What Is Thyroid Eye Disease?
Thyroid Eye Disease (TED), also called Graves’ orbitopathy, happens when your immune system attacks the tissues around your eyes. It’s not just an eye problem-it’s an autoimmune condition tied to thyroid dysfunction. Most people with TED have Graves’ disease, where the thyroid goes into overdrive and produces too much hormone. About 90% of TED cases happen in people with hyperthyroidism, but it can also show up in those with underactive thyroids or even normal thyroid levels.
It’s rare, affecting roughly 90 to 300 out of every 100,000 people. But when it hits, it changes everything. The inflammation doesn’t just swell your eyelids-it pushes your eyeballs forward, tightens your eye muscles, and messes with your vision. Symptoms often start within six months of a Graves’ diagnosis. And here’s the thing: even if your thyroid levels get controlled, the eye damage can keep getting worse.
Common Symptoms You Can’t Ignore
If your eyes feel like they’re bulging, you’re not imagining it. That’s proptosis, and it’s one of the most visible signs of TED. You might notice people staring at you because your eyes look wide open-even when you’re not paying attention. That’s eyelid retraction. It’s not just cosmetic; it means your eyelids can’t close fully at night, leaving your corneas exposed. Around 45% of patients struggle with this, and 15-20% end up with corneal ulcers if it’s not treated.
Other symptoms are harder to ignore:
- Grainy, gritty, or burning eyes (78% of patients)
- Excessive tearing or dryness (65-80%)
- Light sensitivity (60%)
- Double vision when looking side to side or up and down (50% in moderate to severe cases)
- Pain behind the eyes, especially with movement (40-60%)
- Blurred vision (25-35%)
Some people lose color vision first-this is often the earliest warning of optic nerve compression. In severe cases, which affect about 5% of TED patients, vision loss can happen fast. The disease usually hits both eyes, but one side is almost always worse-by 30-40% in 70% of cases.
How Doctors Diagnose TED
There’s no single test for TED. Diagnosis needs a mix of thyroid checks and eye exams. Your doctor will start with blood tests: TSH, free T4, free T3, and anti-TSHR antibodies. High anti-TSHR levels match up with worse eye symptoms in 75% of cases.
Then comes the eye work. An ophthalmologist will measure your eyelid position, test your vision and color perception, check eye pressure, and scan for swelling. Optical coherence tomography (OCT) shows fluid buildup in the retina. Orbital ultrasound or MRI reveals which eye muscles are enlarged-medial rectus in 90% of cases, inferior rectus in 75%, and so on.
The Clinical Activity Score (CAS) is critical. It counts seven signs of inflammation: redness, swelling, pain with movement, and more. A score of 3 or higher means your disease is still active. If it’s 2 or lower, you’re likely in the inactive phase. Many community doctors skip this score, but academic centers use it to guide treatment. Only 45% of non-academic ophthalmologists track it consistently.
Treatment: From Steroids to Breakthrough Drugs
Before 2020, treatment options were limited. Steroids helped reduce swelling but came with serious side effects-liver damage, high blood sugar, weight gain. Selenium supplements (100 mcg twice daily) showed promise for mild cases, cutting progression to severe disease by 35% in European trials.
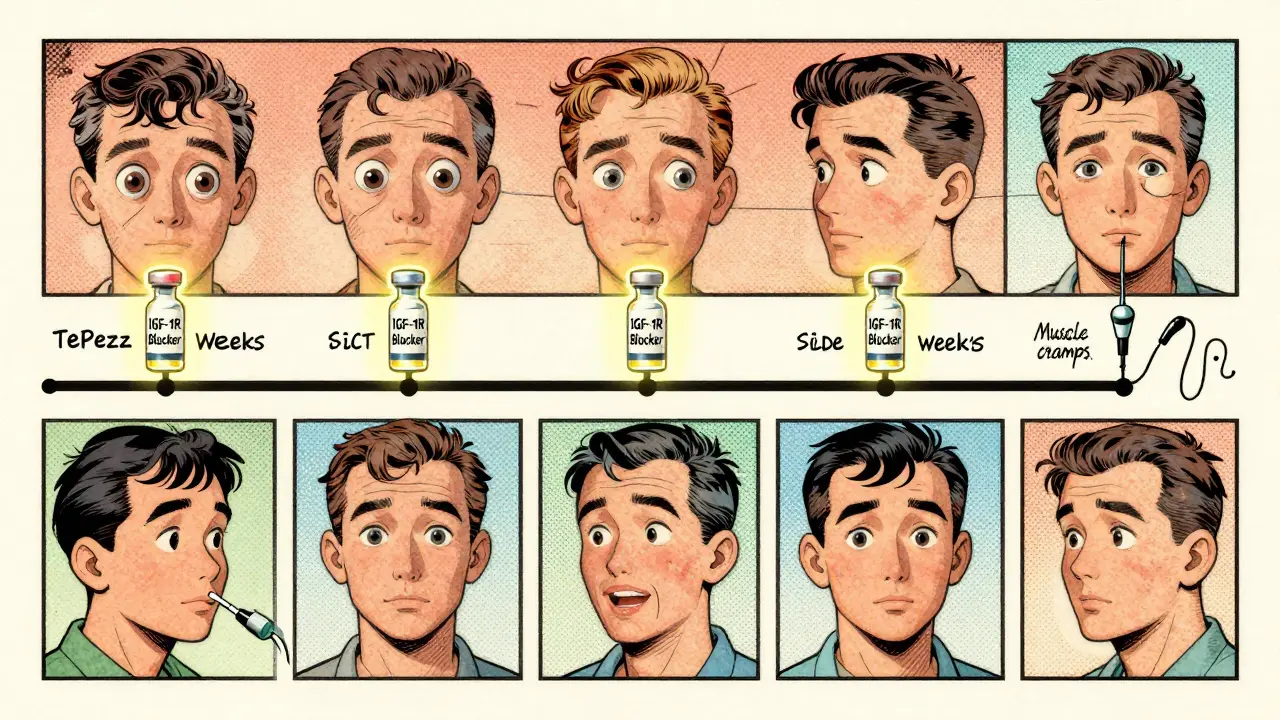
Then came teprotumumab (Tepezza). In January 2020, the FDA approved the first drug made specifically for TED. It blocks the IGF-1R receptor, which drives the inflammation. In clinical trials, 71% of patients saw their eyes retreat by at least 2 millimeters-compared to just 20% on placebo. Double vision improved in 68% of those on Tepezza, versus 29% on placebo.
But it’s expensive. Each infusion costs about $5,500. A full course-eight infusions over 21 weeks-runs close to $44,000. Insurance often denies coverage upfront. About 35% of initial requests get rejected. Still, for moderate to severe cases, it’s a game-changer. The European Group on Graves’ Orbitopathy now recommends it as first-line therapy over steroids.
Surgery: Fixing What Medicine Can’t
Medicine can stop the inflammation, but it can’t undo permanent damage. That’s where surgery comes in. If your eyes are pushed too far forward and you can’t close them, orbital decompression removes bone from the eye socket to create space. This is needed in 5-10% of cases, especially when the optic nerve is squeezed. Today, 65% of these are done with endoscopic methods-less invasive, fewer complications.
After inflammation calms down, you might need strabismus surgery to fix double vision. It works in 30-40% of cases. Eyelid retraction surgery restores natural lid position in 25-35% of patients, with success rates of 75-85% if done at least six months after the disease stabilizes.
Here’s the catch: many people need more than one surgery. About 20% of TED patients go under the knife multiple times, each procedure targeting a different problem-bulging, then double vision, then eyelid position.
The Hidden Toll: Mental Health and Daily Life
TED isn’t just physical. A 2022 survey found 74% of patients had anxiety or depression. Nearly two-thirds said they were embarrassed by their appearance. Over half couldn’t drive at night because of double vision. One in five reported losing a job or being passed over for promotion because of how they looked.
Tepezza helps-but it’s not perfect. On Reddit, 82% of users said their eyes looked better, but 65% got muscle cramps, and 12% noticed hearing loss. The FDA added a warning in 2022 after post-marketing data showed hearing problems in 5.7% of users, up from 1.1% in trials.
Patients often wait months to get diagnosed. Primary care doctors misidentify TED as allergies or sinus infections nearly half the time. The average delay is over six months. By then, damage may already be done.

Why Timing Matters
The window to stop TED from getting worse is narrow. Experts say treatment should start within the first 12 months of symptoms-and ideally within six. During the active phase, inflammation is high, and drugs like Tepezza can reverse damage. Once it goes inactive, the focus shifts to surgery to fix what’s already changed.
Smoking is the biggest risk factor. It increases your chance of getting TED by 7.7 times and doubles the risk of severe disease. Quitting is the single most effective thing you can do-even if you’ve already been diagnosed.
What’s Next for TED Treatment?
Tepezza isn’t the end. A biosimilar version, teprotumumab-trbw, is expected in 2025. Other drugs like rituximab and satralizumab are in late-stage trials. Researchers are also testing vaccines that target the TSHR antibodies before they cause damage. The goal isn’t just to treat symptoms-it’s to stop TED before it starts.
Right now, 68% of TED treatments happen in academic centers. Community doctors manage only mild cases. That’s changing. More hospitals are setting up coordinated TED clinics with endocrinologists and eye specialists working side by side. These clinics cut diagnosis-to-treatment time by 45 days.
What You Can Do Today
- If you have Graves’ disease and your eyes feel weird-see an ophthalmologist within 30 days.
- Track your symptoms: bulging, pain, double vision, dryness. Use apps like TED Tracker to log changes.
- Quit smoking. No exceptions.
- Ask for the Clinical Activity Score. If your doctor doesn’t know it, ask for a referral.
- Don’t wait for vision loss. If you notice color changes or sudden blurring, get emergency care.
TED is complex, but progress is real. What used to be a slow, painful decline is now a treatable condition-with the right timing and the right team.
Can thyroid eye disease go away on its own?
In mild cases, symptoms may stabilize or improve over time, especially if thyroid levels are controlled. But the inflammation doesn’t truly resolve without treatment. Up to 40% of untreated patients are left with permanent changes like bulging eyes, double vision, or eyelid retraction. Early intervention stops progression and improves outcomes.
Is Tepezza covered by insurance?
Coverage varies. Many insurers require prior authorization and often deny initial requests-about 35% of the time. You’ll need documentation proving moderate to severe disease, active inflammation (CAS ≥ 3), and failure of steroid therapy. Appeals are common and often successful with support from your specialist.
Can you get TED without having Graves’ disease?
Yes, but it’s rare. About 10% of TED cases occur in people with normal thyroid levels or hypothyroidism. These patients still have the same autoimmune antibodies attacking eye tissue. The trigger isn’t always an overactive thyroid-it’s the immune system misfiring.
Does stress make thyroid eye disease worse?
Stress doesn’t cause TED, but it can trigger immune flares. High cortisol levels may worsen inflammation in people already predisposed. Managing stress through sleep, exercise, and therapy can help stabilize the condition, especially during the active phase.
How long does Tepezza treatment take?
A full course is eight infusions, given every three weeks-so about 21 weeks total, or just under five months. Most patients start noticing improvement by the fourth infusion. Results are usually visible within 12 weeks, with maximum benefit around week 20-24.
Are there alternatives to Tepezza?
For moderate to severe cases, intravenous steroids are still used, but they’re less effective and carry more risks. Newer drugs like rituximab and satralizumab are in trials and show promise for patients who don’t respond to Tepezza. For mild cases, selenium and eye lubricants are first-line. Surgery is the only option in the inactive phase.
Can children get thyroid eye disease?
Yes. The European Medicines Agency approved Tepezza for patients as young as 12 in June 2023. Pediatric TED is rare but serious. Early treatment prevents long-term damage to vision and facial structure. Children respond similarly to adults, with about 68% showing reduced eye bulging after treatment.
What’s the success rate of eyelid surgery for TED?
When performed after the disease has been inactive for at least six months, eyelid retraction surgery has a 75-85% success rate. Most patients regain natural lid position and can close their eyes fully. Complications like overcorrection or asymmetry occur in about 10-15% of cases and may need revision.




Comments
I had TED last year. Tepezza was a miracle. My eyes stopped bulging after the 3rd infusion. Yeah, the muscle cramps sucked, but I can close my eyes at night now. No more corneal ulcers. Worth every penny.
I just read this and cried 😭 I didn’t know I wasn’t alone. My doctor called it ‘dry eyes’ for 8 months. I felt like I was going crazy. Thank you for writing this. Someone needs to make a documentary.
Honestly? This reads like a pharmaceutical brochure. Everyone’s obsessed with Tepezza but no one talks about how it’s just another profit machine for Big Pharma. You think a 44k drug is ‘breakthrough’? Or just a cash grab disguised as science?
The Clinical Activity Score is the only valid metric. If your clinician isn’t using CAS ≥ 3 as a threshold for intervention, they’re practicing 1990s medicine. Also, selenium is a placebo for mild cases - don’t confuse palliative care with disease-modifying therapy.
Wait - so if you’re hypothyroid and get TED, you still have anti-TSHR antibodies? That’s wild. So it’s not the thyroid level, it’s the receptor misfire? Like your immune system’s just… mad at eyeballs? 🤯
Oh sweetie, you think smoking’s the biggest risk? Honey, it’s the 7-hour workday and 3 cups of coffee while scrolling Reddit at 2am. Your immune system is exhausted. You’re not sick because of Graves - you’re sick because you forgot how to rest.
YOU CAN DO THIS. I was diagnosed 2 years ago. Now I’m hiking again. Tepezza changed my life. Don’t wait. Don’t listen to the doubters. Your vision is worth fighting for. 💪❤️
In Nigeria, we call this 'eye swelling from stress'. No one knows about TED. My cousin lost sight in one eye. No MRI. No Tepezza. Just prayers and herbal paste. This info needs to reach more places.
So let me get this straight - we have a drug that reverses eye bulging but only 45% of community docs even know the CAS score? This isn’t medicine. This is a class war disguised as science. Your access to sight depends on your zip code.
I’m an endo nurse. We’ve had 3 patients on Tepezza this year. Two had insurance denials. One had to sell her car. The third got approved after her husband wrote a 12-page letter with photos of her eyes. It’s not fair. But it’s real.
The FDA warning about hearing loss? That’s buried in the footnotes. No one talks about it. I had tinnitus after infusion #5. My audiologist said it was permanent. You think your eyes are the only thing that matters?
I’ve been thinking… what if TED isn’t autoimmune at all? What if it’s a hidden bioweapon? The timing matches with 5G rollout. The antibodies? Nanotech markers. They’re testing it on women first - look at the stats. 74% anxiety? That’s not stress. That’s surveillance. They want us docile. Tepezza? It’s a distraction. They don’t want you cured. They want you compliant.
I’m a retired ophthalmologist. I’ve seen TED since the '80s. Steroids. Orbital decompression. Bandages. Then… Tepezza. I cried in the clinic. This is the first time in 40 years we’ve had a real, targeted, disease-modifying therapy. Yes, it’s expensive. Yes, access is broken. But the science? It’s beautiful.
The real tragedy isn’t the cost or the delay. It’s that we treat this like a medical oddity instead of a human crisis. People lose jobs. Relationships. Sleep. Identity. We fix the eyeballs but never fix the world that makes them feel like monsters. We need more than drugs. We need compassion.