Most people don’t feel high cholesterol. No chest pain. No dizziness. No warning sign. It just creeps up-silent, steady, and dangerous. By the time symptoms show up, the damage is often already done. That’s why high cholesterol is called a silent killer. It’s not about feeling bad. It’s about what’s happening inside your arteries right now.
What Exactly Is Hypercholesterolemia?
Hypercholesterolemia is the medical term for having too much cholesterol in your blood. Cholesterol isn’t all bad-it’s needed to build cells, make hormones, and digest food. But when levels get too high, especially the bad kind (LDL), it sticks to your artery walls. Over time, this builds up into plaque. That’s how heart attacks and strokes start.
The numbers matter. Total cholesterol above 200 mg/dL is considered elevated. But the real concern is LDL-low-density lipoprotein. If your LDL is above 190 mg/dL, you’re in the severe range. For most people, doctors aim to get it below 100. If you’ve had a heart attack or have diabetes, they’ll push for even lower-under 70.
There are two main types. One is genetic-familial hypercholesterolemia (FH). The other is lifestyle-driven. FH affects about 1 in 250 people worldwide. If you have it, you’re born with it. Your body can’t clear LDL properly because of a faulty gene, usually in the LDLR or PCSK9 gene. People with FH often have LDL levels over 190 from childhood. Some even have levels above 450. That’s not just high-it’s dangerous.
Familial vs. Lifestyle-Driven High Cholesterol
If your cholesterol is high and your family has a history of early heart disease, don’t ignore it. Familial hypercholesterolemia doesn’t care if you eat salad or run marathons. Even with perfect habits, LDL stays sky-high. That’s why it’s often missed. People assume they’re healthy because they’re active or don’t smoke. But genetics don’t lie.
Physical signs can help spot FH. Look for fatty lumps on tendons-especially the Achilles heel or knuckles. These are called tendon xanthomas. Yellowish patches around the eyelids? That’s xanthelasmas. Both are strong red flags. About 20-40% of people with FH develop these by age 30. If you see them, get tested. Now.
On the other hand, most cases of high cholesterol come from diet, inactivity, or other conditions. Eating too much saturated fat-think fried foods, fatty meats, butter-raises LDL. Being overweight, especially around the waist, does too. So do conditions like hypothyroidism, chronic kidney disease, or type 2 diabetes. About 68% of people with type 2 diabetes also have abnormal cholesterol levels.
The big difference? Lifestyle changes work. Cutting back on saturated fats, adding soluble fiber, and exercising can lower LDL by 10-15%. That’s huge. But for FH? Diet alone won’t cut it. You’ll need medication-often multiple drugs-from day one.
How Is It Diagnosed?
There’s no symptom to follow. No pain to report. The only way to know is a blood test. A lipid panel measures total cholesterol, LDL, HDL (the "good" kind), and triglycerides. You don’t even need to fast anymore. The National Lipid Association says non-fasting tests are just as accurate for screening.
Who should get tested? Everyone over 40. But if you have a family history of early heart disease, or if you’re overweight, diabetic, or smoke, get checked earlier-maybe even in your 20s. The American Heart Association recommends screening every 4-6 years for adults without risk factors. For those with FH or other risks, testing every year or two is common.
Genetic testing is available for FH, especially if LDL is over 190 or there’s a family history of heart attacks before age 55 (men) or 60 (women). It’s not always necessary, but it can confirm the diagnosis and help family members get tested too.
Treatment: It’s Not Just About Statins
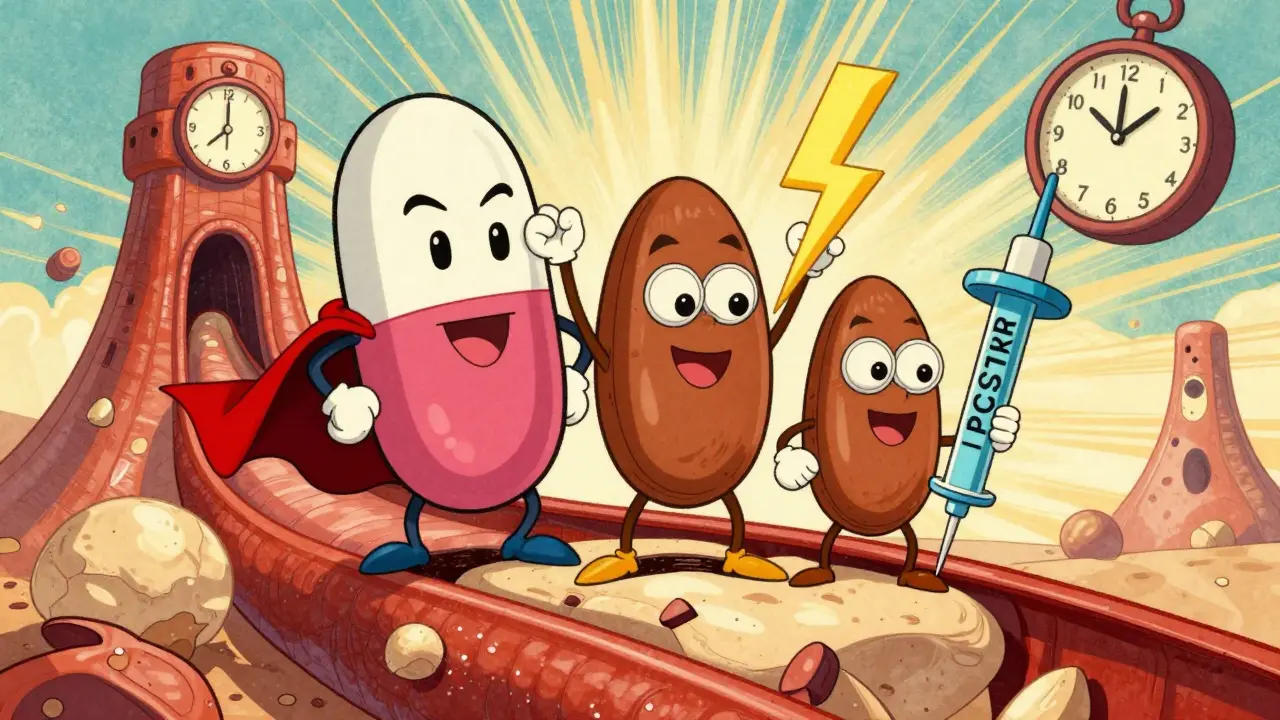
Statins are the first line of defense. Drugs like atorvastatin and rosuvastatin can drop LDL by 50% or more. They’ve been proven to cut heart attacks and strokes by up to 30%. But not everyone tolerates them. Around 7-29% of people have muscle pain or other side effects.
If statins don’t work or aren’t an option, there are alternatives. Ezetimibe blocks cholesterol absorption in the gut. It lowers LDL by about 18% on its own. PCSK9 inhibitors-alirocumab and evolocumab-are injectable drugs that help your liver clear LDL faster. They knock down LDL by 50-60% and are often used in FH patients. These are expensive, but for those with severe FH, they’re life-saving.
Then there’s inclisiran (Leqvio). Approved in 2021, it’s a new kind of drug-a small RNA therapy. You get two shots a year. It lowers LDL by half and stays active for months. No daily pills. No monthly injections. Just twice a year. It’s a game-changer for adherence.
For FH patients, doctors often use triple therapy: a high-dose statin, ezetimibe, and a PCSK9 inhibitor. It’s aggressive, but necessary. Left untreated, heterozygous FH can cut life expectancy by 30 years. The median age for a first heart event? 53 for men, 60 for women.
Why Lifestyle Still Matters-Even With Medication
Some people think, "I’m on a statin, so I can eat whatever I want." That’s a dangerous myth. Medication doesn’t cancel out bad habits. It just helps manage the damage.
The Portfolio Diet, studied in JAMA Cardiology, showed that combining plant sterols, oats, nuts, and soy protein can lower LDL by 30%-almost as much as a low-dose statin. It’s not magic. It’s science. Swap out butter for olive oil. Eat beans instead of steak. Snack on almonds instead of chips. Add a tablespoon of ground flaxseed to your morning yogurt. These small changes add up.
Exercise helps too. Just 30 minutes of brisk walking five days a week can raise HDL and lower triglycerides. It doesn’t need to be intense. Consistency is the key.
And don’t forget weight. Losing just 5-10% of your body weight can significantly improve cholesterol numbers. Even if you’re not "thin," getting healthier matters.
The Real Problem: We’re Not Treating Enough People
Here’s the uncomfortable truth: millions of people with high cholesterol aren’t getting treated. In the U.S., only about 55% of adults who should be on statins are actually taking them. For Black adults, the rate drops to 42%. For women, it’s 49%. Why? Fear of side effects. Confusion over guidelines. Cost. Or just not knowing they’re at risk.
The economic cost is staggering. Cholesterol-related heart disease costs the U.S. $218 billion a year-$142 billion in medical bills, $76 billion in lost productivity. That’s not just numbers. It’s people missing work. Families losing loved ones too soon.
And yet, the tools to fix this exist. We have effective drugs. We have clear guidelines. We know who’s at risk. The gap isn’t science. It’s access. It’s awareness. It’s action.
What You Can Do Right Now
Don’t wait for a heart attack. Don’t wait for a doctor to bring it up. Take control.
- Get your cholesterol checked-no fasting needed.
- If your LDL is above 190, ask about familial hypercholesterolemia.
- If you have a family history of early heart disease, get tested-even if you feel fine.
- Start making small food changes: more vegetables, less processed meat, swap butter for olive oil.
- Move every day. Walk, dance, garden-just get moving.
- If your doctor prescribes a statin or other drug, take it. Don’t stop because you feel fine.
- Ask about inclisiran if you struggle with daily pills.
High cholesterol isn’t a life sentence. But it won’t fix itself. It needs attention. It needs action. And it needs you to care enough to act-before it’s too late.
Can you have high cholesterol and still be thin?
Yes. Cholesterol isn’t just about weight. Genetics play a huge role-especially in familial hypercholesterolemia. Thin people can have LDL levels over 200 mg/dL. That’s why blood tests matter more than appearance.
Does eating eggs raise cholesterol?
For most people, dietary cholesterol from eggs has a small effect on blood levels. The bigger issue is saturated fat-found in bacon, butter, and fried foods. One egg a day is fine for healthy people. But if you have FH or heart disease, talk to your doctor about limits.
Is high cholesterol hereditary?
Yes. Familial hypercholesterolemia is inherited. If one parent has it, each child has a 50% chance of getting it. Even if you don’t have FH, family history increases your risk. If a close relative had a heart attack before age 55 (men) or 60 (women), get tested.
Can you reverse plaque buildup from high cholesterol?
You can’t make plaque disappear completely, but you can stabilize it and slow or even shrink it. Aggressive LDL lowering-with statins, ezetimibe, or PCSK9 inhibitors-has been shown to reduce plaque in arteries. Combined with diet and exercise, it can prevent future heart events.
What’s the difference between HDL and LDL cholesterol?
LDL (low-density lipoprotein) carries cholesterol to your arteries, where it can build up as plaque. That’s why it’s called "bad" cholesterol. HDL (high-density lipoprotein) picks up excess cholesterol and takes it back to the liver to be removed. That’s why it’s "good." But lowering LDL is far more important than raising HDL.
How often should I get my cholesterol checked?
Every 4-6 years if you’re healthy and over 20. If you have risk factors-like high blood pressure, diabetes, smoking, or family history-get tested every year or two. If you’re on medication, your doctor will likely check it every 3-6 months until your levels stabilize.
Are natural supplements like red yeast rice safe for lowering cholesterol?
Red yeast rice contains a compound similar to statins and can lower LDL. But it’s not regulated like prescription drugs. Doses vary, and it can cause the same side effects as statins-muscle pain, liver issues. Don’t use it without talking to your doctor. It’s not a safer alternative-it’s an uncontrolled one.
Can children have high cholesterol?
Yes. Children with familial hypercholesterolemia can have LDL levels over 190 from birth. The American Academy of Pediatrics recommends screening kids with a family history of early heart disease or high cholesterol between ages 2 and 10. Early detection can save lives.





Comments
LDL above 190? Bro, that’s not high, that’s a warning siren with no volume control. I got tested at 28, my doc looked at the numbers and just said ‘you’re not getting off this train.’
It’s eerie how cholesterol doesn’t scream. No pain, no panic-just silent decay. We treat symptoms like they’re the enemy, but this? This is the ghost in the machine. You don’t feel it until the machine stops.
So let me get this straight-you’re telling me I can eat a whole wheel of brie, skip the gym, and still be ‘fine’ if I take my statin? Cool. I’ll just add that to my ‘I’m not dying today’ checklist. 🙃
Just got my lipid panel back-LDL 210. I’m not scared, I’m motivated. 🏃♀️💪 Time to swap my croissant for oats and start walking the dog twice a day. Small steps, big wins!
The notion that ‘non-fasting lipid panels are equally accurate’ is a dangerous oversimplification. The NLA’s position is based on population-level trends, not individual diagnostic precision. To suggest fasting is obsolete is to misunderstand the clinical nuance of triglyceride variability and VLDL dynamics.
I’m from a culture where we eat ghee daily and still live to 90. But I also know my uncle had a heart attack at 47. This isn’t about tradition-it’s about knowing your numbers. My mom got tested at 35 because her dad died young. She’s still here because she listened.
So I’m thin, eat salad, and my LDL is 205? Yeah, I guess my genes really hate me. 😅 But hey-at least I don’t have to explain to my aunt why I didn’t eat her fried chicken.
Ugh, another ‘cholesterol is silent’ post. Like we didn’t already know. But here’s the real issue-people think if they’re ‘active’ or ‘eat clean’ they’re immune. Newsflash: your yoga pants don’t fix your genes. I had a cousin with FH, ran marathons, ate quinoa, died at 42. No one saw it coming. Now her kids are being tested. Too late for her. Don’t be her.
The inclusion of inclisiran as a ‘game-changer’ is misleading. Its cost per QALY exceeds $500,000 in most models. It’s a marvel of biotechnology, yes-but it’s not a public health solution. It’s a luxury for the insured. Let’s not romanticize pharmaceutical innovation while millions go untreated.
My doc put me on a statin last year. Had muscle pain for a week, switched to ezetimibe. No pain, LDL down 25%. Not magic, but it works. Also started eating almonds instead of chips. I still eat pizza. But now I eat it with a side of broccoli. Progress, not perfection.
Bro, I’m 26, skinny, run 5k every morning, and my LDL is 220. My dad had a stent at 45. So I started eating flaxseed, took a PCSK9 test, and now I’m on inclisiran. Two shots a year? Yes please. My mom cried when she saw my results. We’re finally getting ahead of this.