What if your pain isn’t telling you that something’s broken?
For years, we’ve been taught that pain equals damage. If your back hurts, there must be a herniated disc. If your knee aches, the cartilage is worn out. This idea seems logical - and it’s been the foundation of medical advice for decades. But here’s the twist: pain neuroscience education shows us that pain is not a direct line from injury to suffering. It’s a complex output of your brain, shaped by thoughts, emotions, memories, and even how safe you feel.
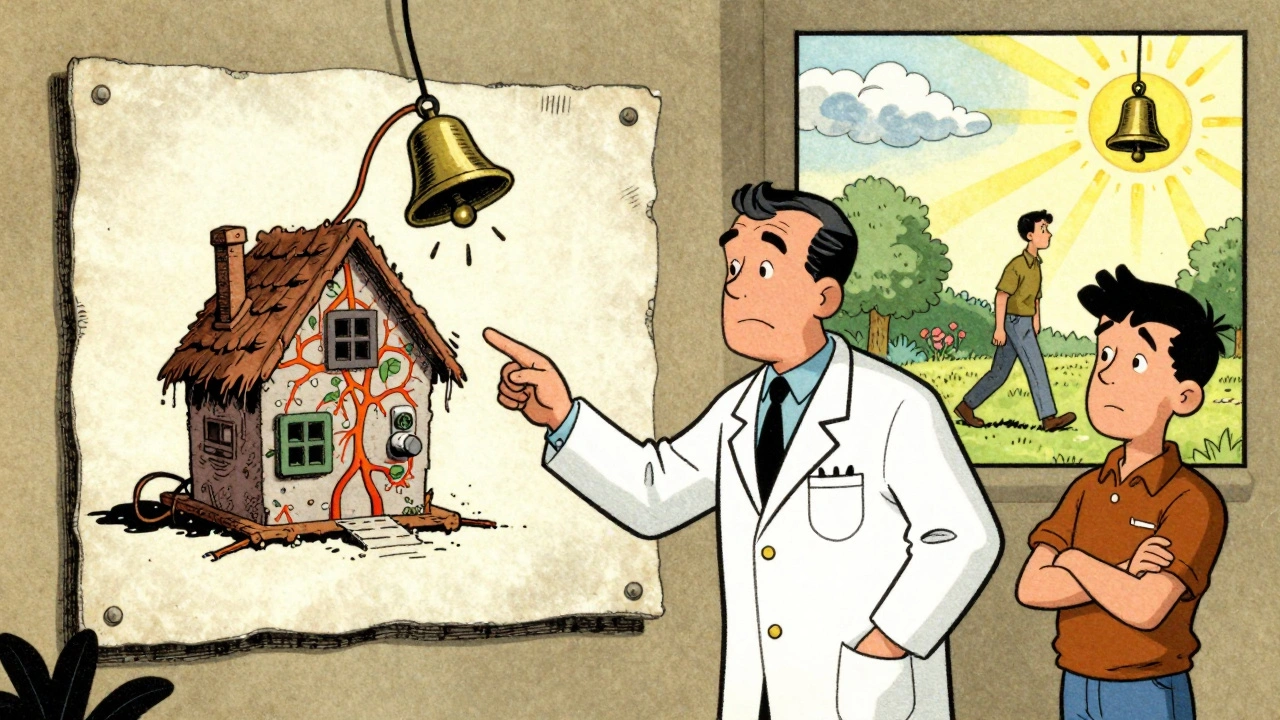
Imagine your nervous system as a smoke alarm. It’s not designed to detect fire - it’s designed to detect potential danger. Sometimes it goes off when there’s no fire at all. That’s what happens in chronic pain. The alarm gets too sensitive. It doesn’t mean your body is falling apart. It means your brain has learned to protect you too well.
How pain really works - not what you were told
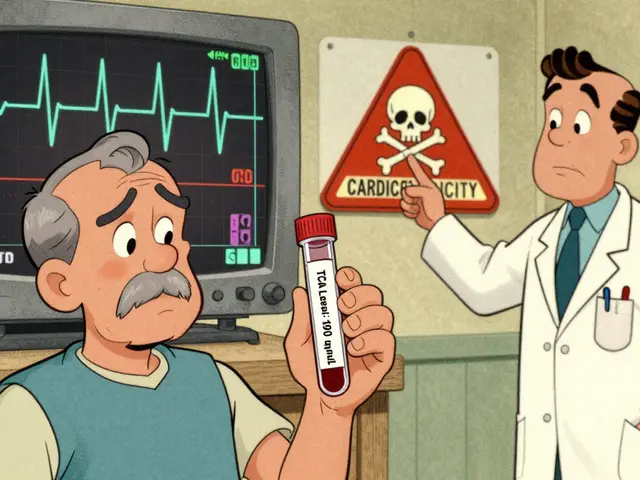
Traditional pain models focus on tissue damage. If you tear a muscle, you feel pain. Simple. But that model fails when people have severe pain with no visible injury - or when someone has a torn tendon but feels no pain at all. Pain neuroscience education (PNE) flips the script.
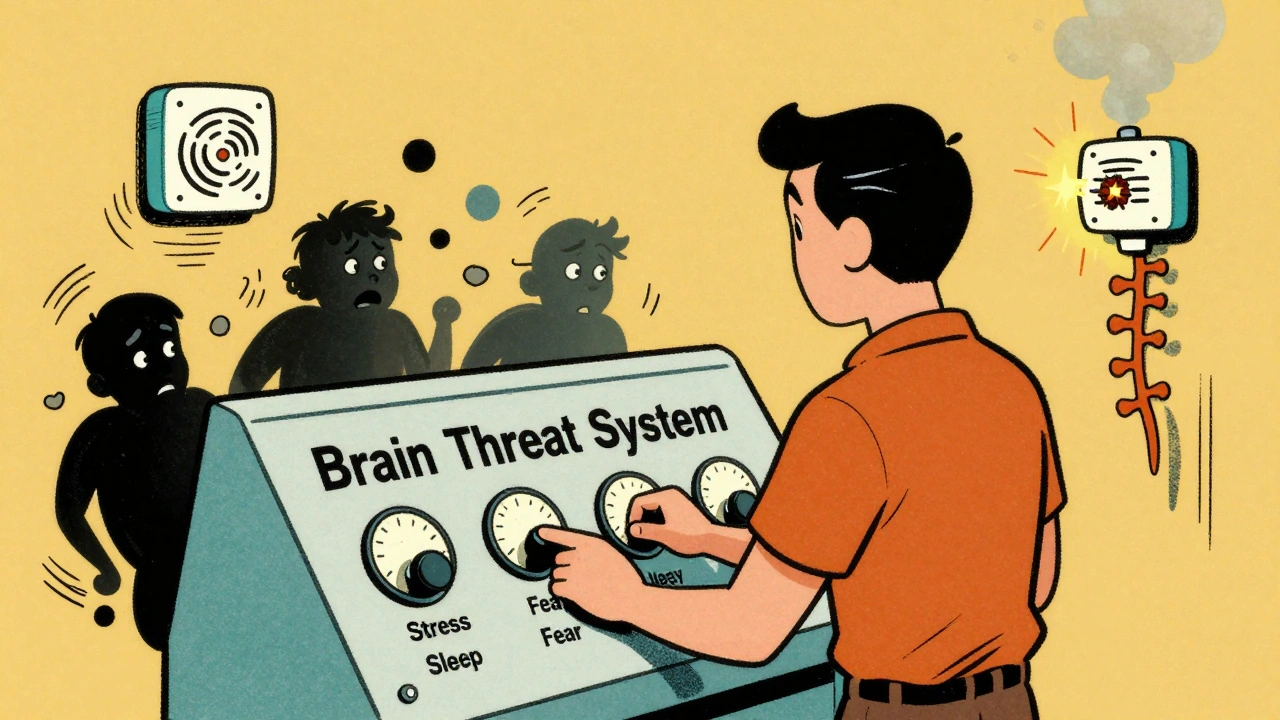
Pain isn’t a signal. It’s a threat response. Your brain takes input from your body - inflammation, movement, pressure - and combines it with everything else it knows: your past injuries, your stress levels, your fear of movement, even what your doctor said last week. Then it decides: is this dangerous? If yes, you feel pain. Even if there’s no tissue damage.
Key concepts in PNE include:
- Central sensitization: Your spinal cord and brain become hyper-responsive. Even light touch can feel painful because the system is stuck on high alert.
- Neuroplasticity: Your nervous system can change. It learned to hurt - and it can unlearn it.
- The biopsychosocial model: Pain isn’t just biological. It’s shaped by psychology (fear, anxiety) and social factors (work stress, sleep, support systems).
Studies show that people who understand this shift report less pain, move more freely, and rely less on medications. In one 2023 review of 23 trials, PNE reduced pain scores by an average of 1.8 points on a 10-point scale - not because their body changed, but because their brain did.
Why traditional pain advice often makes things worse
When you’re told, “Your spine is degenerating,” or “Don’t lift heavy things - you’ll hurt yourself,” your brain hears: “Your body is fragile. Movement is dangerous.” That message increases fear. Fear increases muscle tension. Tension increases pain. It’s a loop.
One patient I worked with in Perth had been told for years that her lower back pain was due to “instability.” She avoided bending, twisting, even walking too far. She stopped gardening, stopped playing with her grandchildren. Her pain didn’t get better - it got worse.
When we talked about how her nervous system had become overprotective - not her spine being broken - something shifted. She started moving again. Not because the pain disappeared, but because she stopped fearing it. Within three months, she was back on her feet, walking 5 kilometers daily. Her pain didn’t vanish - but her relationship with it did.
What does a PNE session actually look like?
PNE isn’t a lecture. It’s a conversation. A skilled clinician uses simple metaphors, drawings, and stories to explain how pain works. No jargon. No scary diagrams of nerves firing. Just clear, relatable ideas.
One common metaphor is the “alarm system.” Think of your nerves as a smoke alarm in a kitchen. If you burn toast, it goes off - that’s normal. But if the alarm is old, dusty, or wired wrong, it might go off every time you walk by - even without smoke. That’s what happens in chronic pain. The alarm is hypersensitive. The goal isn’t to fix the kitchen. It’s to recalibrate the alarm.
Another favorite is the “pain volume knob.” Your brain has a dial that turns pain up or down. Stress, sleep, worry, and even the weather can turn it up. Safety, movement, and understanding turn it down. PNE helps you find the knobs - and learn how to turn them.
Sessions usually last 30 to 45 minutes. They’re often done in person, but digital tools like the “Pain Revolution” app are now used by over 186,000 people worldwide. Many clinics now combine PNE with gentle movement - not to fix the body, but to prove to the brain that movement is safe.
Who benefits most from PNE - and who doesn’t?
PNE works best for people with persistent pain - pain that lasts longer than three months. That’s when the nervous system has had time to rewire itself. Studies show 82% of chronic pain patients respond well to PNE.
But it’s not a magic bullet. It doesn’t help much for acute pain - like a broken bone or recent surgery - where actual tissue damage is the main issue. And it’s less effective for people with very low health literacy or severe cognitive impairment. If someone can’t grasp the idea that pain isn’t always damage, the message gets lost.
Some patients walk away frustrated. They expected the pain to disappear after one session. PNE doesn’t promise that. It promises understanding. And understanding is the first step to real change.
What happens when you combine PNE with movement
PNE alone helps. But when you pair it with movement - even gentle walking, stretching, or strength training - the results jump.
Research shows that adding exercise to PNE improves outcomes by 30-40% compared to education alone. Why? Because movement is the best teacher for the brain. When you bend over without pain, your brain starts to believe: “Maybe it’s safe after all.”
One 42-year-old nurse with fibromyalgia in Adelaide started PNE with a physical therapist. She was taking six pain pills a day. After six sessions of PNE and a graded walking program, she cut her pills to one every three days. She didn’t become pain-free. But she became functional. She returned to work full-time. She stopped canceling plans.
That’s the goal: not to eliminate pain, but to reclaim your life despite it.
Why more clinics are using PNE - and how to find it
In 2010, only 12% of U.S. physical therapy programs taught PNE. By 2023, that number jumped to 72%. Medicare now reimburses for PNE as part of physical therapy visits. Companies like Liberty Mutual use it in workplace injury programs - and they’ve seen a 22% drop in claim duration.
But here’s the catch: only 28% of practicing physical therapists feel confident delivering it. That’s because it’s not just about knowing the science. It’s about how you say it. You need to listen. You need to meet people where they are. You need to replace phrases like “your disc is bulging” with “your brain is being extra careful.”
To find a provider who uses PNE, ask:
- “Do you explain pain using the brain and nervous system, not just imaging results?”
- “Do you use metaphors like ‘alarm system’ or ‘volume knob’?”
- “Do you combine pain education with movement?”
Look for therapists trained by the International Spine and Pain Institute or those who reference the “Explain Pain” handbook by David Butler and Lorimer Moseley. These are the most widely recognized resources.
The science behind why PNE works
It’s not just theory. Brain scans show real changes after PNE.
In a 2019 fMRI study, people with chronic pain showed 22% less activity in the insular cortex - the part of the brain that processes threat - after a PNE session. Their prefrontal cortex, which helps regulate emotions and decision-making, became more active. In other words: their brains stopped treating every twinge as an emergency.
That’s neuroplasticity in action. Your brain rewires itself based on new information. When you learn pain isn’t danger, your brain stops overreacting. That’s not placebo. That’s biology.
What to expect - and what not to expect
PNE is not quick. It’s not a one-time fix. It’s a shift in perspective. Some people feel lighter after one session. Others take weeks to let go of old beliefs.
Don’t expect:
- Pain to vanish overnight
- A miracle cure
- Someone to “fix” your body
Do expect:
- More confidence in moving
- Less fear of pain
- More control over your life
One Reddit user, PainWarrior87, wrote: “The metaphor of a sensitive smoke alarm helped me understand my pain wasn’t signaling danger. I’ve since returned to hiking and reduced opioid use by 75%.” That’s the power of PNE. It doesn’t erase pain. It gives you back your life.
Final thought: Pain is not your enemy
Pain is trying to protect you. It’s just been misled. PNE doesn’t tell you to ignore your pain. It tells you to understand it. Once you do, you stop fighting yourself. You stop fearing movement. You stop waiting for a miracle.
You start living again - not because the pain is gone, but because you’re no longer afraid of it.





Comments
i was told my back was 'degenerated' and i believed it for years. then i read about pain being an alarm system and it just clicked. i started walking again. no magic, just less fear. now i garden with my grandkids.
thank you for this.
this is the most important thing i've read about pain in 10 years. i used to think my chronic knee pain meant i was broken. turns out my brain was just being overly protective. i started moving again, slowly, and now i'm hiking again.
the smoke alarm metaphor? genius. 🙏
ok but let’s be real-this is just placebo with fancy words. if your pain doesn’t go away after one session, you’re just not trying hard enough. the fact that you’re still in pain means your body is still damaged. stop letting your brain trick you into thinking it’s all in your head.
i’ve been living with fibromyalgia for 17 years. i’ve seen every specialist, had every scan, taken every pill, tried every diet, meditated, cried, screamed, and still woke up in pain every morning. then i found this. not because i suddenly got stronger or my tissues healed-but because i stopped fighting my own nervous system. i don’t have less pain, but i have more life. and that’s worth more than any pill. i’m not cured. but i’m finally free.
so let me get this straight-you’re telling me the entire medical establishment has been lying to us for decades? that all these MRIs and surgeries are just scams to keep us dependent? that doctors don’t even know what pain is? and now some guy in Australia wrote a book and suddenly we’re all supposed to believe pain is just a ‘sensitive alarm’? sorry, but if my spine is visibly degenerating on the scan, it’s not ‘in my head’-it’s in my spine. this feels like a cult.
this is textbook pseudoscience dressed up as enlightenment. you’re not ‘retraining your brain’-you’re gaslighting patients into ignoring real pathology. if you have a torn meniscus, it’s torn. no amount of metaphors changes that. this is why people end up in wheelchairs-they’re told their pain isn’t real.
i used to think pain was a direct line from injury to suffering. then i hurt my back lifting a box, got an MRI that showed ‘mild degeneration,’ and spent 2 years terrified to bend over. then i found a therapist who explained the alarm system. i didn’t need surgery. i needed to stop being afraid. now i deadlift again. not because my spine is fixed-but because my brain finally stopped screaming ‘DANGER’ at every movement. this isn’t magic. it’s science.
i’ve read the ‘Explain Pain’ book. it’s cute. but let’s not pretend this is revolutionary. this is just rebranded cognitive behavioral therapy with neuroscience buzzwords. if you’re going to call it ‘pain neuroscience education,’ at least cite the actual fMRI studies-not cherry-picked anecdotes from Reddit. also, the ‘volume knob’ metaphor is infantilizing. we’re adults, not toddlers with a dimmer switch.
i’m a PT and i’ve been using PNE for 5 years now. the results? life-changing. not for everyone-but for the people who’ve been told ‘it’s all in your head’ and then find out ‘it’s not in your head, it’s your brain being too careful’? that’s the turning point. i’ve had patients go from wheelchairs to walking 5k. not because we fixed their spine. because we fixed their fear. if you’re skeptical, try it. just listen. don’t fix. just explain.
pain is the soul’s whisper when the body forgets how to breathe.
so now we’re supposed to believe pain is a metaphor? cool. next they’ll tell us cancer is just your cells having a bad day. this is the kind of woo that kills people. if your knee hurts, get it scanned. if your spine is degenerating, stop pretending it’s ‘just an alarm.’ you’re not a smoke detector. you’re a human being with real tissue. stop letting therapists make you feel guilty for wanting real answers.
PNE is the missing link between biopsychosocial models and clinical practice. The neuroplasticity evidence is robust-fMRI changes in the insula and prefrontal cortex are replicated across multiple RCTs. What’s often missed is that PNE isn’t a standalone intervention. It’s a catalyst for graded exposure. The education primes the brain to tolerate movement, which then drives descending inhibition. That’s why combining it with movement yields 30-40% better outcomes. This isn’t fluff. It’s neurobiology.
The application of pain neuroscience education represents a paradigmatic shift in the clinical management of persistent pain conditions. The integration of neurobiological principles with psychosocial context facilitates a more holistic therapeutic approach. It is imperative that practitioners articulate these concepts with precision and fidelity to the evidence base, lest the intervention be reduced to mere anecdotal appeal.
I’ve seen this exact ‘pain is a myth’ nonsense destroy lives. My cousin was told her chronic pain was ‘all in her head’ after she had a spinal fusion. They told her to ‘retrain her brain.’ She stopped taking her meds. She stopped seeing specialists. She ended up in the ER with a collapsed vertebra because no one listened when she said it hurt. This isn’t empowerment-it’s negligence. If your spine is broken, it’s broken. Don’t let some therapist talk you out of getting real help.