Most red eyes aren’t infections. They’re dryness, allergies, or a bad night’s sleep. But when the usual fixes flop, vitamins can be the missing piece. If you’re trying to figure out whether nutrient gaps are feeding that stubborn flare, here’s a clear, practical guide-what matters, what’s noise, how to test, how to fix, and when to see a doctor. No magic pills. Just honest steps that work.
If you’re sick of waking up to eye redness, this will help you pinpoint if a vitamin issue is part of the problem, or if something else is stealing the show.
TL;DR: Does a vitamin deficiency really cause red eyes?
- Yes, but it’s not the top cause. Vitamin A, riboflavin (B2), niacin (B3), vitamin C, and vitamin D have the strongest links to inflamed or easily irritated eyes. Deficiencies can worsen dryness, fragile vessels, and surface inflammation.
- Redness from vitamins tends to come with other clues: night vision trouble (A), cracked lips/mouth sores and light sensitivity (B2), scaly sun-exposed rash (niacin), easy bruising/bleeding gums (C), and winter low mood/bone aches (D).
- Don’t guess-dose. Rule out common causes first (allergies, dry eye, screens, contact lenses). If redness sticks around 2-4 weeks, ask your GP for labs and a plan.
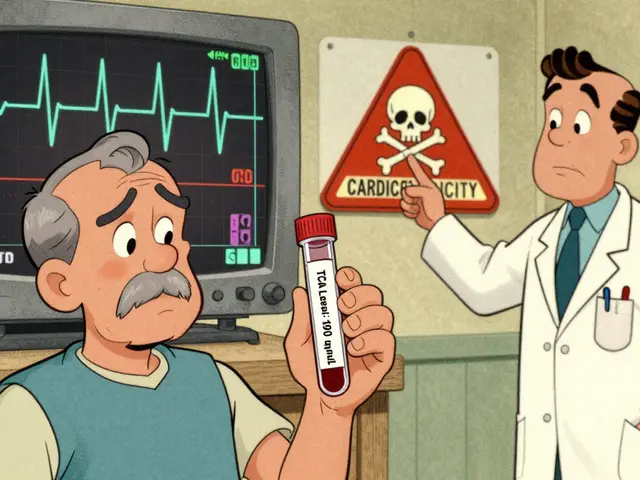
- Food-first works. Supplements help when tests or risks say you need them. Avoid megadoses-vitamin A toxicity is real; high-dose niacin can harm.
- See urgent care fast if redness comes with severe pain, light sensitivity, vision changes, halos around lights, or one eye looks angry out of the blue.
How to figure out if your red eyes are vitamin-related (step-by-step)
I live in Perth, where wind, sun, and ocean spray make dry eyes a local sport. I’ve been there-gritty, red eyes after long laptop days. Here’s the simple process I wish I had sooner.
- Start with the easy wins (7 days):
- Rest your eyes: 20-20-20 rule (every 20 minutes, look 20 feet away for 20 seconds).
- Hydrate and blink more (set a tiny phone reminder if you forget).
- Switch to preservative-free artificial tears, 3-4x/day.
- Skip decongestant drops (they often cause rebound redness).
- Clean eyelids nightly (warm compress + lid wipe), especially if you have flaky lashes.
- Take contacts out earlier; give eyes a break on weekends.
- Scan for vitamin-style clues:
- Night vision seems worse than peers? Dry patches on the whites? Think vitamin A shortage (rare in Australia, but possible with crash diets or malabsorption).
- Cracked mouth corners, sore tongue, light sensitivity? Consider riboflavin (B2).
- Rough, sun-exposed rash on neck/hands, brain fog, gut upsets? Classic niacin (B3) deficiency signs.
- Easy bruising, bleeding gums, slow wound healing? Possibly vitamin C.
- Winter slump, bone or muscle aches, frequent infections? Low vitamin D is common in winter.
- Check your risk profile:
- Diet: low intake of dairy/eggs/leafy greens/orange veg? Heavy ultra-processed foods?
- Lifestyle: heavy alcohol use, smoking, strict vegan without B12 supplement, yo-yo dieting.
- Medical: coeliac disease, inflammatory bowel disease, bariatric surgery, pancreatic issues, chronic antacid use (for B12), orfat-malabsorption.
- Life stage: pregnancy (vitamin A limits!), kids on restrictive diets, older adults with low appetite.
- Season and latitude: less sun means lower vitamin D-yes, even in WA winters if you work indoors.
- Decide on testing (weeks 2-4 if redness persists):
- Ask your GP for: 25(OH)D for vitamin D; plasma ascorbic acid for vitamin C if scurvy signs; B12 and folate if you’re vegan or fatigued; ferritin (iron) if you bruise easily; and general bloods if you feel off.
- Vitamin A and riboflavin tests are uncommon. Your doctor may assess diet and signs instead. Severe vitamin A deficiency is usually obvious clinically.
- Act on results, not hunches:
- Correct with food first, then add the right supplement dose if you’re low or at high risk.
- Recheck labs in 8-12 weeks if you were deficient or borderline.
- Keep the basics: blink breaks, tears, lid hygiene, allergy control.
That’s it. Simple, methodical, and safer than throwing random pills at your eyes.

What else causes red eyes-and how to tell the difference
Vitamins aren’t the usual suspect. These are.
- Dry eye and screens: Burning, sand-in-the-eye feeling, worse by day’s end, improves with blinking or artificial tears. Perth’s wind and air-con don’t help.
- Allergies: Itch is king. Both eyes, stringy mucus, lids look puffy. Often seasonal (spring) or around pets/dust.
- Contact lens overwear: Redness after long wear, discomfort on insertion, sometimes light sensitivity. Take a break and see your optometrist.
- Viral conjunctivitis: Watery, gritty, highly contagious. Often after a cold. One eye, then the other.
- Bacterial conjunctivitis: Thick, sticky discharge, lids glued in the morning.
- Blepharitis/meibomian gland dysfunction: Crusty lashes, flaky skin, lid margin inflammation, morning blur that clears.
- Subconjunctival bleed: A red patch like a paint spill, but no pain. Often from coughing or rubbing. Heals on its own.
- Irritants: Chlorine, smoke, dust, strong winds, makeup or lens solutions you don’t tolerate.
Red flags-don’t wait: Severe pain, vision drop, halos around lights, one very red eye with deep ache (scleritis), trauma, chemical splash, or a contact lens wearer with pain and light sensitivity. That’s same-day care. Acute angle-closure glaucoma and uveitis can be sight-threatening.
Where vitamins fit: deficiencies rarely cause explosive, one-eye emergencies. They more often set the stage-drier surface, fragile vessels, slower healing-so everyday triggers make you red faster and longer.
Food, test numbers, and safe supplement plans (with Australia-specific tips)
Here’s the evidence-backed link between key vitamins and red, irritated eyes-and what to do about it.
Vitamin A: Supports the eye’s surface and tear-making cells. Low A can cause conjunctival dryness (xerosis), Bitot spots, and corneal problems (WHO, 2019). In Australia it’s uncommon unless intake is very poor or absorption is impaired. Don’t megadose-retinol toxicity damages the liver and bone.
Riboflavin (B2): Low B2 can lead to light sensitivity, burning eyes, and a red, vascularized cornea; you might also see mouth cracks and a sore tongue. Fixing diet usually turns this around quickly.
Niacin (B3): Severe deficiency (pellagra) is rare but real; you see dermatitis on sun-exposed skin, gut symptoms, mood and memory issues, and often conjunctivitis and blepharitis.
Vitamin C: Strengthens blood vessels and supports healing. Deficiency leads to fragile vessels and sometimes subconjunctival bleeds. Australia still reports pockets of scurvy in adults with highly restricted diets (Medical Journal of Australia, 2016 case series).
Vitamin D: Not a classic ocular vitamin, but low D is linked with worse dry eye and allergic eye disease in several meta-analyses (2017-2023). Supplementation can help tear stability in some, though results vary. Think of D as an inflammation modifier, not a cure-all.
What about B12 and E? B12 deficiency can show up with neurologic symptoms and fatigue; small studies suggest B12 may help corneal nerve repair in dry eye, but data are limited. Vitamin E has antioxidant roles; clear links to redness are weak. Prioritize A, B2, B3, C, and D first.
| Nutrient | How it relates to red eyes | AU adult RDI/AI | Upper limit (UL) | Useful test & target | Top food sources (typical serve) |
|---|---|---|---|---|---|
| Vitamin A | Maintains ocular surface; deficiency causes dryness, irritation, night vision issues | Men: 900 µg RAE/day; Women: 700 µg RAE/day | 3,000 µg RAE/day (retinol) | Serum retinol; deficiency often <0.7 µmol/L (clinical context matters) | Liver (1 slice), eggs (2), dairy, orange veg (carrots, pumpkin), leafy greens |
| Riboflavin (B2) | Low levels can cause photophobia, burning, corneal vascularization | Men: 1.3 mg/day; Women: 1.1 mg/day | No UL set | Dietary assessment; specialised EGRAC >1.3 suggests low status | Dairy, eggs, lean meats, mushrooms, almonds, fortified cereals |
| Niacin (B3) | Pellagra includes conjunctivitis/blepharitis; eye irritation and redness | Men: 16 mg NE/day; Women: 14 mg NE/day | 35 mg/day (nicotinic acid, to limit flushing) | No routine test; diagnose clinically with diet/history and symptoms | Meat, fish, peanuts, whole grains, fortified breads/cereals |
| Vitamin C | Fragile vessels and poor healing when deficient; can worsen irritation | Adults: 45 mg/day (smokers need +35 mg) | 1,000 mg/day | Plasma ascorbic acid: <11 µmol/L deficient | Citrus, kiwifruit, capsicum, berries, broccoli |
| Vitamin D | Low D linked with worse dry eye/allergy symptoms; modulates inflammation | AI: 5-10 µg/day (200-400 IU), age-dependent | 80 µg/day (≈3,200 IU) | 25(OH)D: ≥50 nmol/L often used as sufficient in AU | Safe sun, oily fish, eggs; supplements if low by test |
Notes: Australian NRVs via NHMRC. Your doctor may individualise targets. Pregnancy requires special caution with vitamin A-avoid high-dose retinol.
Smart supplement rules (Australia, 2025):
- Check the label form: Vitamin A as beta-carotene is safer than high-dose retinol if you’re not deficient. Vitamin D3 (cholecalciferol) tends to raise levels better than D2.
- Stick close to RDI unless you’re confirmed low. Typical correction ranges: Vitamin D3 1,000-2,000 IU/day if your 25(OH)D is below 50 nmol/L; recheck in 8-12 weeks. Vitamin C 200-500 mg/day for a month if your diet is poor; then food-only.
- Niacin: avoid high-dose nicotinic acid unless supervised (flushing, liver risk). Niacinamide (nicotinamide) doesn’t flush but still stick to moderate doses unless prescribed.
- Med interactions: Retinol can interact with isotretinoin; high-dose vitamin C may affect some lab tests; vitamin D can interact with certain diuretics. When in doubt, ask your GP or pharmacist.
- Smokers: skip high-dose beta-carotene supplements-linked with increased lung cancer risk in trials.
What to eat this week (quick, realistic ideas):
- Breakfast: Greek yoghurt with berries and almonds (B2, C). Or eggs on wholegrain toast with sautéed mushrooms (A precursors, B2).
- Lunch: Tuna and capsicum salad with spinach, olive oil, lemon (D, C, A precursors). Veg option: chickpea, pumpkin, and kale salad.
- Dinner: Grilled salmon with roasted carrots and broccoli (A precursors, C, D) or a tofu-veggie stir-fry with brown rice and peanuts (B3, C).
- Snacks: Kiwifruit, mandarins, a handful of nuts, fortified cereal if needed.
I’m not anti-supplement. I’m pro-getting the basics right, then supplement with purpose.

Quick checks, examples, and FAQs to keep you on track
Fast self-checklist (print this):
- My redness improves with artificial tears and breaks (points away from deficiency).
- I have other signs: night vision issues, mouth cracks, sun-exposed rash, bleeding gums, winter aches (points toward deficiency).
- I’m in a risk group: vegan without B12, heavy alcohol use, malabsorption, very low-variety diet, indoor winter lifestyle.
- I can name 5 foods I ate yesterday rich in A/B2/B3/C/D. If not, time to tweak meals.
- I’ve had redness for 2-4 weeks despite basic care → book GP and ask about targeted labs.
Real-world snapshots:
- Desk worker, Perth winter: Dry, red eyes by 4 pm, worse in air-con. Vitamin D came back 37 nmol/L. D3 1,000 IU/day plus tears and blink breaks improved comfort in 3 weeks; lab normalised by 10 weeks.
- Strict diet, little fruit/veg: Red eyes with easy bruising and sore gums. Plasma vitamin C very low. A month of 250 mg/day vitamin C and a produce-heavy shop fixed the gums and toned down redness.
- Cracked mouth corners, light sensitivity: Diet lacked dairy/eggs, few greens. Classic riboflavin picture. Adding dairy or fortified alternatives and eggs cleared symptoms within weeks.
Mini‑FAQ:
- Can red eyes be the only sign of a vitamin deficiency? It’s possible but uncommon. Most true deficiencies show up elsewhere-skin, mouth, energy, vision in the dark.
- How fast will redness improve after fixing a deficiency? Dryness from low A/B2/C can ease within 2-6 weeks once intake improves. Vitamin D effects on tear film can take 6-12 weeks.
- Is vitamin A safe in pregnancy? You need some, but avoid high-dose retinol supplements. Use food sources and prenatal guidance. Talk to your obstetrician before any vitamin A pill.
- Do kids get vitamin-related eye redness? Rare in Australia, but picky eaters can run low on C or B vitamins. See a GP or paediatrician before supplementing.
- What about omega‑3? Not a vitamin, but relevant to dry eye. The 2018 DREAM trial (NEJM) found no benefit over placebo for supplements, yet some people still feel better on a fish-rich diet. Try food first.
- Which drops should I avoid? Decongestant “get the red out” drops often rebound. Use preservative-free lubricants; if allergic, pick an antihistamine-mast cell stabiliser drop as advised by your pharmacist or GP.
- Can I self‑diagnose with online tests? No. Especially for vitamin D and A, labs and clinical context matter. Your GP can order the right tests and read them properly.
Next steps and troubleshooting (pick your scenario):
- Short-term redness after screens/wind/chlorine: Use tears, blink rule, wraparound sunnies outdoors, rinse after the pool. Add a serve of orange veg and leafy greens daily for a month and reassess.
- Persistent redness + mouth cracks or bleeding gums: Book GP. Ask for B-group review and/or vitamin C test. Bring a 3-day food diary.
- Winter indoor worker, low energy: Ask for 25(OH)D. If low, D3 1,000-2,000 IU/day is typical until recheck. Add eggs and oily fish; aim for safe sun as appropriate.
- Contact lens wearer with redness: Stop lenses until cleared. See your optometrist to review fit and hygiene. Vitamin tweaks help, but lens-related inflammation needs direct care.
- Sudden pain, halos, vision changes, or one angry eye: Same-day urgent care-don’t wait for diet changes.
Why you can trust this: The links between vitamin A and the ocular surface are long-established (WHO guidance on xerophthalmia). Riboflavin and niacin deficiency eye findings are textbook nutrition (and still taught for a reason). Vitamin C deficiency shows up in Australian case reports (MJA, 2016). Vitamin D’s role is newer and more nuanced-associations are strong; benefits from supplementation vary, but are reasonable when you’re actually low. For RDIs and limits, clinicians in Australia use NHMRC Nutrient Reference Values. Your GP or optometrist can tailor this to your history and current meds.
I’m not promising that fixing vitamins alone will turn your eyes snow-white. But if you cover the basics and fill the right gaps, you remove the friction that keeps your eyes inflamed. That’s usually where the win lives.
-Harrison, Perth



Comments
OMG this is SO helpful!! 🙌 I’ve been dealing with red eyes for months and thought it was just allergies, but now I’m checking my vitamin D levels tomorrow. Also, the food ideas? Chef’s kiss. 🥑🍊 I’m adding salmon to my meal plan ASAP.
man i’ve been so lazy about my eyes lately. just staring at screens all day like a zombie. but this? this actually made me wanna change. not because it’s ‘science’ but because it feels doable. blink more? yeah. eat an egg? sure. i’m not perfect, but i’m trying. thanks for writing this like a human.
THIS IS A GOVERNMENT COVER-UP. THEY DON’T WANT YOU TO KNOW VITAMIN A IS THE REAL KEY TO EYE HEALTH - BUT THEY’RE PUSHING ‘ARTIFICIAL TEARS’ TO KEEP YOU BUYING PRODUCTS. THE WHO? PROBABLY FUNDED BY BIG PHARMA. I’VE BEEN TAKING 10,000 IU OF RETINOL DAILY FOR 3 YEARS - MY EYES ARE PEARL WHITE. NO DOCTOR WOULD TELL YOU THIS. THEY’RE PAID OFF.
Look, I get it - vitamins are nice, but let’s be real. We live in a world where the air is poison, the water’s got microplastics, and our phones are basically radiation emitters. You think a couple of carrots and a fish oil pill is gonna fix what modern life is doing to our bodies? Nah. This whole guide is just a Band-Aid on a hemorrhage. But hey, at least it’s a pretty Band-Aid. I’ll take my vitamin D, my omega-3, and my existential dread. We’re all just one bad night’s sleep away from becoming a walking symptom.
I appreciate the effort, but you’re still missing the point. Vitamin C deficiency? In 2025? In the U.S.? That’s not just poor nutrition - that’s a moral failure. If you’re eating processed food and calling it a diet, you’re not ‘low on nutrients’ - you’re choosing ignorance. And please, for the love of all that is holy, stop using ‘B2’ like it’s a crypto coin. It’s riboflavin. Say it properly. Also, why are you recommending kiwifruit? That’s expensive. Buy oranges. Or better yet - grow your own.
While the empirical correlations presented are statistically plausible and align with contemporary nutritional epidemiology, one must exercise considerable caution in extrapolating causative relationships from observational data. The conflation of association with intervention efficacy remains a persistent epistemological flaw in public health communication. Furthermore, the recommendation of dietary modification without stratification by genetic polymorphisms (e.g., BCMO1 variants affecting vitamin A conversion) constitutes a reductionist approach to complex physiological systems.
Wait. Wait. Wait. You said ‘vitamin D3 1,000–2,000 IU/day’ - but the UL is 80 µg/day - which is 3,200 IU - so you’re within range - BUT - did you even check the NHMRC guidelines? Because if you’re in Perth, and you’re indoors all winter - and you’re over 50 - then 2,000 IU is barely a maintenance dose - and you didn’t even mention magnesium - which is required for D metabolism - and - oh my god - you didn’t even mention K2 - which directs calcium - and without it - you risk vascular calcification - this guide is dangerously incomplete - and I’m not even mad - I’m just disappointed.
Why are people still falling for this? Vitamins don’t fix red eyes. You’re just giving yourself a placebo because you don’t want to admit you’re addicted to your phone. 😒 I’ve had red eyes for years. Took a week off screens. Gone. Not because of carrots. Because I stopped staring at pixels like a zombie. 🤦♀️
This is actually one of the most balanced guides I’ve read on eye health. I’m from India, where vitamin A deficiency is still common in rural areas, and I’ve seen kids with night blindness. But even here, urban folks are getting dry eyes from screens - and no one connects it to diet. Your food suggestions? Spot on. I’ll share this with my sister who’s vegan and always complains about red eyes. Thank you.
Good stuff. I’m in Dublin, and winter here is basically a vitamin D funeral. I’ve been taking 2000 IU since November. My eyes still get a bit crusty in the morning - but they’re not as red. Still, I blame the rain.
I’ve been reading this whole thing while sipping my chamomile tea, and honestly - I’m emotional. Not because it’s perfect - but because it’s real. I used to think my red eyes were just ‘bad genetics’ - until I started eating more eggs and walking outside at lunch. No supplements. Just food. And sunlight. And breathing. It’s not rocket science - it’s human science. I’ve been telling my coworkers to stop drinking those energy drinks and just eat an apple. They laugh. But one of them just texted me - ‘my eyes don’t burn anymore.’ So yeah. This matters. Not because of the science - but because we forgot how to take care of ourselves. And you reminded us. Thank you.