Imagine this: you pick up your prescription, open the bottle, and the pills look nothing like what you’ve been taking for months. The color is wrong. The shape is off. The label says a completely different drug. Your heart drops. You’re not alone. Every year, 1.5 million people in the U.S. get the wrong medication from a pharmacy. Some of these mistakes are minor. Others can land you in the hospital-or worse.
Stop Taking It Right Away
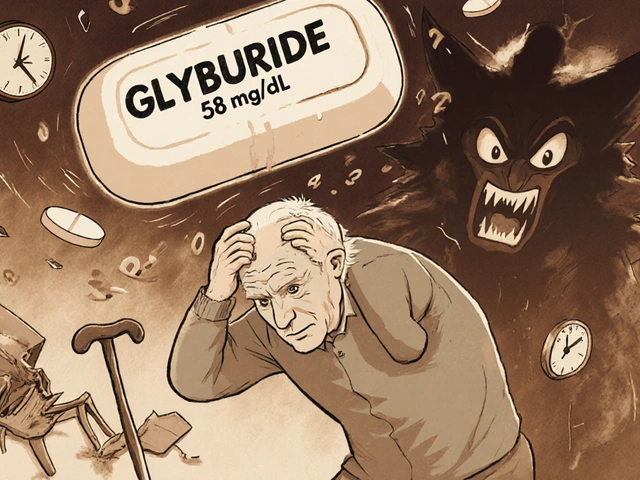
The first thing you must do? Stop taking the medication immediately. Even if you feel fine, don’t assume it’s harmless. Many wrong medications don’t cause instant symptoms, but they can still be dangerous. Taking someone else’s blood pressure pill, for example, could crash your heart rate. Swallowing a diabetes drug when you don’t have diabetes can send your blood sugar into a tailspin. The longer you wait, the more damage you risk.Call Your Doctor Right Now
Don’t wait until your next appointment. Call your prescribing doctor the moment you realize something’s wrong. Tell them exactly what you found: the name on the bottle, what the pill looks like, and how it differs from what you expected. Your doctor might need to:- Prescribe the correct medication right away
- Order blood tests to check for side effects
- Advise you to go to the emergency room
Call the Pharmacy-Talk to the Manager
Don’t just leave a voicemail. Ask to speak with the head pharmacist or store manager. Be calm but clear: “I received the wrong medication. I need to speak with someone in charge.” Ask them to:- Confirm what was supposed to be dispensed
- Explain how the error happened
- Provide a written statement of the incident
Document Everything
Write down every detail while it’s fresh:- The date and time you picked up the prescription
- The name of the pharmacy and the pharmacist you spoke with
- What you thought you were supposed to get
- What you actually received
- When you noticed the mistake
- Any symptoms you experienced
- The wrong medication in the bottle
- The pharmacy label
- The original prescription slip (if you still have it)
- The correct medication (if you later get it)

Report the Error
Pharmacies don’t always fix their systems unless they’re held accountable. Reporting isn’t just about you-it’s about preventing this from happening to someone else. Report to:- The Institute for Safe Medication Practices (ISMP) - They run a confidential national reporting system. Over 100,000 errors have been reported since 1991. You don’t need to give your name.
- Your state’s pharmacy board - Every state has one. In Georgia, you file with the Composite Medical Board and the Attorney General’s Consumer Protection Division. Find yours at the National Association of Boards of Pharmacy website.
- The FDA’s MedWatch program - They collect medication error reports from patients and providers. In 2022 alone, they received over 92,000 reports, 38% from community pharmacies.
Legal Options: What You Can Do
If the wrong medication caused you harm-physical, emotional, or financial-you may have legal rights. Pharmacy errors are considered medical malpractice. You don’t need to be injured badly to act. Even if you only had a few days of dizziness or nausea, you can still pursue compensation for medical bills, lost wages, or pain and suffering. Key legal steps:- Gather evidence - Your documentation, photos, medical records, and pharmacy records.
- Don’t talk to insurance adjusters - If the pharmacy’s insurer calls, say: “I’m consulting a lawyer first.” Never give a recorded statement without legal advice.
- Consult a medical malpractice attorney - Most work on contingency (you pay nothing unless you win). The American Association for Justice says 70% of pharmacy error cases settle out of court.
- Act fast - Statutes of limitations vary by state. In Georgia, you have 2 years from the date you discovered the error. In some states, it’s as short as one year.
Why This Happens-and How Pharmacies Could Prevent It
You might wonder: “How could this happen?” It’s not just human error. It’s a system problem. Common causes include:- Similar-looking or sounding drug names (e.g., hydralazine vs. hydroxyzine)
- High workload during peak hours
- Missing or unclear prescriptions
- Failure to use barcode scanning
What You Can Do to Prevent This Next Time
You can’t control the pharmacy, but you can protect yourself:- Always check your pills - Compare the shape, color, and imprint code to what you’ve taken before. Use apps like Drugs.com or WebMD to look up pill images.
- Ask the pharmacist - “Can you confirm this is the medication my doctor prescribed for my high blood pressure?”
- Use one pharmacy - They can track your history and catch dangerous interactions.
- Keep a current medication list - Include names, doses, and why you take them. Bring it to every appointment.
Long-Term Risks of Ignoring a Pharmacy Error
Even if you feel fine now, the risks don’t disappear. The Journal of the American Medical Association found that patients who experience medication errors have a 28% higher risk of dying within five years. For those who got the wrong heart or blood pressure meds, the risk jumps to 42%. These aren’t just statistics. They’re real people-parents, grandparents, friends-who never got the chance to fix what went wrong because no one told them what to do.Final Thought: You’re Not Overreacting
If you’ve been given the wrong medicine, you’re not being paranoid. You’re being smart. This isn’t a minor mistake. It’s a serious safety failure. Taking action protects your health, your rights, and potentially others’ lives too.Don’t wait. Don’t assume it was a one-time glitch. Document. Report. Act.



Comments
Look, I’ve been on seven different meds in the last three years, and I’ve never once trusted a pharmacy to get it right. I always pull out my phone and cross-check the pill imprint on Drugs.com before I swallow anything. It’s not paranoia-it’s survival. I’ve seen friends end up in the ER because they assumed the bottle looked ‘close enough.’ Don’t be that person. Take five seconds. Save your life.
And yeah, I know the system’s broken. But if you’re waiting for Big Pharma or the FDA to fix it, you’re already dead inside. You’ve got to be your own advocate. No one else will.
I don’t care if you’re busy, tired, or in pain-check the damn pills. It’s not hard. It’s just inconvenient. And inconvenience beats death every time.
Stop taking it. Call your doctor. Save the bottle. Report it. Done. No drama. No hashtags. Just action.
Let’s be brutally honest: this isn’t a ‘pharmacy error’-it’s a systemic collapse of American healthcare infrastructure. We’ve outsourced critical medical functions to profit-driven corporations that treat pharmacists as disposable labor under 12-pill-per-minute quotas. The barcode scanning stat? 62% adoption? That’s not negligence-it’s deliberate underinvestment.
We’re not talking about ‘human error.’ We’re talking about a capitalist structure that externalizes risk onto patients. The VA cut errors by 55%? Because they decoupled care from shareholder returns. The rest of us? We’re collateral damage in a market that values efficiency over human life.
And don’t get me started on the FDA’s MedWatch program. A 38% reporting rate from community pharmacies? That’s not transparency. That’s a public relations stunt. Real accountability requires mandatory public dashboards, real-time error tracking, and criminal liability for repeat offenders. Not ‘reporting’-retribution.
And yes, I’m aware this is a radical stance. But radical times demand radical honesty. If you’re still trusting a CVS pharmacist to catch a hydralazine/hydroxyzine mix-up while they’re on their 14th shift this week, you’re not just naive-you’re complicit.
I can’t even breathe thinking about this. I had this happen to my mom last year-she took a pill that was supposed to be for arthritis but was actually a thyroid med. She didn’t say anything because she didn’t want to ‘cause trouble.’ Then she started shaking at 3 a.m. and I had to rush her to the hospital. She cried for two days after because she felt guilty for ‘making a fuss.’
Why do we make people feel bad for protecting themselves? Why is it seen as ‘confrontational’ to ask, ‘Is this right?’ Why is the burden always on the patient? I’m so tired of being told to ‘be polite’ while my family’s life is on the line.
I’ve started carrying a laminated card in my wallet that says: ‘I am not asking permission. I am verifying my medication. This is non-negotiable.’ I hand it to pharmacists. Some roll their eyes. One cried. I don’t care. My mom is alive because I didn’t let her be silent.
If you’re reading this and you’ve ever felt too scared to speak up-please, just this once-say something. You’re not being difficult. You’re being brave.
Oh wow, another ‘how to not die from a pharmacy’ guide. Groundbreaking. Did you also include ‘don’t drink poison’ and ‘avoid falling off cliffs’? This is like writing a manual on how to not get hit by a bus when you’re walking across the street.
Here’s the real issue: you’re an adult. You’re responsible for your own body. If you can’t verify your own meds, maybe you shouldn’t be allowed to leave the house alone. And why are you using five different pharmacies? You’re literally asking for disaster. Stop being a victim and start being a responsible human.
Also, ‘take photos’? You’re going to sue someone over a pill mix-up? Congrats, you’re now part of the lawsuit economy. Next thing you know, you’ll be suing your toaster for burning your toast.
Just check the damn bottle. That’s it. No videos. No lawyers. No ‘I’m a victim.’ Just use your brain. It’s not that hard. You’re overcomplicating it because you want attention.
And for the love of God, stop tagging the FDA. They’re not your therapist.
Okay, but let’s talk about the psychosocial architecture of medication error trauma. The pill bottle isn’t just a container-it’s a symbolic vessel of trust, and when that trust is violated, it triggers a cascade of epistemic insecurity. You’re not just dealing with a wrong drug-you’re dealing with a rupture in your ontological safety net.
And the documentation? That’s not evidence-it’s performative self-preservation. You’re constructing a narrative arc to legitimize your suffering in a system that pathologizes patient agency.
Also, 92% of successful claims have photographic proof? That’s not a statistic, that’s a cultural artifact of late-stage capitalism’s need for visual validation. You can’t prove harm unless you’ve got a TikTok-ready image.
And the VA’s 55% reduction? That’s not ‘redesigning workflows’-that’s state-funded institutional control. We’re not talking about safety. We’re talking about surveillance capitalism in scrubs.
Also, emojis: 🩺💊📉📉📉 #MedErrorTrauma #PharmacyApocalypse #CheckYourPillsOrDieTrying
I don’t know why people make this so complicated. If the pills look wrong, don’t take them. Call the pharmacy. End of story. Why do we need 12 steps, photos, lawyers, and reports? Just don’t swallow it. That’s the only thing that matters.
Also, I don’t trust anyone who takes meds without reading the label. If you can’t read a pill bottle, you shouldn’t be on pills.
My aunt took the wrong blood thinner once. She didn’t tell anyone because she was scared they’d think she was ‘crazy.’ Two weeks later, she had a stroke. She’s fine now, but she’s terrified to take anything. I made her a little card with the names of all her meds, the correct colors, and the pharmacy’s direct line. I carry a copy too.
People think this is about lawsuits. It’s not. It’s about dignity. You deserve to know what’s in your body. No one should have to beg for the truth.
And yes, I’m telling you this because I care. Not because I want to be right. Just because I’ve been there.
Everyone’s right here. But let’s not turn this into a blame game. Pharmacists are overworked, underpaid, and often the only healthcare professional patients interact with daily. We need better systems, yes-but we also need to support the people trying to fix it.
I work in a pharmacy. I’ve caught my own mistakes before pills left the counter. I’ve stayed late to double-check scripts. I’ve cried because I was scared I’d hurt someone.
So yes, check your pills. Document everything. Report errors. But also, thank the pharmacist when they get it right. Ask them how their day is. A little kindness goes further than a lawsuit.
We’re all trying. Let’s not forget that.