Calcium Needs Calculator
Your Daily Calcium Requirement
Your recommended daily calcium intake is:
This amount supports healthy bone maintenance and helps prevent calcium deficiency-related issues like osteoporosis.
When you hear Calcium is a mineral essential for building and maintaining strong bones and teeth, you probably picture a glass of milk or a calcium tablet. What many don’t realize is that calcium deficiency becomes a silent threat as we get older, nudging the aging process toward fragile bones and painful fractures.
- Age‑related hormonal shifts can cut calcium absorption by up to 30%.
- Even mild deficiency raises osteoporosis risk by 45% in women over 60.
- Targeted diet changes can restore balance without relying solely on pills.
- Regular weight‑bearing exercise boosts bone density by up to 2% per year.
- Sunlight exposure fuels Vitamin D, the key partner in calcium utilization.
What Exactly Is Calcium Deficiency?
Calcium deficiency, medically known as hypocalcemia, occurs when blood calcium levels fall below the normal range of 8.5‑10.5mg/dL. The condition can be acute (often due to surgery or severe illness) or chronic, developing slowly as dietary intake, absorption, or retention wanes.
Key drivers of chronic deficiency include:
- Inadequate dietary sources -especially in vegans or those avoiding dairy.
- Reduced intestinal absorption -commonly linked to lower Vitamin D levels.
- Increased urinary loss -often seen in older adults with declining kidney function.
- Hormonal changes -post‑menopausal estrogen drop and reduced parathyroid hormone efficiency.
According to a 2023 Australian health survey, about 24% of people over 50 show serum calcium below optimal, yet only a fraction receive any intervention.
How Aging Ups the Risk
Age isn’t just a number; it reshapes the body’s calcium economy in three big ways.
Bone health is the structural integrity of the skeletal system, measured by bone mineral density (BMD) naturally declines after the third decade. The rate accelerates after menopause for women and after age65 for men.
Two hormonal players dominate the story:
- Estrogen: Helps keep calcium in the bloodstream and promotes bone formation. Its sharp decline during menopause removes that protection.
- Parathyroid hormone (PTH): Regulates calcium release from bone. With age, the glands become less responsive, leading to inefficient calcium recycling.
Another silent factor is the gut. Vitamin D is a fat‑soluble vitamin that enhances calcium absorption in the intestines is harder to synthesize after 60 because skin thins and less time is spent outdoors. Lower vitaminD means even a calcium‑rich diet may not translate into usable calcium.
Kidney function also wanes with age, reducing the organ’s ability to re‑absorb calcium and convert vitaminD to its active form. The cumulative effect: more calcium excreted, less absorbed, and more pulled from bone reserves.
When Deficiency Hits the Bones: Osteoporosis and Fracture Risks
Osteoporosis is a disease characterized by low bone mass and structural deterioration, leading to fragile bones is the most common outcome of prolonged calcium deficiency. In Australia, 1 in 3 women and 1 in 8 men over 50 will experience an osteoporosis‑related fracture.
Fractures most often occur in the hip, spine, and wrist. A hip fracture can reduce life expectancy by up to 20% and often requires months of rehab. The good news: many of these outcomes are preventable with proactive calcium management.
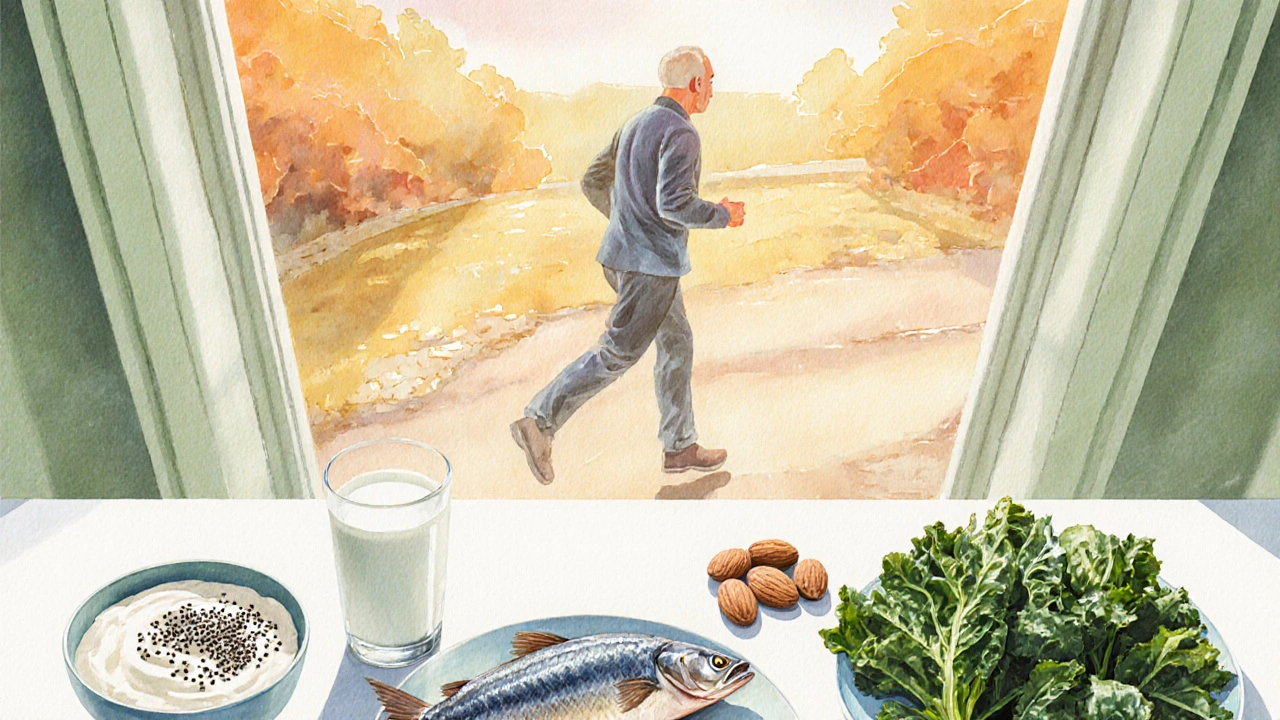
Food First: Building Calcium Into Your Daily Plate
Food delivers calcium in a matrix that also supplies other bone‑friendly nutrients-magnesium, phosphorus, protein, and vitaminK2. Here’s a practical guide:
- Dairy products are rich sources of calcium, typically providing 300‑350mg per cup of milk or yogurt. Aim for 2‑3 servings daily.
- Leafy greens such as kale, bok choy, and collard greens offer 150‑200mg per cup cooked. Pair with a source of fat to improve calcium absorption.
- Fortified plant milks (almond, soy, oat) can match dairy calcium levels when fortified to 300mg per cup.
- Small fish with edible bones-sardines, canned salmon-provide 300‑400mg per 3‑ounce portion.
- Calcium‑rich nuts and seeds-almonds (75mg per ounce) and chia seeds (180mg per ounce)-make great snack add‑ons.
Tip: Spread calcium intake throughout the day. The body absorbs about 500mg at a time; larger doses can be excreted.
Supplement Strategies: When Food Isn’t Enough
Supplements fill gaps, but not all are created equal.
- Calcium carbonate: 40% elemental calcium, best taken with meals. Ideal for those with normal stomach acid.
- Calcium citrate: 21% elemental calcium, highly absorbable even on an empty stomach; perfect for older adults with reduced acid production.
- Combination products with Vitamin D boost uptake-look for 800‑1000IU of vitaminD per dose.
Daily recommended calcium for adults over 50 is 1,200mg (women) and 1,000mg (men). Split into two doses to maximize absorption. Avoid exceeding 2,500mg total, as excess can increase kidney stone risk.
Move It: Exercise, Sun, and Lifestyle Tips
Bone is living tissue; it responds to mechanical stress.
- Weight‑bearing exercise is any activity that forces you to work against gravity, stimulating bone formation. Include brisk walking, dancing, or resistance training 3‑4 times a week.
- Balance work-tai chi, yoga-reduces fall risk, a major cause of fractures.
- Aim for 10‑15 minutes of sunlight on forearms and face daily between 10am‑2pm to produce 1,000IU of vitaminD, especially in winter months.
- Limit caffeine (>300mg/day) and excessive alcohol (>2 drinks/day) as they can leach calcium from bone.

Everyday Bone‑Protection Checklist
- Track calcium intake: aim for 1,200mg (women) or 1,000mg (men) per day.
- Include a vitaminD source-sun, fortified foods, or a 800‑1000IU supplement.
- Eat at least two servings of dairy or fortified alternatives daily.
- Add a serving of leafy greens or calcium‑rich fish three times a week.
- Do 30 minutes of weight‑bearing activity at least three times weekly.
- Schedule a bone density test (DEXA scan) after age60 or earlier if you have risk factors.
- Review medications with your doctor-some drugs (e.g., steroids, proton‑pump inhibitors) can impair calcium balance.
Common Pitfalls and How to Sidestep Them
Relying on one food source. Over‑reliance on milk can lead to excess saturated fat. Mix dairy with fortified plant milks and greens.
Taking mega‑doses of calcium supplements. Doses >1,000mg at once can cause constipation and increase heart‑disease risk. Split doses.
Skipping vitaminD. No matter how much calcium you eat, without vitaminD the body can’t absorb it efficiently. Check serum 25‑OH‑vitaminD annually.
Neglecting resistance training. Cardio alone isn’t enough; muscles pull on bone, signaling it to stay dense.
| Source | Calcium (mg per serving) | VitaminD (IU) | Key Plus |
|---|---|---|---|
| Milk (1cup) | 300 | 100 (fortified) | High‑quality protein |
| Greek yogurt (1cup) | 250 | 80 (fortified) | Probiotics for gut health |
| Fortified soy milk (1cup) | 300 | 120 | Plant‑based, low‑fat |
| Sardines (3oz, with bones) | 350 | 270 (natural) | Omega‑3 fatty acids |
| Calcium citrate supplement (500mg dose) | 500 | 500 (if combined) | Easy on stomach |
Frequently Asked Questions
How much calcium do I need after age 50?
Women 51‑70 need about 1,200mg daily; men the same age need 1,000mg. Above 70, both sexes should aim for 1,200mg.
Can I get enough calcium from a vegan diet?
Yes, by combining fortified plant milks, tofu set with calcium sulfate, leafy greens, almonds, and possibly a calcium‑citrate supplement.
Is calcium carbonate or calcium citrate better for seniors?
Calcium citrate is generally preferable for seniors because it absorbs well without needing stomach acid, which often declines with age.
How often should I get a bone density scan?
If you’re over 60, a DEXA scan every 2‑3years is standard. Earlier testing is advised if you have risk factors like family history of osteoporosis or long‑term steroid use.
Can too much calcium be harmful?
Excessive calcium (>2,500mg/day) can lead to kidney stones, constipation, and may increase cardiovascular risk, especially when taken without vitaminD.




Comments
Calcium absorption declines due to reduced gastric acid production, which is why calcium citrate is often recommended for older adults. The recommended intake aligns with the RDA outlined in the article.
I completely understand how overwhelming these guidelines can feel; it’s a lot to take in at once. Remember that small, consistent changes-like adding a fortified plant milk to your morning cereal-can make a huge difference over time.
While the article touts dairy as the primary calcium source, one must consider that many populations thrive on plant‑based diets, which, when properly fortified, provide comparable calcium levels; moreover, lactose intolerance affects a significant portion of adults, making dairy a less universal solution; therefore, the emphasis on milk may be somewhat myopic.
Typo: “absorbtion” not “absorption”. Also, “vitamin D” should be lowercase d. 👍
Aging may feel like a relentless march toward frailty, but your bones can still stand strong.
The key lies in viewing calcium not as a single hero, but as part of an entire supporting cast.
First, make sure you get at least the recommended daily milligrams of calcium, whether from dairy, fortified alternatives, or leafy greens.
Second, vitamin D acts like the spotlight that lets your body absorb that calcium efficiently.
Third, weight‑bearing exercise sends a signal to bone cells, telling them to stay dense and resilient.
Fourth, regular check‑ups, such as a DEXA scan, give you a clear picture of where you stand.
Fifth, be mindful of medications that can leach calcium, and discuss alternatives with your doctor.
Sixth, spread your calcium intake throughout the day to improve absorption.
Seventh, avoid mega‑doses that can cause kidney stones and cardiovascular strain.
Eighth, stay hydrated, because water helps transport minerals throughout your bloodstream.
Ninth, incorporate foods rich in magnesium and vitamin K, which work hand in hand with calcium.
Tenth, limit excessive caffeine and alcohol, as they can increase calcium loss.
Eleventh, consider a modest supplement only if your diet falls short, and choose calcium citrate for better uptake.
Twelfth, celebrate each small victory-adding a cup of fortified soy milk or a handful of almonds-because consistency beats perfection.
Finally, remember that you are in control, and with these simple steps you can protect your bones and live vibrantly.
Wow, another endless lecture; we get it, you’ve read a textbook. But most of us just need a quick tip, not a novella.
Great summary! If you’re looking for a quick starter, try adding a cup of fortified oat milk to your coffee and take a 10‑minute walk after meals-that’s an easy way to boost both calcium and bone‑stimulating activity.
Just remember to stay consistent.
Consistency is the foundation; even a small daily habit can add up to big bone health gains over the years.
If you slack off, your bones will scream for help!
I dunno why everyone fusses about calcium when you can just eat sardines 😂 but yeah maybe check it out.
Sardines are a solid source, just keep an eye on the sodium and pair them with vitamin‑D rich foods for best absorption.
Absolutely!; however, remember that a balanced diet should include not only calcium‑rich foods; also, vitamin D, magnesium, and regular exercise are essential; don’t rely on a single nutrient alone!