Blood Thinner Timing Calculator for Spinal Procedures
Blood Thinner Timing Calculator
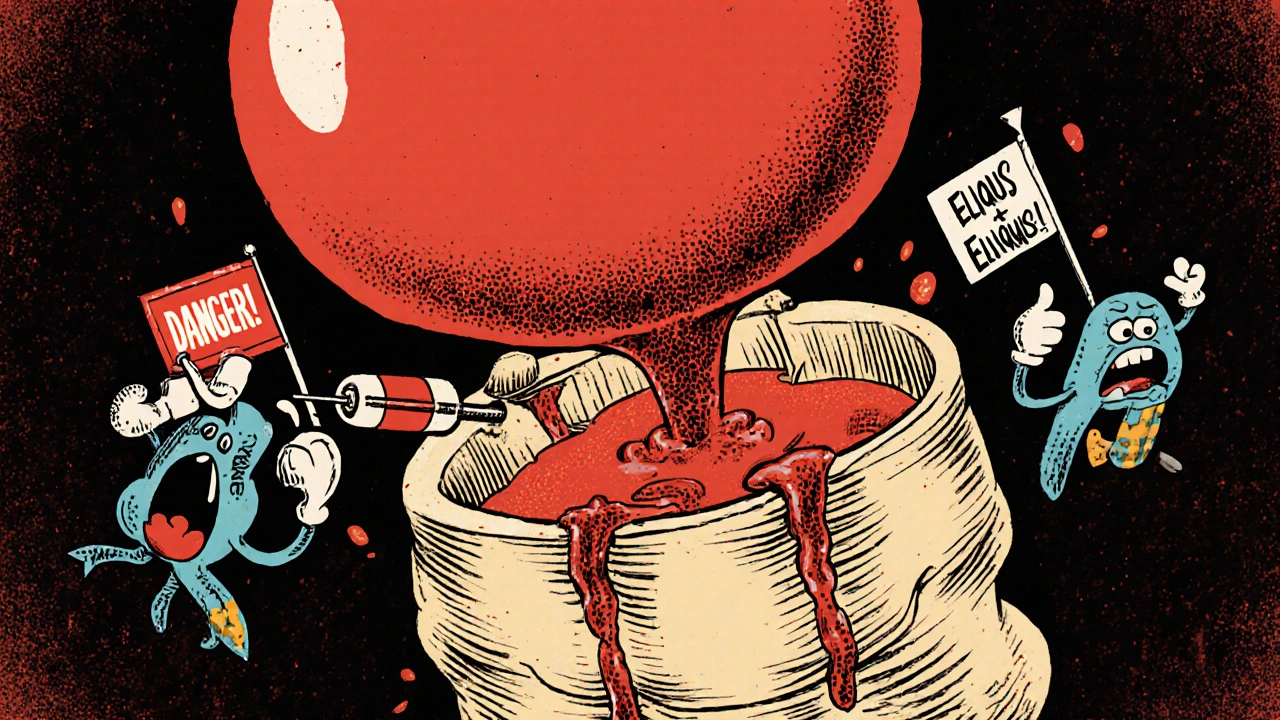
Getting an epidural or spinal injection while on blood thinners isn’t as simple as showing up and lying down. Even though these procedures are common-used for labor pain, back surgery, or chronic pain management-they carry a rare but terrifying risk: spinal epidural hematoma. This is when blood collects in the tight space around your spinal cord, squeezing it like a tube being pinched shut. If not caught fast, it can cause permanent paralysis. And the people most at risk? Those taking medications to prevent blood clots.
Why Blood Thinners Make Spinal Procedures Risky
Your body has two competing systems: one that stops bleeding, and one that keeps blood flowing. Blood thinners like warfarin, enoxaparin (Lovenox), rivaroxaban (Xarelto), or apixaban (Eliquis) tip the balance toward flow. That’s good for preventing strokes or clots in your legs. But when you stick a needle near your spine, you’re poking a delicate area packed with blood vessels. A small leak can turn into a dangerous pool of blood-sometimes as little as 1-2 milliliters-because the spinal canal has almost no room to spare. This isn’t theoretical. Between 1992 and 2013, the FDA documented 100 confirmed cases of spinal or epidural hematomas linked to Lovenox alone. And while the overall chance is low-about 1 in 150,000 for a simple epidural-it spikes dramatically under certain conditions. For example, if you’re on therapeutic-dose enoxaparin and the procedure happens less than 24 hours after your last dose, your risk jumps to 0.31%. That’s nearly eight times higher than if you waited long enough.Who’s Most at Risk?
It’s not just about the drug. Risk comes from a mix of factors:- Medication type: Warfarin is dangerous if your INR is above 1.4-your risk increases nearly ninefold. Therapeutic-dose LMWH (like Lovenox) carries a 4.3 times higher risk than prophylactic doses. DOACs like rivaroxaban and apixaban are safer when timed right, but still risky if taken too close to the procedure.
- Procedure type: A simple diagnostic spinal tap has a risk of 0.001%. A single epidural steroid shot? About 0.0067%. But if you’re getting an epidural catheter left in place for days, or undergoing complex spinal surgery, your risk climbs to 0.5-1.0%.
- Technical factors: More than three needle attempts? Your risk goes up 6.2 times. If the needle hits a blood vessel and you see blood-tinged fluid? Risk jumps 11.8 times.
- Your body: Age over 70? Risk triples. Kidney problems? Risk nearly quintuples. Low hemoglobin? Risk more than quadruples. Spinal stenosis? Risk doubles.
Even healthy people aren’t safe if timing is off. One case study in Pain Medicine showed a patient on warfarin with a perfectly normal INR of 1.2 still developed a hematoma-and ended up with permanent foot drop.
What Happens When a Hematoma Forms?
Symptoms don’t sneak up. They hit hard and fast:- Severe, sharp back pain (93% of cases)
- Numbness or tingling in legs, buttocks, or groin (89%)
- Weakness or inability to move legs (76%)
- Loss of bladder or bowel control (34%)
These usually show up within 12 hours-sometimes as early as 2. The clock is ticking. A 2018 study found that patients who got surgery within 8 hours had a 79% chance of full recovery. After 24 hours? Only 9% recovered fully. Permanent paraplegia happens in about 24% of cases. And if treatment is delayed, 3-5% of patients die.
How Long Should You Stop Your Blood Thinners?
Timing isn’t guesswork. It’s science. Here’s what the latest guidelines (ASRA 2017, updated 2022) say:Warfarin
- Stop 5 days before the procedure.
- Check INR within 24 hours before. Target: less than 1.4.
- Restart 4 hours after a single-shot procedure. Wait 6 hours if you’re getting a catheter.
Low Molecular Weight Heparin (LMWH-e.g., Lovenox)
- Prophylactic dose (e.g., 40 mg daily): Stop 10-12 hours before.
- Therapeutic dose (e.g., 1 mg/kg twice daily): Stop 24 hours before.
- Restart 2 hours after single injection. Wait 4 hours for catheters.
Direct Oral Anticoagulants (DOACs-e.g., Xarelto, Eliquis)
- Apixaban or rivaroxaban with normal kidney function (CrCl >50 mL/min): Stop 48 hours before.
- Same drugs with kidney impairment (CrCl <30 mL/min): Stop 72 hours before.
- Restart 2-4 hours after procedure, depending on catheter use.
These windows aren’t suggestions. They’re based on how long each drug stays active in your blood. Skip them, and you’re gambling with your spine.
What About Aspirin or Plavix?
This is where things get messy. Some doctors say aspirin is safe to keep taking. One study of over 1,200 epidural steroid injections found zero hematomas in patients who kept their daily aspirin. Another study found dual antiplatelet therapy (like aspirin + clopidogrel) increased risk nearly fourfold. So if you’re on just aspirin for heart protection? You might be fine. But if you’re on two antiplatelets after a stent? That’s a red flag. Most experts recommend stopping dual therapy 5-7 days before a spinal procedure.What If You Can’t Stop Your Blood Thinners?
Some patients can’t stop-like those with mechanical heart valves, recent clots, or high stroke risk. For them, the choice isn’t easy. You might need:- A different kind of pain control: peripheral nerve blocks instead of spinal/epidural.
- General anesthesia instead of regional.
- Close monitoring in a hospital setting for 24 hours after the procedure.
There’s no perfect solution. But avoiding the procedure altogether isn’t always the answer either. A 2023 study showed that with proper planning, even high-risk patients can safely receive neuraxial anesthesia-just not without a detailed team approach.

What Should You Do Before Your Procedure?
Don’t wait for your doctor to bring it up. Take charge:- Make a full list of every medication you take-prescription, over-the-counter, supplements. Include doses and when you last took them.
- Ask: “Am I on a blood thinner? Which one? What’s the safest way to pause it?”
- Request a copy of your latest INR or kidney function test.
- Confirm your anesthesiologist has reviewed your anticoagulation plan before you’re wheeled in.
- Know the warning signs: back pain, numbness, weakness. Report them immediately.
One anesthesiologist on Reddit shared a near-miss: a 68-year-old patient on rivaroxaban developed saddle anesthesia 12 hours after catheter removal. He needed emergency surgery and still lost nerve function in his L5 nerve. That patient didn’t know he was at risk. He didn’t know to ask.
How to Stay Safe: Tools and Resources
You’re not alone in this. There are tools to help:- The ASRA Anticoagulation Checklist is updated quarterly and available free online.
- The mobile app Neuraxial Anticoag has been downloaded over 12,000 times and gives real-time timing guidance.
- Many hospitals now use electronic alerts that flag anticoagulant use when a spinal procedure is ordered.
But here’s the catch: a 2021 study found 17% of digital tools had outdated info. Always double-check with your care team. Don’t rely on an app alone.
The Bigger Picture: Why This Matters
Spinal epidural hematomas are rare-but when they happen, they’re devastating. The average cost to treat one? Over $287,000. That’s not just money. It’s years of rehab, lost independence, and lifelong disability. In 2022, 78 malpractice claims were filed in the U.S. over these cases. Sixty-two percent resulted in settlements averaging $1.2 million-mostly because guidelines weren’t followed.Regulators are stepping in. The FDA now requires all anticoagulant manufacturers to include clear warnings about neuraxial procedures. Starting in 2025, U.S. hospitals doing more than 50 spinal procedures a year must report their hematoma rates. This isn’t bureaucracy-it’s patient safety.
And research is moving forward. A 2022 study found that a blood biomarker called GFAP can detect spinal bleeding within 2 hours-with 94% accuracy. That could mean earlier surgery and better outcomes.
But until those tools are routine, the best defense is knowledge. Know your meds. Know the timing. Speak up. Your spine doesn’t forgive mistakes.
Can I still get an epidural if I’m on blood thinners?
Yes-but only if your medication is properly timed and your risk factors are assessed. Many people on blood thinners safely receive epidurals or spinal anesthesia when guidelines are followed. The key is stopping the drug for the correct number of hours before the procedure and restarting it safely afterward. Never assume it’s safe without checking with your doctor and anesthesiologist.
How do I know if I’m having a spinal hematoma?
Symptoms come on quickly: severe back pain, numbness or tingling in your legs or groin, weakness in your legs, or trouble controlling your bladder or bowels. If you’ve had a spinal or epidural procedure in the last 12-24 hours and notice any of these, tell your medical team immediately. Waiting even a few hours can make the difference between full recovery and permanent damage.
Is aspirin safe to take before a spinal procedure?
For most people taking only aspirin (81 mg or 325 mg daily), the risk of spinal hematoma is extremely low-studies show it’s close to zero. Many anesthesiologists allow patients to keep taking aspirin. But if you’re on aspirin plus another antiplatelet like clopidogrel (Plavix), that doubles or triples your risk. Always disclose all medications, and follow your provider’s advice.
What if I can’t stop my blood thinner because I have a heart valve or recent clot?
In these high-risk cases, alternatives are available. You may receive a different type of pain control, like a nerve block in your arm or leg, or general anesthesia instead of spinal/epidural. Your care team may also monitor you closely in the hospital for 24 hours after the procedure. Never stop your anticoagulant without consulting your cardiologist or hematologist-stopping could cause a life-threatening clot.
Do I need to stop my blood thinner if I’m just getting a diagnostic spinal tap?
Even for a simple spinal tap, guidelines still apply. The risk is very low-about 1 in 100,000-but it’s not zero. If you’re on warfarin, you’ll still need your INR checked. If you’re on LMWH or DOACs, you’ll still need to pause it for the recommended time. Never assume a "minor" procedure is risk-free when you’re on blood thinners.
Can I use a mobile app to time my blood thinner before a spinal procedure?
Apps like Neuraxial Anticoag can be helpful tools-they’re designed by experts and updated regularly. But they’re not foolproof. A 2021 study found 17% of digital tools had outdated recommendations. Always cross-check with your anesthesiologist or pharmacist. Never rely on an app alone. Your life depends on accurate timing, not an algorithm.




Comments
Got my epidural last year on Xarelto. Docs made me stop 48 hours before. Felt weird lying there waiting but better safe than paralyzed.
As a pain management fellow, I can tell you the biggest mistake I see is underestimating the time needed for DOAC clearance. People think 'oh it's a new drug so it's safer'-but if you don't wait the full 48 hours with renal impairment, you're playing Russian roulette with their spinal cord. The data is crystal clear: delay = survival. Speed = paralysis.
And don't get me started on the nurses who push for 'just one quick shot' because the patient is 'in so much pain.' That one quick shot can cost someone their mobility for life.
Always check CrCl. Always double-check last dose. Always document. And if there's any doubt? Delay it. No one ever got sued for waiting an extra 6 hours.
I keep thinking about how fragile we are. One needle. One tiny bleed. One moment where the system fails. We trust doctors to be gods, but they're just people juggling a hundred variables-meds, labs, timing, anatomy, fatigue. And yet, we ask them to make life-or-death calls with a 1-in-150,000 chance of disaster. That’s not statistics. That’s a human being’s future hanging by a thread.
It’s not about fear. It’s about reverence. For the spine. For the blood. For the silence between heartbeat and paralysis.
I’m not a doctor. But I’ve sat in those waiting rooms. And I know what it feels like to be told 'it’s fine' when your whole body is screaming 'what if it’s not?'
Y'all are ignoring the REAL issue: pharmaceutical companies pushed these DOACs because they make more money than warfarin. They downplayed the bleeding risks. The FDA knew. The guidelines were manipulated. You think 48 hours is enough? That's what they told you. But the real data? Buried. Just like the 2015 study where 17 patients got hematomas after 'safe' timing. All lawsuits settled with NDAs.
They want you to believe it's safe. It's not. It's a money scheme wrapped in medical jargon.
Let’s be real-this whole 'risk of paralysis' thing is just fearmongering. I’ve seen 300+ epidurals in my practice. Zero hematomas. Zero. Meanwhile, people die from DVTs because they’re too scared to get their meds. You’re more likely to get hit by lightning than have a spinal hematoma from an epidural on anticoagulants. The real danger is overcautious medicine that denies people pain relief and causes opioid dependence. We’re trading one disaster for another.
Also, the stats? Useless. You’re comparing a single-dose epidural to a 3-day catheter in a 75-year-old with renal failure and stenosis. Of course the risk is higher. But that’s not the average patient. Stop scaring healthy people out of necessary care.
And why are we even talking about this? Because someone got a bad outcome and now everyone’s treating every epidural like a nuclear launch code.
Man I had a buddy who got a spinal tap for a headache and ended up in a wheelchair because they didn’t wait long enough on his Eliquis. He was 32. Had a baby on the way. Now he can’t feel his toes. I still think about it. The docs said 'it’s fine' and he trusted them. That’s the problem. We’re taught to trust the system but the system’s got holes bigger than a truck.
Don’t be the guy who says 'I’m fine' and skips the wait. Be the guy who asks 'what if I’m not?'
And if you’re a provider? Don’t rush. Don’t assume. Don’t let the clock run on someone else’s spine.
Y’all are missing the point. This isn’t about meds or timing. It’s about the fact that hospitals are understaffed and nurses are overworked. Someone’s gonna screw up. Someone’s gonna forget to check the INR. Someone’s gonna do the procedure 2 hours after the last Lovenox because the patient is crying. It’s not a question of IF. It’s WHEN. And when it happens, you’ll see headlines. But by then, the damage is done.
And the docs? They’ll say 'it was an unfortunate complication.' Meanwhile, the patient’s wife is begging for answers.
And we’re still letting this happen? 😡
So you're telling me I gotta stop my blood thinner for 48 hours but I can still get a CT scan with contrast that'll fry my kidneys? What a joke. The system's rigged. They care more about liability than actual care. I'd rather take my chances with the needle than with the hospital billing department.
Also I typoed 'epidural' as 'epidural' twice. Whatever. You get the point.
I got my epidural while on Lovenox and they didn't even check my labs. Just said 'you're fine' and stuck the needle in. I felt a zap. But no pain. No numbness. I'm fine. So maybe all this fear is just hype.
Thank you for sharing this information with such clarity. It is important that we approach medical decisions with both compassion and precision. For many patients, especially those from communities with limited access to specialist care, understanding these risks can be life-changing. I hope this post reaches those who need it most.
Let me correct the inaccuracies in this post. The ASRA guidelines were not 'updated in 2022'-they were reaffirmed with minor clarifications. Also, the FDA's 100-case dataset included only confirmed cases, but the true incidence is likely higher due to underreporting. And you omitted the critical point that spinal hematomas are more common in patients with undiagnosed spinal vascular malformations-a factor not accounted for in any risk stratification. This entire narrative is dangerously oversimplified.
I knew this would happen. I’ve been saying for years that the medical industry is slowly turning us all into paralyzed lab rats. They don’t care about us. They care about the lawsuits they’ll avoid. They don’t want you to know that there’s a secret protocol where they use a different needle if you’re on blood thinners-it’s thinner, less visible, but causes more micro-bleeds. They hide it because if you knew, you’d never sign the consent form. I’ve seen the documents. I’ve talked to the insiders. This isn’t medicine. It’s control. And they’re using your fear of pain to keep you quiet.
And don’t even get me started on the fact that the same companies that make Xarelto also own the MRI machines that diagnose these hematomas. It’s a closed loop. You get the shot. You get paralyzed. They get the machine time. They profit twice.
Wake up. This is bigger than epidurals. This is about who owns your body.
Thank you for the comprehensive overview. The data presented aligns with current clinical standards as outlined in the 2022 ASRA update. It is imperative that clinicians rigorously adhere to the recommended intervals for anticoagulant cessation, particularly in patients with comorbid renal insufficiency or advanced age. The temporal window between last dose and procedural intervention remains the most modifiable risk factor. I have observed that multidisciplinary coordination-between pharmacy, anesthesia, and primary care-is the single most effective strategy to mitigate adverse outcomes in this population.
Did you know that the CDC has quietly stopped tracking spinal hematoma cases since 2018? Coincidence? I think not. The real reason they’re pushing this 'timing' narrative is to cover up the fact that the needles being used are defective. They’re made in China. The tip is too sharp. It slices the dura instead of parting it. That’s why the bleeding is so bad. They don’t want you to know. They’d rather you blame the drug.