Every year, thousands of people end up in the hospital-not because their illness got worse, but because they took the wrong pill. It’s not always a mistake by the pharmacist or the doctor. Sometimes, it’s just a quick glance at the bottle, a rushed morning, or the assumption that "this looks right." But here’s the truth: checking your medication label before every dose isn’t just a good idea. It’s the single most effective thing you can do to keep yourself safe.
Think about it. You’ve got a bottle of pills. You’ve taken this exact bottle for weeks. So why bother looking again? Because the label changes. The name might be similar to another pill. The strength might have been adjusted. The refill might say "30" but you only have 12 left. And if you’re on five or more medications-like nearly half of adults over 65-you’re at higher risk. A 2023 study from SmithRx found that people who checked their label before every dose cut their risk of a medication error by 76%. That’s not a small number. That’s life-saving.
What You’re Actually Looking For
You don’t need to be a pharmacist. You just need to know what to check. The FDA’s 2025 labeling standards made it easier. Labels now use larger fonts, clearer contrast, and standardized wording. But you still need to look. Here’s what matters every single time:
- Your full name-Does it match your ID exactly? Even a middle initial mismatch can mean the wrong drug.
- The drug name-Both brand and generic. If it says "Lisinopril" but you thought you were getting "Zestril," they’re the same-but not everyone knows that.
- The dose-Is it 5 mg, 10 mg, or 20 mg? A single number can change everything.
- How often to take it-"Take once daily" is clear. "Take as needed"? That’s trickier. Know the rules.
- Expiration date-Medications don’t last forever. Expired pills can lose potency or even become harmful.
- Warnings-"Avoid alcohol," "Take on empty stomach," "May cause dizziness." These aren’t suggestions. They’re safety rules.
- Pharmacy name and phone number-If something looks off, call them. They’ll confirm it’s right.
That’s it. Seven things. Takes 3 to 5 seconds. But if you skip even one, you’re gambling.
Why Your Memory Fails You
Most people say, "I know what my meds look like." But memory is unreliable. A 2023 study from Dr. Angela Smith’s team at Carolinas HealthCare System found that 83% of patients who relied on memory stopped checking their labels within two weeks. That’s not laziness. That’s how the brain works. Once something feels routine, we stop paying attention.
Here’s a real example: A man in his 70s took insulin every morning. He’d done it for years. One day, his pharmacy switched to a new bottle. The insulin looked almost identical to his saline solution. He grabbed the wrong one. He nearly went into a coma. He didn’t check the label. He thought he knew.
That’s why training isn’t about reminding yourself. It’s about rewiring your behavior.
The Three-Touch Method: How to Make It Stick
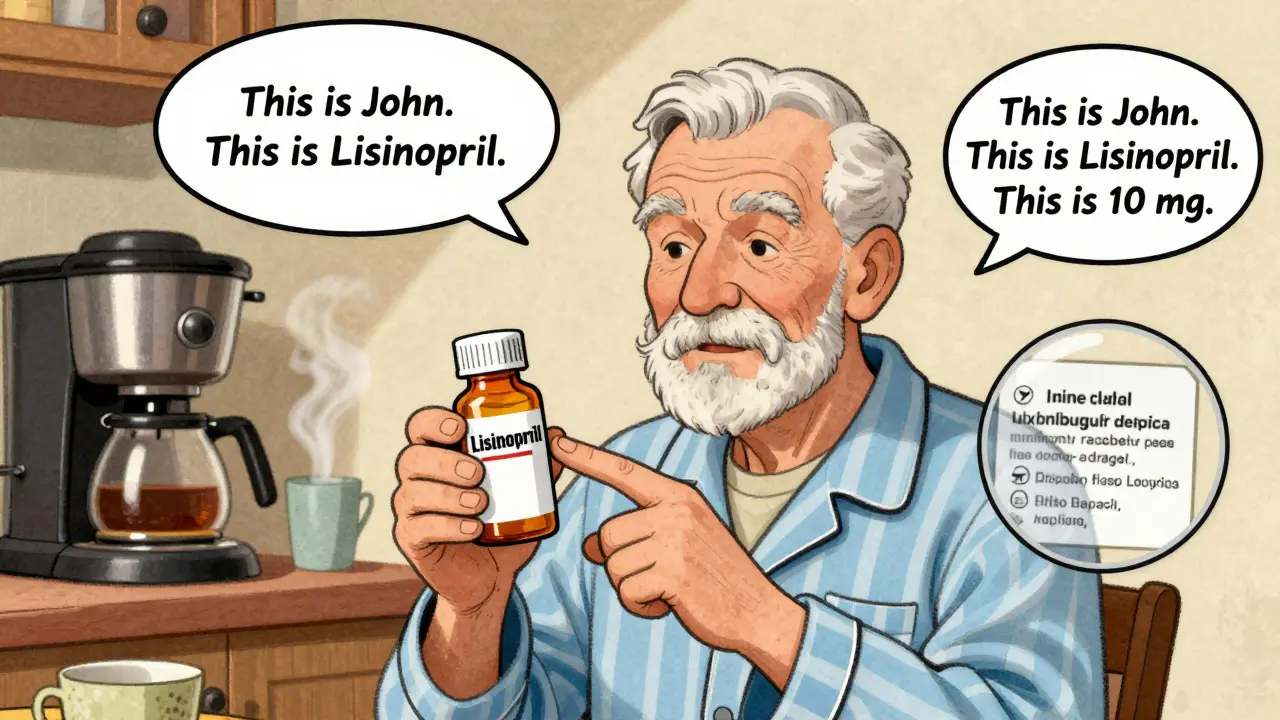
There’s a reason this works: it’s physical. The American Society of Health-System Pharmacists (ASHP) recommends the Three-Touch Method. Here’s how:
- Hold the bottle in your non-dominant hand.
- With your dominant hand, touch the label in three places: your name, the drug name, and the dose.
- As you touch each one, say it out loud: "This is [Your Name]. This is [Drug Name]. This is [Dose] mg."
Why does this work? Because you’re using three senses at once: sight, touch, and sound. A 2023 clinical trial by SmithRx showed that people who used this method had 92% adherence after 30 days. Those who just looked silently? Only 64%.
It feels awkward at first. You might laugh. You might feel silly. But so did brushing your teeth with your non-dominant hand. Eventually, it becomes automatic.

Where to Put Your Meds to Win the Habit
Habits stick when they’re tied to existing routines. You don’t need a fancy app. You need a trigger.
Place your medication bottle right where you do something daily:
- Next to your coffee maker-so you check it before your first sip.
- On your toothbrush holder-so you look at it while brushing.
- By your car keys-so you check before leaving the house.
A 2023 study from MedPak found that people who placed their meds in a high-traffic spot reduced missed checks by 53%. Why? Because you’re not adding a new task. You’re attaching it to something you already do.
And if you take meds at night? Put them next to your bed. Not in the cabinet. Not in the drawer. Right where you’ll see it before you go to sleep.
Tools That Actually Help
Not everyone has perfect vision. Not everyone reads well. Here’s what works:
- Magnifying labels-Stick these on your bottles. They’re cheap, reusable, and increase readability by 38% for people with vision issues.
- Color-coded systems-Use colored stickers or tape: red for morning, blue for night, green for as-needed. 82% of pharmacists recommend this.
- Checklist on the fridge-Write down your meds and doses. Check them off as you take them. Simple. No app needed.
- Teach-back method-Explain your meds to a family member. "This is my blood pressure pill. I take 10 mg every morning." It boosts retention by 57%.
Amazon reviews show that apps with mandatory label verification (you have to scan the barcode before logging the dose) have 63% higher retention than apps that just remind you. Why? Because they force the behavior.

When It Doesn’t Work
This method isn’t magic. It won’t help if:
- Your label is unreadable. If the font is too small or the contrast is poor, ask your pharmacist for a large-print version.
- You have severe memory loss. In that case, you need someone else to help you check.
- You’re overwhelmed with 10+ pills. Talk to your doctor about simplifying your regimen. Sometimes, you can combine doses or switch to once-daily versions.
And if you’re caring for someone else-like an aging parent-don’t just remind them. Do it with them. Sit down. Say it out loud. Touch the label together. Make it a ritual, not a chore.
Why This Matters More Than Ever
In 2025, the average Medicare beneficiary takes 5.1 prescriptions. That’s more than ever. And with more meds comes more risk. The FDA says 25% of errors happen because of name confusion-like mixing up "Lantus" and "Levemir." Both are insulin. One looks like the other. One dose can kill.
The new 2025 labeling standards are helping. Labels now have:
- Minimum 6-point sans-serif font for essential info
- 8-point or larger for warnings
- 70%+ contrast ratio (black on white, not gray on white)
- "High-visibility verification zones"-clear areas you’re meant to check
But none of that matters if you don’t look.
The FDA’s "Check Before You Take" campaign started in January 2024. It’s not a slogan. It’s a rule. And it’s backed by data: 97% of medication safety experts say this practice is essential. Dr. Thomas Davis from Emory University predicts that in five years, checking your label will be as routine as washing your hands.
So start today. Don’t wait for a mistake. Don’t wait for someone to remind you. Pick up your bottle. Touch the label. Say it out loud. Make it a habit. Because the next time you reach for that pill-you want to be sure.
What if I can’t read the label at all?
Ask your pharmacist for a large-print label or an audio label. Many pharmacies now offer audio QR codes you can scan with your phone to hear your medication details. You can also request a caregiver checklist to be placed on your fridge. Never guess-always verify.
Is checking the label enough to prevent all errors?
It’s the most effective single step, but not foolproof. Combine it with a pill organizer for daily doses, a written list of your meds, and regular reviews with your pharmacist. If you’re on five or more medications, schedule a "medication check-up" with your pharmacist every six months.
I use a pill organizer. Do I still need to check the label?
Yes. Pill organizers can be filled wrong. Labels change. A 2023 study found that people who used pill organizers but skipped label checks still had a 42% error rate. Only those who checked the label before filling the organizer cut their risk to under 10%.
What if my pharmacist gives me a different brand?
Generic drugs are safe, but they can look different. Always check the name on the label. If it says "Lisinopril" instead of "Zestril," that’s normal. But if the dose changed from 10 mg to 20 mg without your doctor’s approval, call your pharmacy immediately.
How long does it take to make checking labels a habit?
Most people need 18 to 22 repetitions to make it automatic. That’s about three weeks if you take meds once a day. Use the Three-Touch Method every time. Don’t skip a day. After that, it becomes second nature.



Comments
Let’s be real-this isn’t just about labels. It’s about systemic neglect in healthcare. The FDA’s 2025 standards? A band-aid. The real issue is that pharmacies are still outsourcing labeling to third-party vendors who cut corners to save pennies. I’ve seen bottles where the drug name was printed in 4.5-point font, and the expiration date was smudged. No amount of "three-touch" is going to fix that if the label was designed to be unreadable by design. We need mandatory third-party audits of pharmaceutical packaging-not just recommendations. And while we’re at it, why are we still using paper labels in 2025? NFC chips embedded in bottle caps could auto-sync with your EHR and trigger a voice alert on your phone. Simple. Secure. Scalable.
As someone who’s been on 7 meds for 8 years, I’ve tried everything. The three-touch method? Genius. I started doing it while brushing my teeth-touch, say, repeat. Took me 19 days to stop feeling like a weirdo. Now I do it without thinking. Also, color-coding saved my life. Red for cardiac, blue for neuro, green for PRN. My pharmacist even gave me a custom sticker sheet. No more guessing. No more panic. Just muscle memory. And yeah, I still check the bottle before I pop it into the organizer. Because once, a tech filled my Sunday dose with Tuesday’s pills. I didn’t catch it until I was already halfway to the shower. Scary shit.
OMG YES. 😎 I’ve been screaming this from the rooftops since 2022. My aunt took digoxin instead of diltiazem because the bottles looked identical. She ended up in ICU. The pharmacy? "Oh, sorry, we switched to a new supplier." That’s not an apology-it’s a liability. I now use a QR code scanner app that reads the label and cross-references it with my med list. It beeps if there’s a mismatch. 10/10. Also, I slap neon yellow tape on all my bottles. If you can’t see it from across the room, you’re not trying. And no, I don’t care if it looks like a rave. I’m alive. 💯
I’m from Nigeria, and over here, we don’t have the luxury of FDA-regulated labels. But guess what? We’ve been doing this ritual for decades. My grandma-82, blind in one eye-checks her meds every morning by touch. She runs her fingers over the raised lettering, says the name out loud, and taps the bottle three times. She taught me this. No apps. No stickers. Just discipline. And she’s been on the same meds for 15 years with zero errors. This isn’t a tech solution. It’s a cultural one. We need to stop treating safety like a checklist and start treating it like a sacred practice. The Three-Touch Method? That’s just a Western name for something our grandmothers invented centuries ago.
Let me ask you something. Who really benefits from this "check every label" campaign? Not the patient. Not even the pharmacist. The real winner? The pharmaceutical conglomerates who’ve spent $200 million lobbying for standardized labeling. Why? Because it shifts liability from them to YOU. You think the font size change was about safety? No. It was about legal cover. If you get poisoned because you "didn’t check," then it’s your fault. Not theirs. And don’t get me started on the "Three-Touch Method." It sounds like a cult ritual. What’s next? Bowing to your pill bottle? Singing the drug name in a minor key? This isn’t safety. It’s performative compliance. Real safety? It’s having ONE pill for every condition. One manufacturer. One label. One trusted source. Not seven bottles with seven different fonts and seven different QR codes that lead to five different websites. We’ve been manipulated into believing that vigilance is the solution. It’s not. It’s a distraction from the real problem: consolidation, profit, and systemic opacity.
I love how this post breaks it down so clearly. Honestly, I started doing the three-touch thing after my dad had a near-miss with his blood thinner. We did it together-touch, say it out loud, then put it in his pill box. Now it’s our morning ritual. He says it helps him feel more in control. And honestly? It made me feel less anxious about helping him. I didn’t realize how much fear was tied to just not knowing if he was taking the right thing. The color-coding? Genius. I made a little chart with sticky notes on the fridge. We both check it every night. It’s not about perfection. It’s about presence. And that’s worth more than any app.
Okay, but let’s be honest. How many people actually do this? Like, really? I’ve seen people grab pills while scrolling TikTok. Or take meds in the car. Or just assume the pharmacy didn’t mess up. This whole thing reads like a PSA written by someone who’s never met a real human. The data? Sure. The solutions? Cute. But the reality? Most people don’t care. They’re tired. They’re overwhelmed. They’ve got kids, jobs, bills. You want them to touch three spots on a bottle and say it out loud? Good luck. Meanwhile, the real fix is: fewer meds. Better coordination. Less profit-driven prescribing. But nope. Let’s just make the label bigger and blame the patient. Classic.
It is with profound respect for the dignity of human life that I commend the meticulous and evidence-based approach outlined herein. The integration of multisensory reinforcement-namely, tactile, auditory, and visual modalities-as a behavioral intervention for medication adherence represents a paradigm shift in patient safety protocols. One cannot overstate the empirical significance of the 92% adherence rate observed in the SmithRx trial. Moreover, the strategic anchoring of medication checks to pre-existing daily routines-such as coffee consumption or oral hygiene-exemplifies the principles of behavioral economics as articulated by Thaler and Sunstein. I urge all healthcare providers to institutionalize this protocol as a standard of care. The cost of noncompliance, both in human suffering and fiscal expenditure, is incalculable. Thank you for this vital contribution to public health.