When you’re sick and prescribed an antibiotic, the last thing you want is for your morning yogurt or glass of milk to undo the whole treatment. Yet millions of people do this every day without realizing it. The problem isn’t that dairy is bad for you - it’s that the calcium in milk, cheese, yogurt, and even fortified plant-based milks can bind to certain antibiotics and stop them from working. This isn’t a myth. It’s chemistry. And it can mean the difference between getting better in a few days or ending up back in the doctor’s office with a stubborn infection.
Why Dairy Interferes With Some Antibiotics
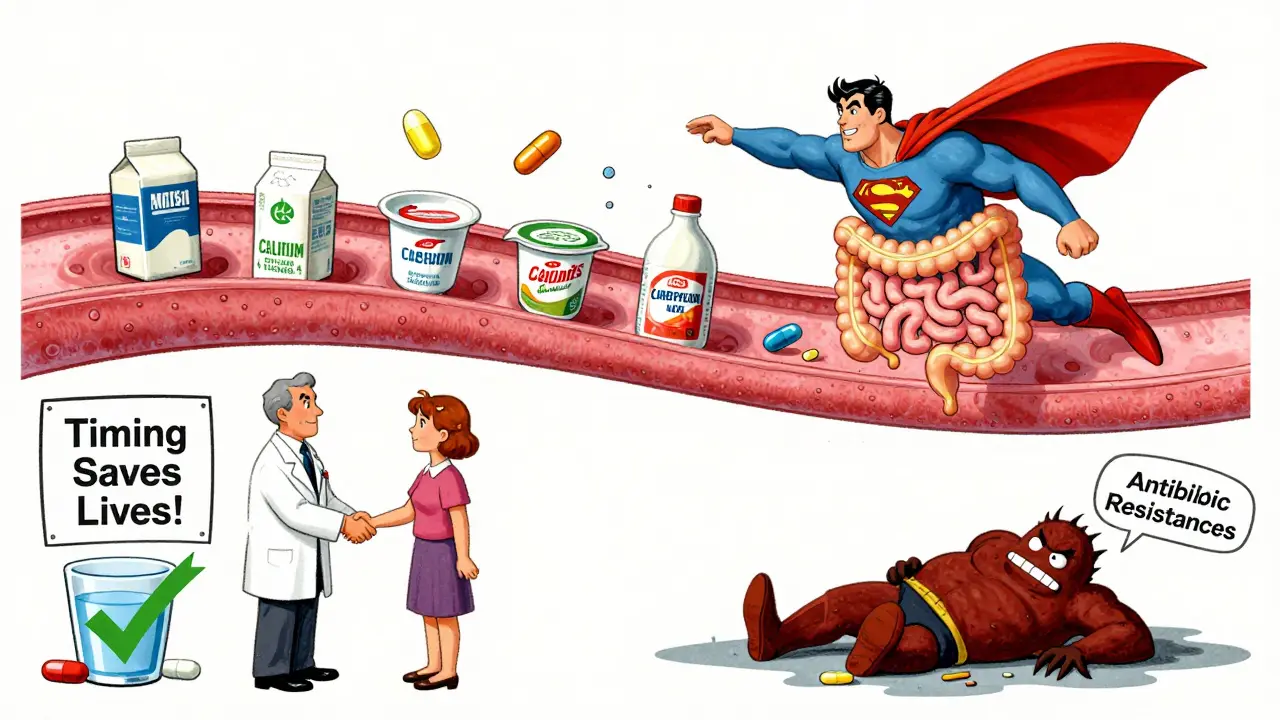
Calcium isn’t just a nutrient - it’s a chemical magnet for certain antibiotics. When you swallow a tetracycline or fluoroquinolone antibiotic with dairy, the calcium ions in milk or yogurt latch onto the drug molecules. This forms a hard, insoluble complex that your gut can’t absorb. Instead of entering your bloodstream to fight the infection, the antibiotic just passes through your system like unused food. This interaction was first documented in the 1960s with tetracycline. Since then, dozens of studies have confirmed it. One 2022 study found that yogurt reduced the absorption of ciprofloxacin by 92%. Milk cut it by 70%. Even a small serving of cheese or a calcium-fortified orange juice can cause the same problem. The effect isn’t minor - it can drop antibiotic levels in your blood by 20% to 92%, depending on the drug and how much dairy you ate.Which Antibiotics Are Affected?
Not all antibiotics are affected. Penicillins, amoxicillin, azithromycin, and most cephalosporins? Fine with dairy. But two major classes are highly sensitive:- Tetracyclines: Includes tetracycline, doxycycline, and minocycline. These are used for acne, Lyme disease, respiratory infections, and some STIs. Tetracycline is the most affected - absorption can drop by up to 90% with dairy. Doxycycline is a bit more forgiving, but still suffers a 50%+ drop if taken with milk.
- Fluoroquinolones: Includes ciprofloxacin, levofloxacin, and moxifloxacin. These are common for UTIs, sinus infections, and pneumonia. Ciprofloxacin is especially vulnerable. A single glass of milk can slash its effectiveness by 70%.
What About Plant-Based Milks?
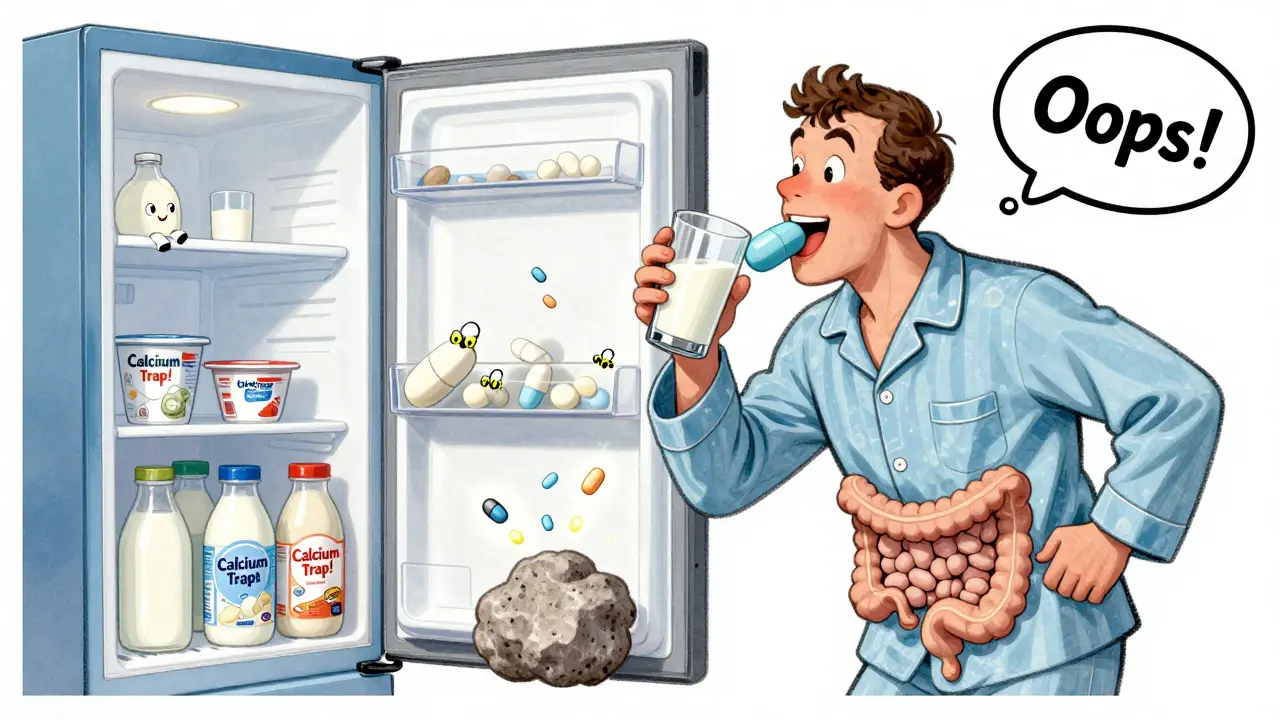
Many people assume almond, oat, or soy milk are safe alternatives. They’re not. Most commercial brands are fortified with calcium - sometimes as much as cow’s milk. A 2023 study in the Journal of the American Pharmacists Association found that calcium-fortified almond milk reduced ciprofloxacin absorption by 85%. Even if the label says “unsweetened,” check the nutrition facts. If it has calcium carbonate or tricalcium phosphate listed, it’s just as risky as dairy.How Long Should You Wait?
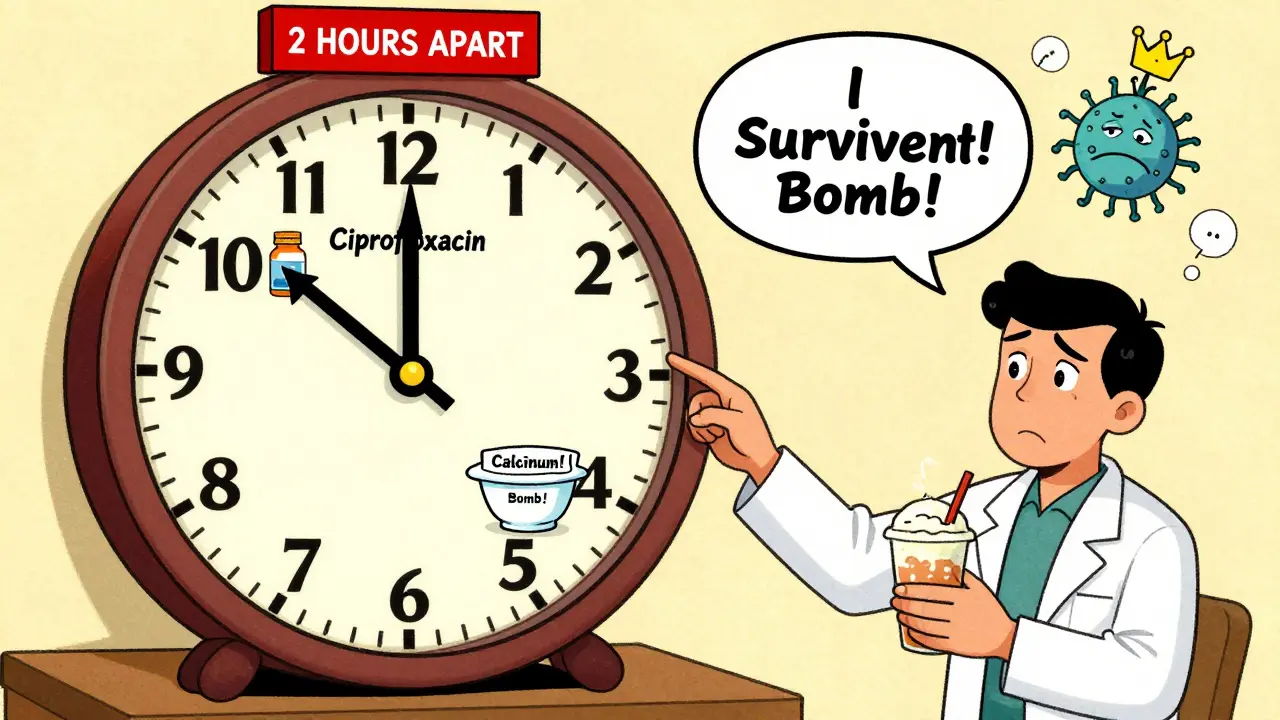
Timing isn’t optional. It’s the only fix. The goal is to keep the antibiotic and calcium apart in your stomach long enough for the drug to be absorbed before the dairy arrives - or after it’s passed through.- For tetracyclines: Take the pill at least 1 hour before eating dairy, or wait 2 hours after. Some experts recommend 3 hours for maximum safety, especially with older tetracycline formulations.
- For fluoroquinolones: Wait 2 hours before and 4 to 6 hours after consuming dairy or calcium-fortified products. Ciprofloxacin is especially sensitive - don’t cut corners.
Real-World Consequences
This isn’t theoretical. In 2022, a survey of 142 patients on HealthUnlocked found that 67% of those who reported antibiotic failure admitted to taking dairy around the same time as their pill. One Reddit user, NurseAmy87, shared a case where a patient on doxycycline for Lyme disease kept getting worse - until her pharmacist asked if she drank milk with her pills. She did. After switching to water and timing her meals, her symptoms cleared within days. A 2023 study in the Journal of Patient Experience tracked 200 people taking ciprofloxacin for UTIs. Those who followed the 2-hour rule had a 98% success rate. Those who didn’t? Only 72% improved. And in cases where the infection didn’t clear, doctors saw signs of early antibiotic resistance - a direct result of sub-therapeutic drug levels.Why Do So Many People Get It Wrong?
You’d think this would be common knowledge. But a 2022 survey by the American Society of Health-System Pharmacists found that 43% of patients received no specific instructions about dairy interactions when they got their prescription. Doctors are busy. Pharmacists aren’t always consulted. Patients assume “avoid dairy” means “don’t drink milk with your pill,” not “don’t have yogurt for breakfast if you take your pill at night.” Even worse, many people don’t realize that calcium supplements, antacids with aluminum or magnesium, and even some iron pills cause the same problem. One patient told her pharmacist she took her ciprofloxacin with her morning vitamins - and didn’t think it mattered because “they’re both pills.”How to Get It Right
Here’s a simple, practical plan:- Check your antibiotic. If it’s a tetracycline or fluoroquinolone, assume dairy interferes until proven otherwise.
- Read the label. New FDA-mandated labels (since January 2023) now include clear timing instructions. Look for phrases like “take 2 hours before or after dairy.”
- Plan your meals. If you take your pill in the morning, have breakfast - including coffee with cream - at least 2 hours later. If you take it at night, avoid late-night snacks with cheese or fortified plant milk.
- Use water. Always take these antibiotics with a full glass of water. Avoid tea, coffee, or juice unless you’re sure it’s calcium-free.
- Use a reminder app. Apps like Medisafe and MyMeds now flag dairy interactions. Input your antibiotic and it’ll remind you when it’s safe to eat yogurt.
What About Newer Antibiotics?
There’s some hope on the horizon. Extended-release versions like Cipro XR were designed to reduce dosing frequency, but they still interact with calcium. Newer tetracycline derivatives are in clinical trials - designed to resist calcium binding. But these won’t be available until 2026 or later. For now, the science hasn’t changed. Calcium still binds. Antibiotics still need to be absorbed. Timing still matters.What If You Forgot?
If you accidentally took your antibiotic with milk or yogurt, don’t panic. Don’t double up. Just wait. If it’s been less than an hour, you might still absorb some of the drug. If it’s been more than an hour, wait until your next scheduled dose and go back to the timing rules. Missing one dose isn’t catastrophic - but doing it repeatedly is.Final Thought: It’s Not About Avoiding Dairy - It’s About Timing
You don’t have to give up cheese, milk, or yogurt forever. You just need to separate them from your antibiotic by a few hours. That’s it. It’s not complicated. But it’s critical. Antibiotic resistance isn’t just about overuse - it’s about under-dosing. And if your pill doesn’t get absorbed because you had a smoothie with it, you’re contributing to the problem. Take your medicine the way it was meant to work. Water. Timing. Patience. Your body will thank you.Can I drink milk with doxycycline?
It’s not recommended. Doxycycline is less affected by dairy than older tetracyclines, but milk can still reduce its absorption by 30% to 50%. To be safe, take doxycycline at least 1 hour before or 2 hours after consuming any dairy products, including yogurt, cheese, or calcium-fortified plant milks.
Does yogurt affect ciprofloxacin more than milk?
Yes. Studies show yogurt reduces ciprofloxacin absorption by up to 92%, compared to 70% for milk. This is likely because yogurt contains higher concentrations of calcium and other ions, plus live cultures that may slow stomach emptying. Avoid yogurt for at least 4 to 6 hours after taking ciprofloxacin.
Are plant-based milks safe with antibiotics?
Only if they’re not fortified with calcium. Most almond, soy, and oat milks are fortified - sometimes with as much calcium as cow’s milk. Always check the nutrition label. If it lists calcium carbonate, tricalcium phosphate, or calcium phosphate, treat it like dairy and avoid it for 2 to 6 hours around your antibiotic dose.
What happens if I take my antibiotic with dairy by accident?
Don’t take another dose. If you realize it within an hour, you might still absorb some of the medication. If it’s been longer, wait until your next scheduled dose and resume your timing schedule. One mistake won’t ruin your treatment, but repeated mistakes can lead to treatment failure or antibiotic resistance.
Can I take calcium supplements with antibiotics?
No. Calcium supplements, antacids with aluminum or magnesium, and iron pills all interfere with tetracyclines and fluoroquinolones. Take them at least 2 hours before or 4 to 6 hours after your antibiotic. Always ask your pharmacist about other supplements you’re taking.
Why don’t doctors always tell patients about this?
Many doctors assume patients will read the label or get advice from the pharmacist. But a 2022 survey found 43% of patients received no specific instructions about dairy interactions. It’s a communication gap - not a medical one. Always ask your pharmacist or doctor: “Can I eat dairy with this antibiotic?”
Is this interaction the same for all antibiotics?
No. Only tetracyclines and fluoroquinolones are strongly affected. Penicillins like amoxicillin, macrolides like azithromycin, and cephalosporins like cephalexin are not impacted by dairy. Always check your specific medication - don’t assume all antibiotics work the same way.


Comments
I took doxycycline with my oat milk latte last week and wondered why my sinus infection didn’t clear up
Turns out my 'healthy' almond milk had calcium carbonate listed right under ingredients
Never again
This is why Western medicine is a joke
You give people pills without teaching them basic biochemistry
Calcium chelation isn't rocket science
But doctors act like it's some ancient secret only pharmacists understand
Meanwhile in India we teach this in high school biology
And you people are still drinking yogurt with ciprofloxacin
Pathetic
My pharmacist told me to avoid dairy with my doxycycline but didn't say anything about oat milk
I've been drinking oat milk with it for months
Guess I'm lucky I didn't get antibiotic resistance
Also why is this not on the bottle
Why do I have to dig through a 10 page PDF to find this
Why is everything so complicated
I just took my cipro with a glass of soy milk and didn't think twice
Now I'm reading this and wondering if I messed up my UTI treatment
Guess I'll stick to water from now on
India has been using natural remedies for centuries
Why do we even need these fancy antibiotics
Our grandmothers used turmeric and neem
Now we're poisoning ourselves with calcium and pills
Western medicine is overrated
It's not merely a matter of calcium chelation-it's a systemic failure of pharmaceutical education, patient communication protocols, and the commodification of healthcare that prioritizes profit over pharmacological integrity
When a patient is handed a prescription for a fluoroquinolone without explicit, unambiguous, written timing instructions regarding calcium-containing substances, it constitutes a breach of the standard of care
The fact that 43% of patients receive zero guidance on this interaction is not negligence-it's malpractice disguised as efficiency
And to suggest that 'timing is simple' is to fundamentally misunderstand human behavior, cognitive load, and the structural inadequacies of primary care delivery systems in the United States
It's not the patient's fault for consuming fortified oat milk-it's the system's fault for failing to provide clear, standardized, and enforceable labeling
Until every antibiotic container includes a color-coded, pictographic warning system with multilingual instructions, this problem will persist, and antibiotic resistance will escalate at an exponential rate
And yes, I've read the FDA guidelines. And no, they're not enough
Who cares
I've taken my antibiotics with milk since I was a kid
Never got sick
Probably just a scam to sell more pills
Also why is everyone so obsessed with plant milks
Just drink cow milk if you want calcium
And if you're worried about antibiotics not working
Maybe you shouldn't be sick in the first place
ok but like… i took my doxy with a protein shake that had calcium phosphate in it and now my skin is breaking out worse than ever
so i went to my dermatologist and she was like ‘did you take it with dairy’
and i was like ‘no i took it with my vegan shake’
she just stared at me
turns out vegan shake = dairy in disguise
so now i take it with water and a sad little banana
and my acne is finally chillin
also why is this not on the box like at all
like come on