Head Surgery Urinary Frequency Tracker
Symptom Overview
After head surgery, increased urination can occur due to disrupted brain-bladder communication. Track your pattern to help identify triggers and causes.
Your Tracking Log
Track your symptoms to see patterns over time.
Common Triggers After Head Surgery
Neurological Causes
Disrupted brain pathways controlling bladder function can lead to overactivity or underactivity of the detrusor muscle.
Hormonal Changes
Alterations in pituitary hormone regulation (especially ADH) can affect urine concentration and volume.
Medication Side Effects
Opioids, diuretics, and some antibiotics may increase urine production or irritate the bladder.
Stress & Recovery
Physical and emotional stress from surgery can impact autonomic nervous system function.
Red Flag Symptoms
Imagine waking up after a serious operation on your skull and finding the bathroom light on more often than the bedroom lamp. That was my reality for months after a head surgery (a procedure that involves opening the skull to treat injury or disease). The constant urge to pee felt like a prank the doctors never warned me about, and I started wondering whether my brain was sending the wrong signals.
TL;DR
- Frequent urination can follow urination after head injury due to nerve disruption, hormone shifts, or medication side‑effects.
- Common medical causes include neurogenic bladder, pituitary dysfunction, and changes in cerebral spinal fluid pressure.
- Track fluid intake, voiding times, and symptom triggers to give your doctor useful data.
- Seek medical help if you notice sudden volume changes, pain, fever, or loss of control.
- Self‑care tools-bladder training, pelvic floor exercises, and adjusted hydration-can reduce the frequency while you wait for a definitive diagnosis.
What does “increased urination” actually mean?
In medical terms, urinary frequency (the need to void more often than usual, typically more than eight times in 24hours) can be harmless or a sign of something deeper. After a head trauma (any injury that jars or penetrates the skull, ranging from mild concussion to severe fracture), the brain’s control over the bladder can be temporarily thrown off. The symptom isn’t just “going to the loo a lot”-it’s the brain’s way of saying the communication line between the cortex, brainstem, and pelvic nerves has been disturbed.
Why does the brain affect the bladder?
Two main pathways link the head to the bathroom:
- Neurogenic bladder (a bladder that doesn’t empty or store urine properly because of nerve damage). When nerves in the spinal cord or brainstem are impacted, the signals that tell the bladder to hold or release urine get scrambled.
- Hormonal swings, especially involving the pituitary gland (the master endocrine organ sitting at the base of the brain). After a head injury, the pituitary can release too much antidiuretic hormone (ADH) or, paradoxically, not enough of it, leading to either water retention or excess urine production.
Another, often overlooked, factor is the pressure of cerebral spinal fluid (the clear liquid that cushions the brain and spinal cord). Swelling or a slight blockage can change the way the brain’s autonomic centers regulate bladder function.
Medical explanations that popped up in my work‑up
When I finally mentioned the symptom to my neurosurgeon, they ordered a battery of tests. Here’s what they looked for:
- Post‑concussion syndrome - lingering headaches, dizziness, and sleep issues that can also involve autonomic dysregulation.
- Pituitary hormone panel - to see if ADH, cortisol, or thyroid hormones were out of balance.
- Urodynamic study - a specialized test that measures bladder pressure, capacity, and flow.
- CT or MRI - to rule out residual swelling that might press on the brainstem.
In my case, the urodynamics showed a mildly overactive detrusor muscle (the bladder’s contractile muscle) - a classic sign of neurogenic bladder. Hormone levels were within normal range, but the brain imaging still showed a thin line of edema near the area that controls autonomic functions.
How to track the symptom yourself
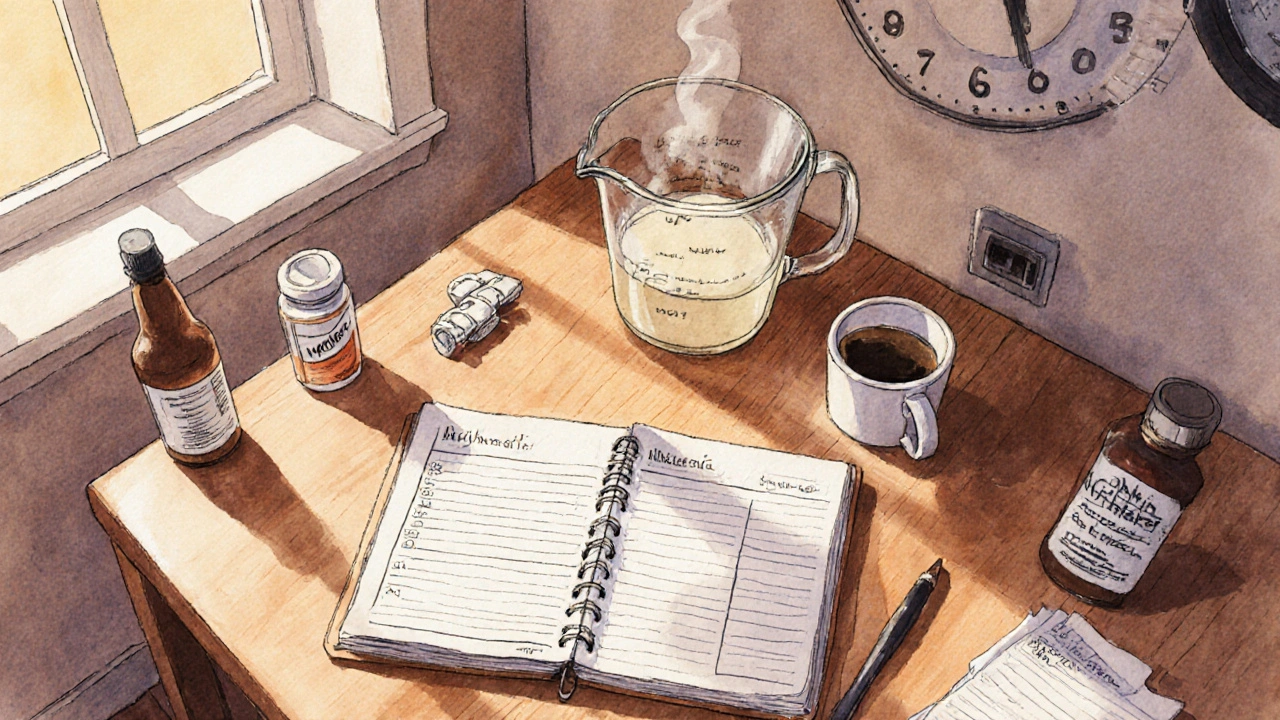
Doctors love data. While waiting for appointments, I started a simple log:
- Note the time of every void.
- Record the volume (I used a measuring jug at home).
- Mark fluid intake - type of drink, amount, and time.
- Highlight moments of stress, medication changes, or new physical activity.
After two weeks, the pattern was clear: caffeine in the late afternoon and a new painkiller both spiked the frequency. The log turned the conversation from “I’m just peeing a lot” to “I’ve had 13 voids between 8am and 6pm, averaging 150ml each, after taking 400mg of ibuprofen.” That concrete info helped the urologist tailor a treatment plan.
When to call a doctor - red‑flag signs
Most of the time, the symptom is annoying but not dangerous. However, look out for these warning signs:
- Sudden increase in volume (more than 2liters in 24hours) - could point to diabetes insipidus.
- Blood in the urine or a burning sensation - possible infection.
- Fever, chills, or flank pain - could be a kidney issue.
- Loss of bladder control (incontinence) or difficulty starting urination - may indicate worsening nerve damage.
- Severe headache, nausea, or visual changes alongside the urinary change - could signal increased intracranial pressure.
If any of these appear, seek medical attention immediately.
Managing the symptom while you wait
My doctor suggested a three‑pronged approach:
- Bladder training - setting scheduled bathroom trips every two to three hours, even if you don’t feel the urge. Over time, the bladder stretches and the urgency fades.
- Pelvic floor therapy - a therapist taught me how to contract the muscles that support the urethra, giving me a bit more control over the flow.
- Medication adjustment - swapping a high‑dose opioid for a milder analgesic reduced the urinary side‑effect.
In addition, I tweaked my hydration: sipping water steadily throughout the day instead of gulping large amounts, and limiting caffeine after 2pm. Those simple tweaks shaved off three to four trips per day within a month.
My personal timeline - the road from confusion to control
Week 0-2 (post‑op): Bed rest, IV fluids, and the first wave of urgency. I thought it was “normal” after surgery.
Week 3-4: The trips became a nightly routine. I started a paper log and noticed the link to coffee.
Week 5: Consulted the neurosurgeon, got referrals to a urologist and a pelvic floor therapist.
Week 6-8: Urodynamic test confirmed an overactive detrusor. Began bladder training schedule.
Month 3: Frequency down to 8-9 times a day, volume up to 250ml per void. Still occasional night trips, but manageable.
Month 6: Full return to work, occasional “just‑in‑case” bathroom dash, but no longer anxiety‑driven.
Takeaway checklist
- Log every void (+ volume) and fluid intake for at least one week.
- Identify and cut down bladder‑irritating triggers (caffeine, certain meds).
- Ask your doctor for urodynamic testing if the frequency persists beyond 4-6 weeks.
- Consider bladder training and pelvic floor therapy as non‑drug first steps.
- Never ignore red‑flag symptoms - act fast.

Frequently Asked Questions
Why does head trauma cause me to pee more?
The brain coordinates bladder storage and release through nerves in the brainstem. Trauma or surgery can disrupt those pathways, leading to an overactive bladder or hormonal imbalances that increase urine production.
Is frequent urination after brain surgery normal?
A mild increase is common during recovery, especially while on pain medication. However, if it persists beyond a month or is accompanied by pain, blood, or fever, you should get evaluated.
Can medications cause this symptom?
Yes. Opioids, certain diuretics, and some antibiotics can increase urine output or irritate the bladder. Talk to your prescriber about alternatives.
What tests confirm a neurogenic bladder?
A urodynamic study measures bladder pressure and flow. Imaging (MRI/CT) can rule out structural causes, and a hormone panel checks for pituitary issues.
Do pelvic floor exercises actually help?
For many patients, strengthening the pelvic floor provides better control over urinary urgency and reduces leakage, especially when the bladder’s signaling is erratic.





Comments
Sounds tough, hope you feel better soon 😊
Frequent urination after cranial procedures often points to a neurogenic bladder, where the brain‑to‑bladder signaling gets scrambled. In many cases, the detrusor muscle becomes over‑active, prompting the urgency you described. Hormonal fluctuations-especially ADH imbalances-can also increase urine output, compounding the problem. Medication side‑effects, particularly from opioids, tend to irritate the bladder lining and raise voiding frequency. Tracking fluid intake, void volume, and trigger events, as you’ve begun, provides physicians with the data needed to tailor interventions.
Yo, you’re not alone in this bathroom marathon! Lots of folks after brain ops end up doing the same dance with the loo. Keep logging those numbers like a pro-trust me, the docs love the stats. When you start tweaking caffeine and meds, you’ll see those trips drop. Hang in there, you’ve got this!
That explanation about the detrusor muscle really clicks with what I’ve read-over‑activity can be a direct result of disrupted neural pathways. It also makes sense why caffeine was a big trigger for you; it’s a known bladder irritant. Adjusting the timing of your pain meds can shave off a few voids a day too. Good luck with the pelvic floor work!
First off, massive kudos for turning a super uncomfortable situation into a data‑driven recovery plan! 🙌 Tracking every ounce of fluid and each little pee might feel like an annoying chore, but it’s actually the golden ticket to pinpointing what’s driving the over‑activity. When you logged that late‑afternoon coffee spike, you uncovered a clear culprit-caffeine is a notorious bladder irritant that can double the urge to go. Swapping that cup for a herbal tea can instantly calm the bladder’s protest. 📊
Medications are another heavyweight in this arena. Opioids, while essential for post‑surgical pain, bind to receptors that can mess with the autonomic nervous system, nudging the bladder into over‑drive. Your switch to a milder analgesic was a smart move; many patients see a 20‑30% drop in void frequency after that change.
Hormonal balance, especially ADH from the pituitary, plays an under‑appreciated role. Even if your labs were "normal," the brain’s stress response can cause subtle swings that tip the water‑retention scales. Hydrating steadily throughout the day-think small sips rather than big gulps-helps keep ADH levels steadier and reduces those sudden surges of urine.
Pelvic floor therapy is often the unsung hero in neurogenic bladder rehab. Those muscles act like a supportive sling, giving you a little extra control when the brain’s signals are fuzzy. Consistent, therapist‑guided exercises can strengthen that sling, leading to fewer “just‑in‑case” bathroom dashes.
Bladder training, the third pillar, is all about resetting the brain‑bladder dialogue. By setting scheduled bathroom trips every two to three hours, you teach the bladder to hold more and signal less often. Over weeks, this can stretch capacity and dampen urgency.
One thing to watch: red‑flag symptoms like sudden spikes over 2 liters a day, blood in the urine, or new headaches. Those aren’t just annoyances; they signal that something deeper might be brewing, and you’d want a doctor to jump in fast.
Bottom line: your systematic log turned a vague complaint into a clear roadmap. Keep the habit alive, keep tweaking triggers, and you’ll likely shave off more trips as you move forward. You’re already at 8‑9 voids a day; that’s solid progress from the 13‑plus you started with. Stay patient, stay data‑curious, and celebrate each small win. 🎉
Your thorough rundown really highlights the interplay between mind and body after neurosurgery. It’s fascinating how a simple habit like sipping water can recalibrate hormonal signals and ease the bladder’s distress. The notion of “training” the bladder mirrors how we can rewire neural pathways through consistent practice-a very philosophical insight. When patients see their own data, the abstract medical jargon becomes tangible, empowering them to participate actively in recovery. In essence, your experience underscores the power of self‑observational science in healing.
They probably hide the real cause on purpose.
Your post is just attention seeking.
While the tone might feel a bit dramatic, sharing personal health struggles can genuinely help others facing similar issues. Dismissing it as “attention seeking” overlooks the usefulness of real‑world data for patients and clinicians alike.
I appreciate the detailed breakdown of possible causes and the practical tips. The emphasis on logging and monitoring is especially valuable for anyone navigating post‑operative recovery. Keep it up.
In many countries with universal health systems, patients receive coordinated post‑operative monitoring that includes bladder function assessments, reducing the need for individual data tracking. It is commendable that you took initiative, yet a more streamlined, state‑run approach could have mitigated much of this inconvenience.