Every year, thousands of people accidentally take two doses of the same medication in one day. It’s not because they’re careless-it’s because life gets busy, routines break down, or multiple people are helping out. One person thinks the pill was taken. Another doesn’t know it was already given. A child refuses medicine in the morning, so it’s tried again at lunch. Before you know it, you’ve doubled the dose-and now you’re worried.
Accidental double-dosing is one of the most common medication errors at home. It doesn’t just happen to seniors. It happens to parents, caregivers, and even healthy adults managing a few prescriptions. The risk? Too high. The U.S. Food and Drug Administration says medication errors cause at least one death every day. Half of all those errors happen in the home. And the worst part? Most of them are completely preventable.
Why Double-Dosing Happens
You think you’re being careful. You take your pills at the same time every day. But then something changes. You’re traveling. A grandkid visits. Your spouse is helping out. You forget if you took your morning dose. You see the pill bottle and think, “I didn’t take that one yet.”
Here’s what actually causes most double-dosing incidents:
- Multiple caregivers giving medication without clear communication
- Using kitchen spoons to measure liquid medicine
- Not knowing two different pills contain the same active ingredient
- Confusion during daylight saving time changes or disrupted routines
- Keeping pills in multiple places-bathroom, kitchen, purse
Children’s Healthcare of Atlanta found that in 41% of pediatric double-dosing cases, a child refused medicine at first, then took it later from another caregiver who didn’t know it had already been given. For older adults, the problem is often memory. A 2023 caregiver survey found 63% of seniors feel anxious about whether they’ve taken their pills-at least once a week. And 28% admitted they’d double-dosed in the past year.
Use a Pill Organizer-But Do It Right
The simplest, most proven tool to stop double-dosing is a pill organizer. Not the fancy kind with alarms. Just a basic one with compartments for each day of the week, and separate slots for morning, afternoon, evening, and bedtime.
WesleyLife’s 2023 survey showed that 68% of seniors use weekly pill organizers. And when used correctly, they reduce double-dosing by 35%. But here’s the catch: it only works if you fill it right.
Don’t just dump all your pills in. Take the time to sort them out. Use a checklist. Write down each medication, dose, and time. Check the label. Is this the same active ingredient as another pill you’re taking? Many people don’t realize that Tylenol, Excedrin, and some cold medicines all contain acetaminophen. Taking two of them means you’re hitting double the dose-and that can damage your liver.
Once filled, place the organizer where you’ll see it every day. Not tucked away in a drawer. Not on the counter where someone else might move it. Put it next to your toothbrush or coffee maker. Make it part of your morning ritual. When you take your pills, you see the empty slot. No guesswork. No doubt.
Track It Digitally-But Don’t Rely on Memory
Smartphone apps like Medisafe have changed the game. In a 2022 study, users who used the app saw an 87% improvement in adherence. These apps send reminders, let you log when you’ve taken a dose, and even notify family members if a dose is missed.
But here’s what most people get wrong: they set up the app once and never look at it again. The magic happens when you use it as a team. If you’re caring for an aging parent, help them set it up. Add your own phone as a notification contact. That way, if they miss a dose, you get a text. If they take it twice, the app flags it.
Even better? Combine the app with a pill organizer. The visual cue from the empty compartment, plus the digital confirmation, cuts double-dosing risk by 62%, according to WesleyLife. It’s not about replacing one tool with another. It’s about layering them.

Never Use Kitchen Spoons for Liquid Medicine
“I just used a teaspoon,” people say. It’s one of the most dangerous myths in home medication safety.
Children’s Healthcare of Atlanta tested kitchen spoons and found their volume varied between 2.5mL and 7.3mL. A standard dose of children’s ibuprofen is 5mL. If you use a spoon that holds 7mL, you’ve given nearly 40% too much. That’s not a little extra. That’s a risk of vomiting, drowsiness, even liver damage.
Always use the syringe or cup that came with the medicine. If you lost it, go to the pharmacy. They’ll give you a new one for free. Never guess. Never improvise. Liquid doses are precise. Your kitchen spoon is not a medical device.
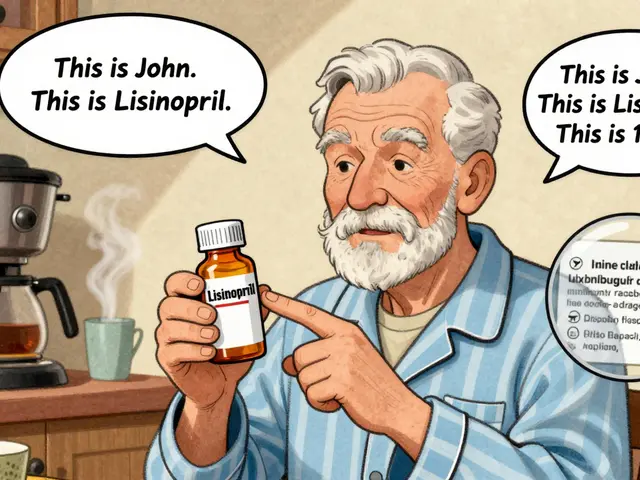
Know What’s in Your Pills
One of the sneakiest causes of double-dosing? Overlapping ingredients.
Let’s say you take a blood pressure pill. Then you get a cold. You grab a cold medicine that says “contains acetaminophen.” You don’t realize your blood pressure pill also has acetaminophen. Now you’re taking two sources of the same drug. Same thing with NSAIDs like ibuprofen. You take one for joint pain. Then you take another for a headache. Two pills. Same active ingredient. Double dose.
Pharmacists at EssexCare Pharmacy say 32% of double-dosing cases they’ve seen in 2023 came from this exact problem. People didn’t know two different brands had the same chemical inside.
Solution? Keep a written list. Include every pill, every vitamin, every supplement-even the ones you only take once a week. Bring it to every doctor’s visit. Ask: “Is this the same as anything else I’m taking?”
Assign One Person to Manage Medications
When multiple people are helping-spouses, kids, visiting relatives-chaos follows.
St. Louis Children’s Hospital found that assigning one person to give all medications cuts double-dosing by 47%. That doesn’t mean that person has to do it alone. It means they’re the one who knows what’s been given, when, and why.
During holidays, when grandparents come over or siblings help out, this becomes even more critical. Children’s Healthcare of Atlanta reported a 33% spike in double-dosing incidents during holiday periods because of uncoordinated care.
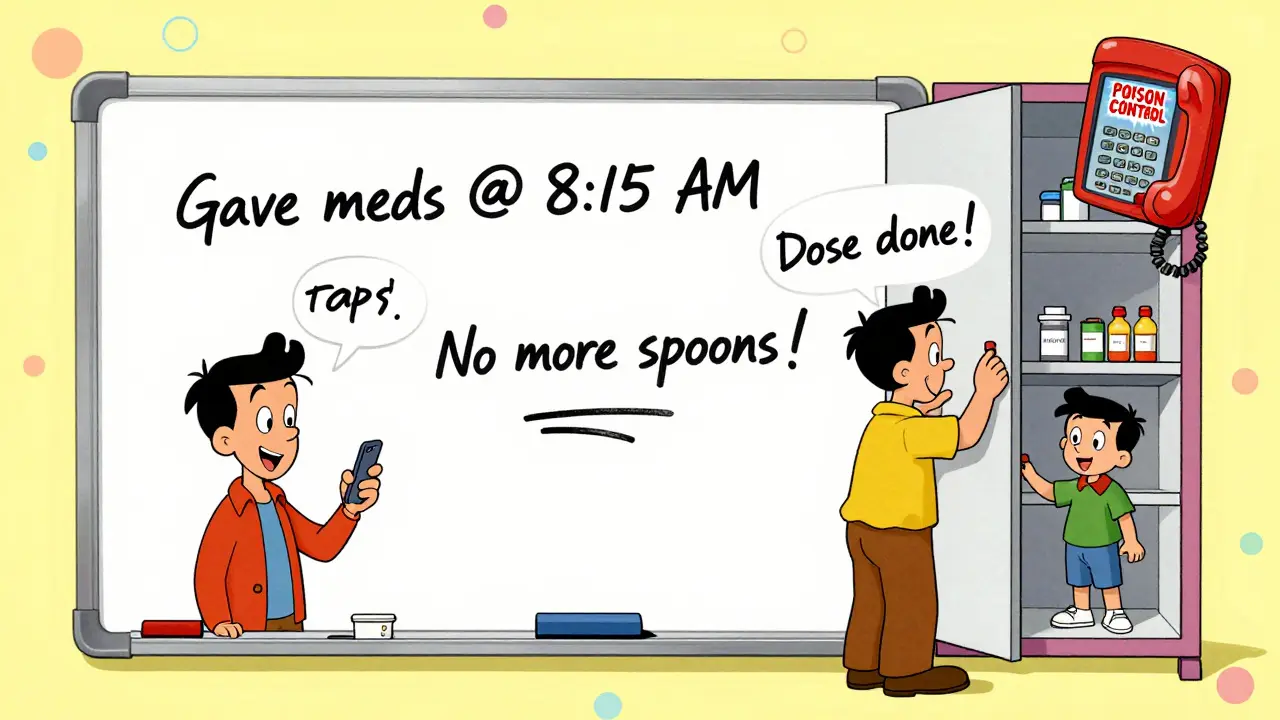
Set up a simple system. A whiteboard on the fridge. A shared note on your phone. A quick text: “Gave morning dose at 8:15.” That’s all it takes to prevent a mistake.
Store Medicines Safely-Out of Reach and Out of Sight
Most people think double-dosing only happens when someone takes too much on purpose. But for kids, it’s often accidental.
Children’s Healthcare of Atlanta says 86% of emergency visits for medicine poisoning in kids involved them getting into medicine belonging to a family member. Not because they were curious. Because it was left on the counter. Because the bottle wasn’t childproof. Because it looked like candy.
Keep all medicines-prescription, OTC, vitamins-in a locked cabinet. Not the bathroom. Humidity ruins pills. Not the kitchen counter. Too easy to grab. A high shelf in a bedroom closet, with a lock if you have toddlers or grandchildren visiting.
And if you’re giving medicine to a child, always lock it up after each use. Even if you think you’ll only be gone for a minute.
What to Do If You Accidentally Double-Dose
Even with all the best systems, mistakes happen. If you realize you’ve taken two doses of the same medicine, don’t panic. But don’t wait either.
Call the Poison Control Center at 1-800-222-1222. They’re staffed 24/7 by nurses and pharmacists who know exactly what to do. Don’t Google it. Don’t wait for symptoms. Call now.
Some medications are safe to double-dose. Others can cause serious harm. Only a professional can tell you which one you’re dealing with.
For children, call immediately. For adults, especially those on blood thinners, diabetes meds, or heart medications, don’t delay.
Make It Stick
Preventing double-dosing isn’t about being perfect. It’s about building habits that work even when you’re tired, distracted, or overwhelmed.
Start with one thing. Pick the biggest risk in your home. Is it liquid medicine? Use the syringe. Is it multiple caregivers? Pick one person to be the point of contact. Is it confusion over pills? Get a pill organizer and fill it together.
Don’t try to fix everything at once. Small changes add up. A weekly pill organizer. A digital reminder. A written list. One person in charge. These aren’t fancy solutions. But they’re the ones backed by data, proven in real homes, and used by hospitals when they discharge patients.
Medication safety isn’t about technology. It’s about clarity. When you know what you’ve taken, when you took it, and why-you stop guessing. And when you stop guessing, you stop risking.




Comments
It's fascinating how something as simple as a pill organizer can dismantle an entire cascade of systemic risk-when you layer visual cues with digital accountability, you're not just managing medication, you're architecting cognitive safety nets. The human brain isn't wired for consistency under stress, and yet we expect it to perform like a pharmaceutical robot. The real innovation here isn't the tool-it's the humility to admit we need external scaffolding to survive our own forgetfulness.
Y'ALL. I work in home care and I’ve seen this a hundred times. One grandma takes her blood pressure med at 8am. Grandkid comes over, sees the bottle, thinks it’s candy-gives it to her again at noon. She doesn’t remember. She’s fine. Until she’s not. Lock the meds. Use the syringe. Write it down. No excuses. This isn’t optional. It’s survival. 🚨💊
One cannot help but observe the tragic irony of modern pharmacology: we have engineered molecules of exquisite precision, yet we entrust their administration to the fickle, distracted, emotionally overloaded Homo sapiens-a creature whose prefrontal cortex was designed to track mammoth migrations, not to manage six different antihypertensives across three time zones. The solution? Not more apps. Not more alarms. But ritual. The sacred act of placing the pill in the palm, the ritual of water, the silence before ingestion-this is where medicine becomes ceremony. And ceremony, unlike technology, remembers.
Per FDA 2023 data, 42% of double-dosing incidents involve polypharmacy patients on ≥5 medications. The real issue isn't adherence-it's pharmacokinetic overlap. Acetaminophen, NSAIDs, and anticoagulants are the top three culprits. Most patients don't realize that 'extra strength' doesn't mean 'extra safe.' You need a med reconciliation protocol at the point of care, not just a whiteboard on the fridge.
this is why u need a pill box with alarms and a qr code that texts ur family if u miss a dose. no cap. my aunt took 2 benzos once and ended up in the er. dont be her.
I love how this post doesn’t just say ‘be careful’-it gives real, doable steps. I’m a nurse in rural India, and we don’t always have fancy apps or pill organizers, but we do have community. We write names on slips of paper, tie them to the bottle, and ask neighbors to check in. Simple. Human. Effective. You don’t need tech to save lives-you just need someone who cares enough to remember for you. 💙
OMG YES. My mom used to keep all her meds in a cereal box on the counter. I found it last year-half the pills were expired, half were crushed, and one was a gummy vitamin she thought was candy. I cried. Then I bought her a lockbox, a pill organizer, and a sticker chart. She’s now got a little ‘medication bingo’ game. She wins a cookie if she gets 7 days right. 🍪✨ We’re not just preventing overdoses-we’re making it fun.
What’s missing here is the emotional component. The guilt people feel after double-dosing is often worse than the physical risk. They don’t need another app-they need permission to be imperfect. The most powerful tool is not the organizer or the app-it’s the conversation. ‘Hey, I think I took that already. Can you check?’ That vulnerability? That’s the real safety net. And it costs nothing.
As a pseudo-philosopher of pharmacological phenomenology, I posit that the pill organizer is not merely a container-it is an ontological anchor in the sea of temporal dislocation. When we disrupt the ritual of ingestion, we fracture the self’s continuity. The digital reminder, then, is not a tool but a prosthetic memory. Yet we fetishize the device while neglecting the intersubjective bond-the caregiver’s gaze, the shared silence before the pill is swallowed. That is where true safety resides.
It is imperative to underscore that the majority of home-based medication errors stem not from negligence, but from the absence of standardized, institutionally sanctioned protocols. The reliance on anecdotal systems-whiteboards, text messages, or familial recall-is a structural failure of the healthcare delivery model. Until such practices are codified into clinical guidelines, we are merely bandaging a systemic hemorrhage.
Let’s be real-this isn’t about pills. It’s about control. We’re terrified of forgetting. So we overcompensate. We stack alarms. We buy organizers. We text our siblings. But the truth? We’re not afraid of the medicine. We’re afraid of being useless. Of being the one who messed up. The real fix isn’t a syringe or a checklist. It’s saying out loud: ‘I need help.’ And letting someone else hold the bottle.