COPD Medication Safety Checker
Check Your Medications for COPD Safety
This tool helps you identify medications that may worsen your COPD. Based on GOLD 2023 guidelines and clinical studies, certain drugs can increase risk of respiratory failure or hospitalization. Always consult your doctor before making any changes to your medications.
How this tool works
Enter your medications and we'll check them against high-risk categories for COPD patients. Results will show safety status, potential risks, and safer alternatives when available.
Living with COPD means every medication you take - even something as simple as a sleep aid or painkiller - can either help or hurt your breathing. It’s not just about the disease itself. The real danger often comes from drugs that seem harmless on the surface but quietly worsen lung function. Many people with COPD are unaware that common prescriptions and over-the-counter meds can trigger hospital visits, or worse. The good news? Avoiding just a few high-risk medications can cut your risk of a serious flare-up by nearly a third.
Why Some Medications Are Dangerous for COPD
COPD damages the lungs’ ability to move air in and out. Your body already works harder just to breathe. When you add a drug that slows down your breathing or thickens mucus, you’re stacking the odds against yourself. The problem isn’t always the drug itself - it’s how it interacts with your already compromised lungs.
According to the GOLD 2023 guidelines, about 1 in 5 COPD hospitalizations are caused by medications that shouldn’t have been taken in the first place. That’s preventable. And it’s not just about big, scary drugs. Some of the most dangerous ones are the ones you can buy without a prescription.
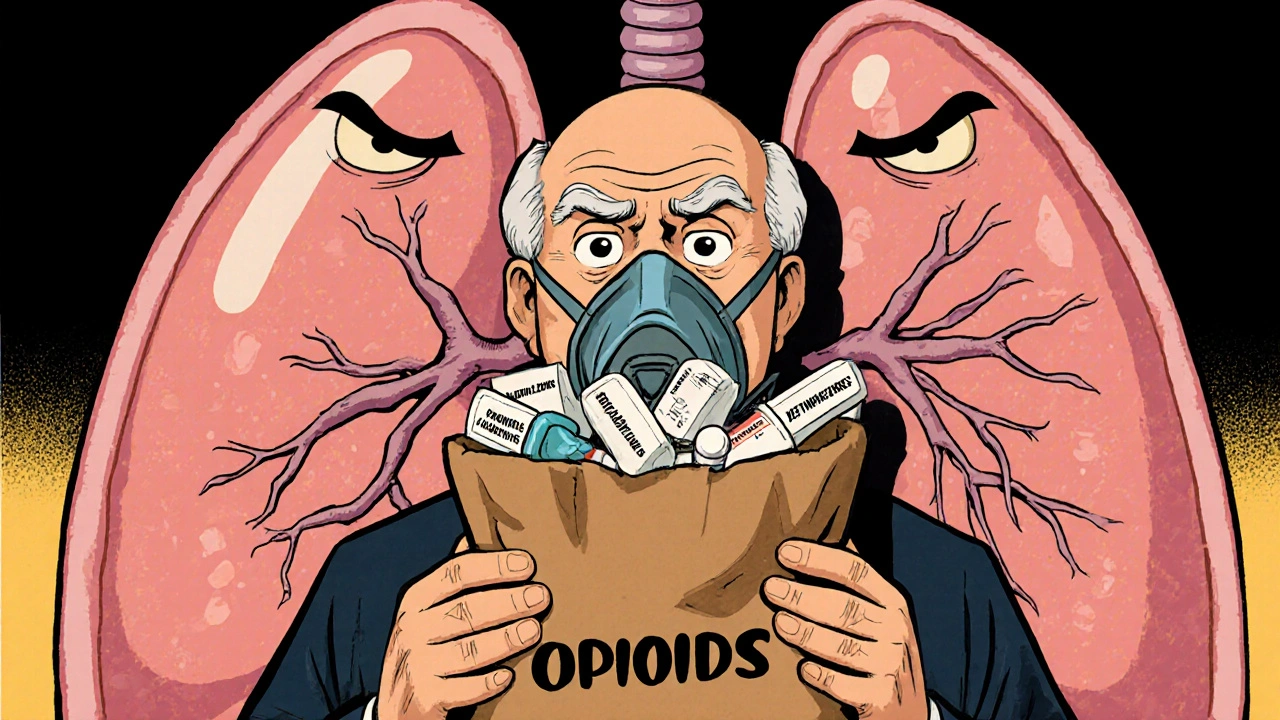
Opioids: The Silent Respiratory Suppressors
Opioids like morphine, oxycodone, and hydromorphone are powerful painkillers, but they’re also powerful suppressors of your brain’s breathing drive. In healthy people, this might just mean drowsiness. In someone with COPD, it can mean stopping breathing entirely.
A 2022 study in the American Thoracic Society journal found that COPD patients on opioids had a 37% higher chance of respiratory failure than those using non-opioid pain relief. The CDC recorded over 1,200 COPD-related deaths tied to opioids in the U.S. in 2021 - a number that’s been climbing since 2019.
Even low doses can be risky. One patient in Perth, age 68 with moderate COPD, was prescribed oxycodone for back pain. Within a week, his oxygen levels dropped at night. He didn’t realize the medication was the cause until his pulmonologist asked about all his pills. Switching to acetaminophen and physical therapy brought his breathing back to baseline.
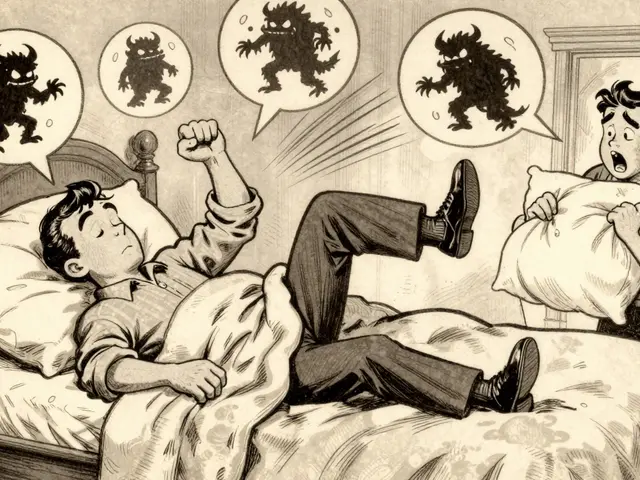
Benzodiazepines and Sleep Aids: A Deadly Combo
Alprazolam (Xanax), diazepam (Valium), zolpidem (Ambien), and eszopiclone (Lunesta) are all CNS depressants. They calm your nerves - and your breathing. When taken alone, they’re risky for COPD. When taken with opioids? The risk of respiratory arrest jumps by 400%, according to a 2022 study in Chest Journal.
In 2021, nearly 3 out of 10 COPD patients hospitalized for breathing problems had used a prescription sleep aid in the prior 30 days. These drugs don’t just make you sleepy - they blunt your body’s natural response to low oxygen. Your brain stops telling you to breathe harder when you need to.
There are safer alternatives. Cognitive behavioral therapy for insomnia (CBT-I) works better than pills for long-term sleep. Melatonin, under a doctor’s guidance, is often a gentler option. Always talk to your doctor before stopping or starting any sleep medication.
Non-Selective Beta-Blockers: Hidden Lung Constrictors
Many people with COPD also have heart disease. Beta-blockers are commonly prescribed to protect the heart. But not all beta-blockers are the same.
Non-selective ones - like propranolol, nadolol, and timolol - block receptors in the lungs as well as the heart. This causes bronchoconstriction, tightening your airways. A 2022 meta-analysis found these drugs increase COPD exacerbation risk by 31%.
Cardioselective beta-blockers like metoprolol and bisoprolol are much safer. They mainly target the heart. One patient shared on a COPD forum: “Switching from propranolol to metoprolol improved my FEV1 by 15% in three months. I had no idea my heart med was choking my lungs.”
If you’re on a beta-blocker and your breathing has gotten worse, ask your doctor: “Is this cardioselective?” If not, ask about switching.

First-Generation Antihistamines and Tricyclic Antidepressants: Mucus Traps
Diphenhydramine (Benadryl), hydroxyzine, and tricyclic antidepressants like amitriptyline have strong anticholinergic effects. That means they dry up secretions - including the mucus in your lungs.
Thicker mucus is harder to cough out. That leads to clogged airways, infections, and flare-ups. A 2021 study in the Annals of Allergy, Asthma & Immunology showed these drugs increase sputum viscosity by up to 35% in COPD patients.
Tricyclics are especially risky. A 2022 study found 27% of COPD patients on these drugs had worsening breathing, compared to just 9% on SSRIs like sertraline or escitalopram.
The Beers Criteria, updated in 2023, lists both first-gen antihistamines and TCAs as medications to avoid in older adults with COPD. Safer options? Second-gen antihistamines like loratadine (Claritin) or cetirizine (Zyrtec) don’t thicken mucus. For depression, SSRIs are preferred.
ACE Inhibitors: The Cough Trap
ACE inhibitors like lisinopril and enalapril are common for high blood pressure. But they cause a dry, hacking cough in 12-20% of users. For someone with COPD, that cough isn’t just annoying - it can trigger a flare-up.
The cough hits harder in certain groups: 35% of Asian patients, 25% of African American patients, and 15% of Caucasian patients. That’s not random - it’s genetic.
The American Heart Association recommends switching to ARBs (angiotensin II receptor blockers) like losartan or valsartan for COPD patients. ARBs lower blood pressure without the cough. One study showed a 68% lower rate of cough-related complications compared to ACE inhibitors.
Clarithromycin and Macrolide Antibiotics: Hidden Interactions
Clarithromycin (Biaxin) is often used for lung infections. But it interferes with how your liver breaks down other drugs - especially opioids. A 2021 study found it can boost opioid blood levels by up to 60%, increasing the risk of breathing suppression.
Azithromycin is sometimes used long-term to prevent COPD flare-ups, but it carries its own risk: QTc prolongation. That’s an electrical change in the heart that can lead to dangerous arrhythmias - especially in older patients with heart disease, which is common in COPD.
If you’re prescribed an antibiotic, ask: “Is this the best choice for my COPD and other meds?” Sometimes amoxicillin or doxycycline are safer alternatives.

Muscle Relaxers: Underestimated Danger
Cyclobenzaprine (Amrix), methocarbamol, and baclofen are often given for back pain or spasms. But they depress the central nervous system - just like opioids and benzodiazepines.
A 2020 Mayo Clinic study found that 22% of COPD patients on muscle relaxers needed emergency care for breathing trouble within 30 days. That’s more than 1 in 5.
Physical therapy, heat packs, and stretching are safer for managing muscle tension. If you must take a muscle relaxer, do it under close supervision - and never combine it with other sedatives.
What to Do Now: Your Action Plan
Don’t panic. But do take action.
- Do a brown bag review. Take every pill, supplement, and OTC med you take to your next doctor or pharmacist appointment. Include sleep aids, painkillers, allergy meds, and herbal supplements.
- Ask these questions: “Is this safe for COPD?” “Is there a safer alternative?” “Could this interact with my other meds?”
- Check your anticholinergic burden. Use the Anticholinergic Cognitive Burden Scale (available online) to see if multiple meds are adding up to a dangerous level.
- Get a pharmacist involved. A 2023 study showed pharmacist-led reviews cut COPD hospitalizations by 29%. Pharmacists are trained to spot hidden risks.
- Track your symptoms. If your breathing gets worse after starting a new med - even a small one - write it down and tell your doctor immediately.
Medication Safety Is a Team Effort
COPD management isn’t just about inhalers. It’s about every pill you swallow. The best doctors and pharmacists know this. They don’t just treat the lungs - they treat the whole person and everything they’re taking.
One patient summed it up: “I thought my meds were helping. Turns out, some were hurting me more than the disease.”
You don’t have to live with that risk. With the right information and a proactive approach, you can protect your lungs - one medication at a time.
Can I still take ibuprofen if I have COPD?
Yes, ibuprofen and other NSAIDs like naproxen are generally safe for COPD patients. They don’t suppress breathing or thicken mucus. However, if you have kidney problems or high blood pressure - common with COPD - talk to your doctor first. Long-term use can affect kidney function and fluid balance. Acetaminophen is often preferred for daily pain relief in COPD.
Are inhaled corticosteroids safe for COPD?
Yes, inhaled corticosteroids are commonly used in COPD, especially for patients with frequent flare-ups. They reduce lung inflammation directly in the airways with minimal side effects because very little enters the bloodstream. They’re not the same as oral steroids, which can cause muscle weakness and fluid retention. Always rinse your mouth after using them to prevent thrush.
What about CBD oil or marijuana for COPD?
Smoking or vaping marijuana is not recommended - it irritates the lungs and can worsen COPD symptoms. CBD oil taken orally or sublingually doesn’t carry the same risk, but research is still limited. There’s no strong evidence it improves lung function. It may help with anxiety or pain, but it’s not a substitute for proven COPD treatments. Always tell your doctor if you’re using CBD.
Can I take allergy meds if I have COPD?
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are safe for COPD. Avoid first-generation ones like diphenhydramine (Benadryl) and hydroxyzine - they thicken mucus and make breathing harder. If you’re unsure, check the label for “anticholinergic” or “drowsiness” warnings.
How often should I review my medications?
At least twice a year - or anytime you start or stop a medication. Many COPD patients are on 8-12 different drugs. The more meds you take, the higher the chance of dangerous interactions. A pharmacist-led medication review can catch problems your doctor might miss. Some clinics offer free reviews through Medicare or private insurance.
Next Steps
If you’re on any of the high-risk medications listed - opioids, benzodiazepines, non-selective beta-blockers, first-gen antihistamines, or muscle relaxers - don’t stop them cold turkey. Talk to your doctor about a safe tapering plan.
Start with your brown bag review. Bring every pill, capsule, and bottle to your next appointment. Write down when you started each one and why. Ask: “Is this still necessary? Is there a safer option?”
Small changes - swapping one drug for another - can make a huge difference. One patient in Perth replaced her nightly Ambien with melatonin and a breathing exercise routine. Within two months, her nighttime oxygen levels improved by 8%. That’s not magic. That’s smart medication management.


Comments
I’ve been on oxycodone for 3 years-my doctor said it was fine, but I’ve been crashing at night… I just didn’t connect the dots. Now I’m switching to acetaminophen and I can actually sleep without feeling like my lungs are drowning. Why didn’t anyone warn me sooner???
Let me guess-this is all part of the Big Pharma agenda to keep you dependent on their overpriced, government-approved poisons. They don’t want you breathing better-they want you on 12 different pills so they can bill Medicare. Did you know the WHO quietly banned benzos in 1998? They just didn’t tell you. And now they’re pushing SSRIs as the ‘safe’ alternative… but what if those are just the next phase of the chemical control program?
Stop lying to people. Opioids are dangerous? So are NSAIDs. So is water. You’re not telling the whole truth. The real issue is that doctors don’t monitor patients properly. Blame the system, not the drugs. And don’t act like switching to metoprolol is some miracle cure-what if you have atrial fibrillation? Then metoprolol kills you faster. This article is fearmongering dressed as medicine.
Wait… so you’re telling me… that… drugs… can… have… side effects?? Oh my god. I’m shaking. I’ve been taking Zyrtec for my allergies and now I’m terrified I’m going to wake up one day and my lungs will have… betrayed me. Also, I read somewhere that ACE inhibitors cause coughing? So… is that why my neighbor coughs all the time? Is he secretly a COPD patient? Is he being poisoned by his blood pressure med? I need to call the FDA.
Wow. Just… wow. You’re telling me Americans are too lazy to manage their own health? We need a pharmacist to babysit our meds? In my day, people didn’t need a 10-step plan to take a pill. We just took it. Now we’re all walking around with brown bags like we’re packing for a 3-month survival trip. What happened to personal responsibility? This is why the US is collapsing.
I’ve been on Ambien for 7 years. I don’t sleep without it. I tried melatonin. It made me feel like I was floating through a dream where the government was whispering to me in Latin. I don’t trust this article. I don’t trust the CDC. I don’t trust the WHO. I trust my body. And my body says: ‘Give me the pill.’ If I stop, I’ll die. And if I die, someone will say ‘I told you so.’ I just want to sleep. 😔
Do the brown bag review. It’s simple. Take everything you take to your pharmacist. Ask the three questions. Don’t wait for a crisis. This isn’t complicated. You don’t need a PhD to save your lungs. Just show up. Be honest. Be proactive. Your life depends on it.
EVERYTHING IS A CONSPIRACY. They put fluoride in the water so we forget how to breathe. They make beta-blockers so we forget our own names. They give us Ambien so we don’t wake up screaming about the truth. I used to be fine until I started taking Claritin. Now I can’t even blink without feeling like my lungs are being held underwater. I know what they’re doing. They want us to die quietly. So they can charge more for oxygen tanks.
Just switched from propranolol to metoprolol last month… my oxygen saturation went from 88% to 94% in 3 weeks. I’m not a doctor, but I know what feels right. 🙏 Also, I started using a humidifier and it’s like my lungs finally said ‘thank you.’ You’re not alone. Small changes matter. 💙
My cousin in Delhi died last year because his doctor gave him diphenhydramine for his cold. He had COPD. He didn’t know. He just wanted to sleep. He never woke up. Now I check every pill label like it’s a bomb. I don’t care if it’s ‘over the counter.’ If it says ‘may cause drowsiness,’ I avoid it. This isn’t just advice-it’s survival. I’m not angry. I’m just tired of burying people who didn’t have to die.
I’ve been a COPD patient for 15 years. I’ve been on everything on this list at some point. The hardest part wasn’t the meds-it was the guilt. I felt like I was failing because I needed help. But this article? It doesn’t shame you. It empowers you. Thank you for writing this. I’m printing it out and giving it to my brother. He’s still on Xanax. He needs to see this.
Let’s get real for a second. This isn’t just about avoiding bad drugs-it’s about reclaiming agency. COPD isn’t just a lung disease; it’s a systemic betrayal by a medical system that treats symptoms, not people. You’re not just a patient-you’re a whole human being with a history, a family, and a right to breathe without fear. That’s why the brown bag review isn’t a chore-it’s an act of rebellion. You’re not asking for permission. You’re taking back your breath. And that? That’s powerful. I’ve seen it change lives. Not because of magic pills-but because someone finally asked, ‘What are you really taking?’ And then listened.
Oh, so now we’re blaming the medication? What about the fact that people with COPD smoke for 40 years, eat fast food, never exercise, and then wonder why they can’t breathe? You think a pill swap is going to fix decades of neglect? The real problem is that people want a quick fix for a lifestyle disaster. I’ve seen patients on 15 different medications, still smoking, still drinking, still sitting on the couch watching TV. You can’t medicate away poor choices. This article is like giving a parachute to someone who jumped out of a plane because they didn’t want to climb the stairs. The problem isn’t the fall-it’s the jump.