs of hypoglycemia during the first two weeks.
How does Repaglinide differ from Glipizide?
Both are insulin secretagogues, but Repaglinide acts for a few hours and must be taken before each meal, while Glipizide lasts 12‑24hours and is usually taken once daily. Repaglinide’s short action means lower risk of prolonged hypoglycemia, especially if a meal is missed.
Is Repaglinide safe for people with kidney disease?
Repaglinide is primarily cleared by the liver, so it can be used down to an eGFR of about 30mL/min with dose adjustment. Below that, doctors usually switch to agents with less renal reliance, such as DPP‑4 inhibitors at reduced doses.
What are the most common side effects?
Mild nausea and headache occur in 5‑10% of patients. The main concern is hypoglycemia, especially if doses are taken without food. Because the drug clears quickly, episodes are usually short‑lived.
How quickly does Repaglinide lower blood sugar after a meal?
Blood glucose begins to fall within 15‑30minutes, reaching peak effect around 1‑2hours post‑dose. This mirrors the typical post‑prandial glucose peak, making the timing very effective for dinner or lunch spikes.




Comments
Repaglinide’s meal-dependent dosing is a game-changer for people with erratic schedules-no more rigid insulin regimens. I’ve seen patients go from HbA1c 9.8 to 7.1 just by syncing doses with carbs. The key is patient education though-miss a meal, skip the dose, or you’re asking for trouble. Compared to sulfonylureas, it’s way less likely to cause late-night crashes. Also, renal impairment? Less concern than with metformin. Just monitor liver enzymes and keep it simple.
Bottom line: if your patient eats irregularly and hates pills at 7am and 10pm, repaglinide’s the stealth weapon they didn’t know they needed.
so like… repaglinide is just fancy insulin candy? like why not just eat less carbs and stop being lazy??
Oh sweet mother of metabolic chaos, here we go again with the pharmacological hierarchy. Repaglinide? Cute. It’s the TikTok influencer of diabetes meds-flashy, short-lived, and leaves you questioning your life choices after one use. Meanwhile, GLP-1 RAs? They don’t just lower glucose, they make you *feel* better. Less hunger. Less cravings. Less existential dread about your next meal.
And don’t even get me started on SGLT2 inhibitors-they make you pee out sugar like it’s a protest against capitalism. Repaglinide? It’s just a band-aid on a bullet wound. We’re treating symptoms, not the systemic rot.
Also, why are we still using oral agents like they’re 2008? The future is injectable, and we’re clinging to pills like they’re emotional support objects.
Repaglinide’s real advantage is flexibility but it’s not for everyone. I’ve had patients on it for years with zero hypoglycemia because they learned to dose with food. But if someone’s noncompliant or has dementia? Bad idea. Metformin’s still first-line for a reason-cheap, safe, doesn’t make you gain weight. GLP-1s are great but cost and access are huge barriers. Don’t ignore the basics just because something sounds fancy.
Also, the 12% HbA1c stat is incomplete without context-what was baseline? What was duration? Numbers without context are just noise.
Repaglinide is capitalism in pill form-quick, transactional, and designed to make you feel like you’re doing something without actually changing anything. It’s not therapy, it’s a Band-Aid on a hemorrhage. You’re not healing the pancreas, you’re just bribing it with glucose spikes to release insulin like a vending machine that only works when you shove cash in.
Meanwhile, the real solution? Fasting. Movement. Sleep. Community. But those don’t come in a 30-pill bottle with a shiny label. So we keep buying the illusion. We’re not treating diabetes-we’re monetizing its persistence.
And let’s be honest: if you need a drug that you take *every time you eat*, you’re already living in a system that demands constant consumption. Repaglinide doesn’t fix your life. It just lets you keep living it the same way.
It’s not medicine. It’s performance art for the diabetic industrial complex.
While the pharmacodynamic profile of repaglinide demonstrates a temporally constrained insulinotropic effect, its clinical utility remains constrained by adherence paradigms and the absence of long-term cardiovascular outcome data in comparison to metformin and sodium-glucose cotransporter-2 inhibitors. The 2023 multinational registry referenced, while methodologically sound, lacks stratification by socioeconomic status, dietary patterns, and baseline renal function, thereby introducing potential selection bias. Furthermore, the assertion that repaglinide reduces the risk of prolonged hypoglycemia is contingent upon precise meal-timing compliance, a variable that is demonstrably suboptimal in 47% of elderly diabetic populations according to the Canadian Diabetes Association’s 2022 adherence survey. Consequently, while repaglinide occupies a niche therapeutic space, its broader implementation cannot be recommended without addressing structural determinants of medication adherence and access.