When people talk about generic vaccines, they’re thinking of something simple: cheaper versions of life-saving shots, just like how you can buy a generic version of ibuprofen for a fraction of the price. But vaccines don’t work like that. You can’t just copy a vaccine the way you copy a pill. The reason? Vaccines aren’t chemicals. They’re living systems. They’re made from viruses, cells, proteins, or mRNA - all of which require precise, complex, and fragile manufacturing. And that’s where the real problem begins.
Why there’s no such thing as a true generic vaccine
Unlike regular drugs, which are made of simple molecules and can be replicated exactly, vaccines are biological products. Even two batches from the same factory can vary slightly. That’s why regulators don’t accept the same shortcut used for pills - the Abbreviated New Drug Application (ANDA). For vaccines, every new maker has to prove safety and effectiveness from scratch. There’s no shortcut. You can’t just say, "It’s the same as the original." You have to rebuild the entire process. This isn’t just bureaucracy. It’s science. A vaccine like the mRNA ones from Pfizer or Moderna requires lipid nanoparticles - tiny fat bubbles that protect the genetic code. Only five or seven companies worldwide can make these lipids. If you don’t have access to them, you can’t make the vaccine. Even if you get the recipe, you still need ultra-cold freezers, sterile labs, and trained technicians who know how to handle delicate biological materials. It’s not a factory. It’s a high-precision biology lab.The global vaccine map: who makes what, and who gets left out
India is the unsung hero of global vaccine production. The Serum Institute of India alone churns out 1.5 billion doses a year. It makes 90% of the world’s measles vaccine. It supplies 60% of all vaccines used by the World Health Organization. And it did this for pennies - charging $3 to $4 per dose for the AstraZeneca shot when Western companies charged $15 to $20. But here’s the twist: India doesn’t make vaccines for itself. It makes them for the world. And when India had its own COVID-19 surge in 2021, it stopped exporting. Global supply dropped by half overnight. Meanwhile, Africa, which has 17% of the world’s population, imports 99% of its vaccines. It has zero capacity to make mRNA vaccines. It has no lipid nanoparticle suppliers. It has no cold chain infrastructure to store them. In 2021, 83% of the vaccine doses Africa received through COVAX went to just 10 countries. Twenty-three African nations had vaccinated less than 2% of their people. And yet, Africa is home to over 200 pharmaceutical companies. Most of them make pills - not vaccines. The same pattern shows up in Latin America and Southeast Asia. Countries with strong generic drug industries - like Brazil, Egypt, or Vietnam - still can’t make vaccines. Why? Because the tools, the training, and the raw materials aren’t there. It’s not about skill. It’s about access.The supply chain is a single thread - and it keeps breaking
Vaccine manufacturing isn’t just hard. It’s fragile. Think of it like a Jenga tower. Pull one block out - and the whole thing collapses. During the pandemic, the U.S. banned exports of key raw materials under the Defense Production Act. That included the very lipids needed for mRNA vaccines. India, which relied on China for 70% of its vaccine ingredients, suddenly couldn’t get what it needed. Production slowed. Millions of doses were delayed. This wasn’t a glitch. It was a systemic failure. The world had outsourced vaccine production to a few players - and built a supply chain that depended on political goodwill. Even the WHO’s mRNA technology transfer hub in South Africa, launched with help from BioNTech, took 18 months just to start production. Why? Because they couldn’t find the right machines. The right filters. The right calibration tools. These aren’t off-the-shelf items. They’re custom-built for vaccine production. And the companies that make them? They’re based in Germany, Japan, and the U.S. - and they don’t sell to just anyone.
Costs and profits: why no one wants to build more factories
Building a vaccine plant isn’t like building a smartphone factory. It costs $200 million to $500 million. It takes five to seven years. And once it’s done, you’re locked into producing one type of vaccine. If the next big disease is a different virus? You can’t just retool. You need a whole new plant. Compare that to generic pills. A small factory in India can make 100 different drugs on the same line. The profit margin? Thin, but predictable. With vaccines? You’re gambling. You might make a few billion doses for a global emergency - and then have nothing left to sell. No one wants to invest in that. That’s why the market is so concentrated. Five companies - GSK, Merck, Sanofi, Pfizer, and Johnson & Johnson - control 70% of the global vaccine market. They’re not just big. They’re the only ones who can afford the risk. And they price accordingly. The pneumococcal vaccine, for example, still costs over $10 per dose for low-income countries - even though the cost to produce it is under $1. Gavi, the global vaccine alliance, has been negotiating for years. But the math doesn’t add up.What’s being done - and why it’s not enough
There are efforts to fix this. The WHO’s mRNA hub in South Africa is a start. The African Union wants to get to 60% local vaccine production by 2040. The U.S. FDA is now prioritizing domestic generic drug manufacturing. But these are drops in the ocean. The South Africa hub produces 100 million doses a year. Global demand? Over 11 billion. That’s less than 1%. The African Union’s $4 billion investment plan sounds big - until you realize it’s less than what Pfizer spent on marketing its COVID-19 vaccine in one year. And here’s the real kicker: even if you build the factories, you still need the raw materials. You still need the training. You still need the regulatory approval. And you still need a market that will buy from you. Right now, wealthy countries prefer to buy from established Western firms. They trust them. They’ve been working with them for decades. A new African or Latin American plant? They’re a risk.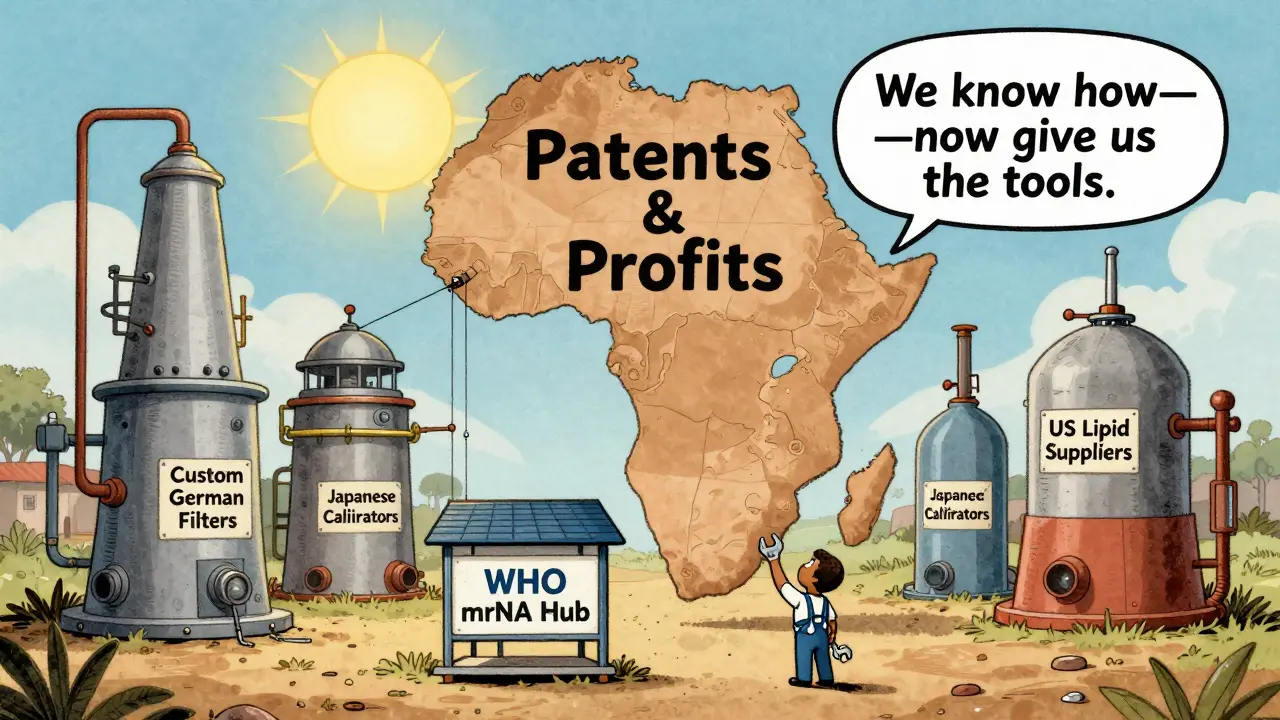
The future isn’t just about making more - it’s about changing the rules
The problem isn’t that we don’t know how to make vaccines. We do. The problem is that the system doesn’t let us make them where they’re needed most. India shows us what’s possible. It has the capacity. It has the expertise. It has the will. But it’s still dependent on foreign suppliers for 70% of its raw materials. If China cuts off exports again? So does India. What we need isn’t just more factories. We need:- A global stockpile of critical vaccine ingredients - not just for emergencies, but for routine use.
- Shared patents and technology, not locked behind corporate walls.
- International funding to build regional manufacturing hubs - not just in Africa, but in Latin America, Southeast Asia, and Eastern Europe.
- Regulatory harmonization - so a vaccine approved in South Africa can be trusted in Nigeria or Senegal without repeating every test.
What’s at stake
This isn’t just about COVID-19. It’s about polio. It’s about measles. It’s about the next disease we haven’t even named yet. If we don’t fix vaccine production now, we’re not just failing the next generation. We’re failing the ones already living in places where a single dose of a vaccine could mean the difference between life and death - and where no one is coming to deliver it.Why can’t we just copy vaccines like we copy pills?
Vaccines are biological products made from living cells, proteins, or mRNA - not simple chemical compounds. Unlike pills, they can’t be proven equivalent through standard tests. Each vaccine must go through a full approval process because even tiny variations in manufacturing can change how the immune system responds. There’s no shortcut like the ANDA process used for generic drugs.
Is India the only country that makes vaccines for the world?
India is the largest producer by volume, supplying 60% of global vaccines used by the WHO and 90% of its measles vaccines. But it’s not alone. Countries like China, South Korea, and Russia also produce large volumes. However, India is unique because it produces high-quality vaccines at low cost for low-income countries - something few others do. Most other manufacturers focus on wealthier markets.
Why don’t more countries build vaccine factories?
Building a vaccine plant costs $200 million to $500 million and takes 5-7 years. The return on investment is uncertain because demand is unpredictable - it spikes during pandemics and drops off after. Plus, the supply chain for raw materials is controlled by just a few global suppliers. Without guaranteed buyers and stable materials, most countries and investors avoid the risk.
Can low-income countries ever become self-sufficient in vaccine production?
Yes - but not without massive international support. The WHO’s mRNA hub in South Africa proved it’s possible to transfer technology. But scaling it requires shared patents, global funding, stable supply chains, and regulatory cooperation. Right now, efforts are too small and too fragmented. Without coordinated global action, most low-income countries will remain dependent on imports for decades.
What happened when India stopped exporting vaccines in 2021?
When India faced its own massive COVID-19 surge, it halted vaccine exports to prioritize domestic needs. This cut global supply by an estimated 50%. Countries relying on Indian-made vaccines - including many in Africa and Latin America - saw delays of months. It exposed how fragile the global system is: one country’s emergency can collapse the entire supply chain.