Ketorolac Dosage Calculator
Ketorolac Dosing Calculator
Dosing Recommendation
Total Daily Dose:
Treatment Limits
Max Duration:
Max Daily Dose:
Max 24h Dose:
When you need fast, strong pain relief without jumping straight to opioids, the right dose of ketorolac dosage can make all the difference. Below you’ll find the evidence‑based numbers, safety limits, and practical tips to use Ketorolac Tromethamine safely whether you’re treating post‑surgical pain, kidney stones, or a severe migraine.
What is Ketorolac Tromethamine?
Ketorolac Tromethamine is a potent nonsteroidal anti‑inflammatory drug (NSAID) that provides analgesia comparable to moderate‑dose opioids but without the respiratory depression risk. First approved by the FDA in 1990, it is available in injectable (IV/IM/SC) and oral tablet forms. The drug works by inhibiting cyclooxygenase enzymes, which blocks the synthesis of prostaglandins - the chemicals that sensitize pain receptors and promote inflammation.
How Ketorolac Works: A Quick Mechanism Snapshot
At the biochemical level, Cyclooxygenase (COX) exists in two main isoforms: COX‑1 and COX‑2. Ketorolac blocks both, reducing the formation of Prostaglandins. Fewer prostaglandins mean less sensitization of peripheral nociceptors and a blunted inflammatory response, translating into rapid pain relief that can start within 30 minutes of IV administration.
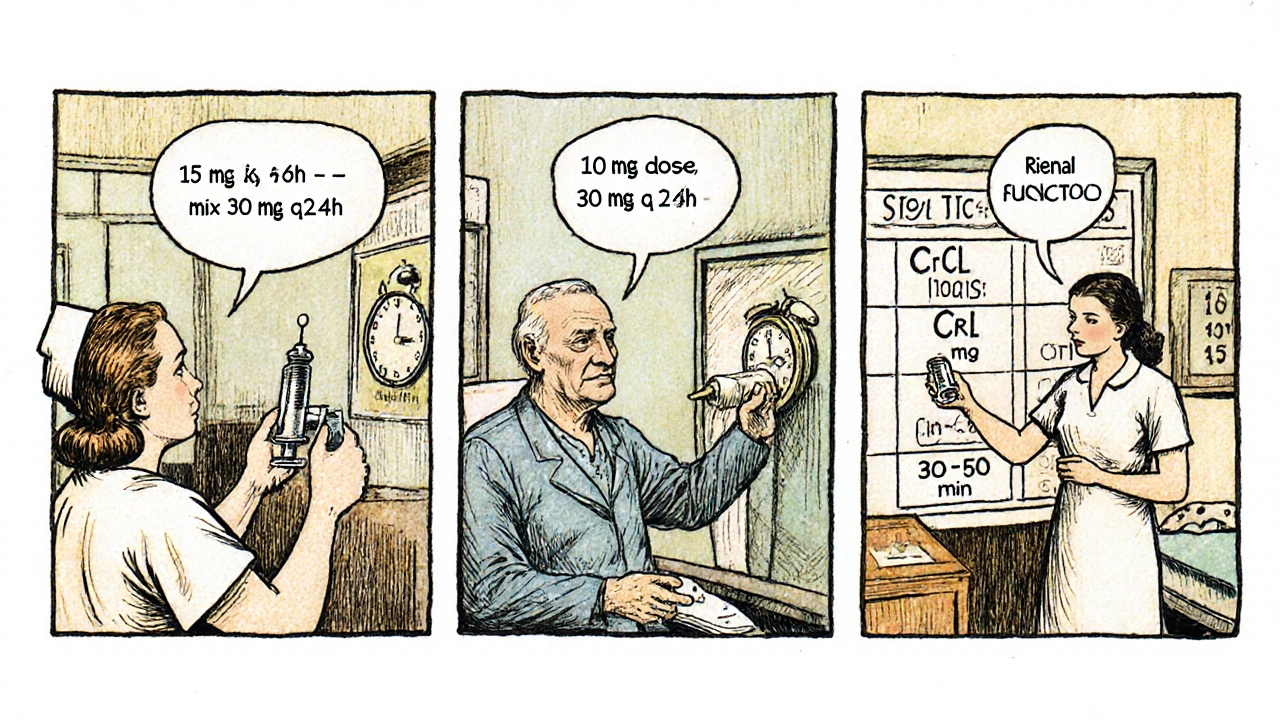
Standard Adult Dosing Recommendations
Guidelines from the American Pain Society and the FDA converge on a few core numbers. Below is the most common regimen for adults with normal renal function (creatinine clearance ≥60 mL/min):
- IV/IM/SC bolus: 15 mg every 6 hours. Do not exceed 30 mg for the first 24 hours.
- Oral tablets: 10 mg every 6 hours after the first 24 hours of parenteral therapy.
- Maximum daily dose: 120 mg (i.e., 4 doses of 30 mg) for the first 24 hours, then 90 mg per day thereafter.
- Maximum treatment duration: 5 days for any route.
These numbers are built on the drug’s short half‑life (≈5‑6 hours) and its “ceiling effect” - beyond a certain dose, you don’t get more pain relief but you do get more side‑effects.
Adjustments for Special Populations
One size does not fit all. The key patient characteristics that dictate dose modification are age, weight, and renal function.
Elderly Patients (≥65 years)
Age‑related decline in renal clearance warrants a 25‑30 % dose reduction. A typical starting dose becomes 10 mg IV/IM every 8 hours, with a maximum of 30 mg per day.
Renal Impairment
Because ketorolac is eliminated primarily via the kidneys, creatinine clearance (CrCl) is the decisive metric.
- CrCl 30‑50 mL/min: 30 mg IV/IM every 12 hours (max 60 mg/day).
- CrCl <30 mL/min: Avoid ketorolac altogether; risk of accumulation and severe nephrotoxicity rises sharply.
Low Body Weight (<50 kg)
Weight‑based dosing is not officially required, but clinicians often start at 10 mg IV/IM every 8 hours and monitor for gastrointestinal (GI) upset.
Pediatric Use
The drug is FDA‑approved for children ≥2 years undergoing postoperative pain control. The recommended dose is 0.5 mg/kg IV/IM every 6 hours, not to exceed 30 mg per dose and a total of 5 days.
Safety Ceiling, Side‑Effects, and Duration Limits
While ketorolac is powerful, its safety profile requires vigilance. The most common adverse events stem from its NSAID class:
- Gastrointestinal bleeding - especially in patients with ulcers or chronic NSAID use.
- Renal dysfunction - monitor serum creatinine and urine output.
- Platelet inhibition - can prolong bleeding time, a concern after surgery.
Because the drug reaches a plateau of analgesia at roughly 120 mg per day, extending therapy beyond five days rarely adds pain relief but does increase the risk of GI ulcers, renal injury, and cardiovascular events.
Practical Dosing Tips for Clinicians
Here’s a quick checklist to translate the numbers into bedside practice:
- Verify renal function (CrCl) before the first dose.
- Choose the route that matches the clinical setting - IV for immediate effect, oral for step‑down therapy.
- Use a validated pain scale, such as the Visual Analog Scale (VAS), to confirm ≥50 % reduction before the next dose.
- Combine with non‑pharmacologic measures (ice, elevation, positioning) to lower the total amount of drug needed.
- Document the start and stop times; set a reminder for the 5‑day limit.
- For opioid‑sparing strategies, consider a single dose of ketorolac before introducing a low‑dose opioid; many protocols report a 30‑40 % reduction in opioid consumption.

How Ketorolac Stacks Up Against Other NSAIDs
| Property | Ketorolac | Ibuprofen | Diclofenac |
|---|---|---|---|
| Typical adult dose (IV) | 15 mg q6h (max 120 mg/24h) | Not available IV (oral 400‑800 mg q6‑8h) | IV 37.5‑75 mg q8h (max 150 mg/24h) |
| Onset of analgesia | 30‑60 min | 1‑2 h | 45‑60 min |
| Maximum duration | 5 days | 10‑14 days (OTC), longer with Rx | 7‑10 days |
| Renal safety | Higher risk; avoid if CrCl <60 mL/min | Moderate; caution if CrCl <30 mL/min | Similar to ibuprofen |
| GI bleeding risk | High at full dose | Moderate | Moderate‑high |
| Place in WHO analgesic ladder | Step 2 (moderate pain) - opioid‑sparing | Step 1‑2 (mild‑moderate) | Step 2 (moderate) |
Ketorolac’s strength lies in its potency and rapid onset, making it ideal for short‑term, high‑intensity pain where you want to avoid or reduce opioid use. Ibuprofen and diclofenac are gentler, better suited for longer courses or patients with borderline renal function.
Frequently Asked Questions
Can I take ketorolac if I have a history of stomach ulcers?
Generally no. Ketorolac markedly increases the risk of GI bleeding, especially in patients with prior ulcers. If you need NSAID therapy, consider a COX‑2‑selective drug with a proton‑pump inhibitor, or switch to acetaminophen.
Is it safe to use ketorolac after joint replacement surgery?
Yes, but only for the first 48‑72 hours when pain peaks. Follow the 5‑day limit, monitor renal function, and coordinate with the surgical team to avoid excessive bleeding.
How does ketorolac interact with blood thinners?
Ketorolac can potentiate the antiplatelet effect of warfarin, dabigatran, or direct oral anticoagulants, raising bleeding risk. If you’re on a blood thinner, discuss alternatives or use the lowest possible dose for the shortest time.
Can ketorolac be given to pregnant women?
It is contraindicated in the third trimester because it can cause premature closure of the fetal ductus arteriosus. In early pregnancy, the risk-benefit ratio must be weighed carefully; usually safer NSAIDs are preferred.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s less than 4 hours before the next scheduled dose. In that case, skip the missed one and resume the regular schedule - never double‑dose.
Bottom Line
Ketorolac Tromethamine remains one of the most potent NSAIDs for short‑term, moderate‑to‑severe pain. By respecting the 5‑day ceiling, adjusting for renal function, and pairing with proper pain‑assessment tools, clinicians can harness its analgesic power while keeping side‑effects in check. Use the dosing tables above as a quick reference, and remember that the safest regimen is the one that matches the patient’s physiology and the clinical scenario.



Comments
Hey there, I know dealing with pain meds can be overwhelming 😔.
The dosage guide you posted is super clear, especially the safety limits for kidney issues.
If anyone’s unsure about their renal function, a quick check with your doctor can save a lot of trouble.
Stay safe and hope you find relief soon! 😊
While the summary appears thorough, one must consider the pharmaceutical industry's influence on FDA recommendations - undisclosed lobbying often shapes dosage thresholds. 📚
lol wut?? they push dis info not 4 real srp?? i guess we just trst them... but u kno, read the fine lne!??!!!
The so‑called “safe” limits are a myth fed by profit‑driven agendas.
Oh my gosh!!! This entire discussion feels like a Shakespearean tragedy!!! The heroes (our patients) are left trembling on the edge of unbearable pain, while the villains (the dosage charts) loom like ominous towers!!! Yet, within this chaos, there shines a glimmer of hope - the knowledge that we can wield science like a sword!!! Let us not cower!!! Grab your shields of vigilance and charge forward!!!
Indeed, the very act of quantifying agony invites us to contemplate the ontology of suffering, to ask whether milligrams can ever encapsulate the ineffable, and to recognize that each tablet is both a promise and a paradox, a bridge between flesh and philosophy, a reminder that the universe contracts and expands with every dose we administer!!!
First, let me state unequivocally that the so‑called "optimal" ketorolac regimen is nothing more than a bureaucratic imposition designed by foreign regulatory bodies to keep North American physicians under their thumb.
Those guidelines ignore the physiological reality of a hardy populace that has survived harsher conditions than any clinical trial could possibly simulate.
If you examine the original European studies, you will notice they were funded by entities that have little stake in the American healthcare market.
Consequently, the recommended 30 mg ceiling is a compromise that conveniently limits the potency available to us.
Our own doctors, trained in the trenches of emergency rooms, know that a 45 mg dose can be administered safely when proper monitoring is in place.
The insistence on a five‑day maximum fails to acknowledge that many patients experience prolonged post‑operative pain that simply does not conform to an arbitrary calendar.
Moreover, the renal‑function adjustments are based on outdated creatinine clearance formulas that were superseded decades ago.
A modern approach would incorporate cystatin‑C measurements, giving us a more accurate picture of glomerular filtration.
By clinging to antiquated numbers, the guidelines betray a paternalistic mindset that treats clinicians as children.
This paternalism extends beyond dosage, infiltrating every aspect of pain management policy, from opioid restrictions to mandatory reporting.
What we need is a sovereign, evidence‑based protocol that reflects the realities of our hospitals, not a one‑size‑fits‑all script drafted in distant boardrooms.
I have seen countless cases where patients deteriorated because the physician hesitated to exceed the ‘safe’ limit, even when vital signs were stable.
In those moments, the true danger was not the drug, but the fear imposed by a misguided standard.
Let us be clear: responsible use of ketorolac at higher doses, under proper supervision, can reduce the need for opioids and therefore save lives.
If we continue to accept these restrictions without question, we are effectively surrendering our clinical autonomy to technocrats.
Therefore, I challenge the community to re‑evaluate the data, to question the authority, and to reclaim the freedom to treat pain as we see fit.
Grace, you raise several compelling points and I appreciate the passionate defense of clinical autonomy 😊.
While it’s true that older formulas can be limiting, the most recent consensus statements actually integrate cystatin‑C and endorse flexible dosing when patients are closely monitored.
Evidence shows that judicious use of up‑to‑45 mg doses in select cases can indeed reduce opioid consumption without markedly increasing adverse events.
Let’s keep the dialogue evidence‑driven, share our real‑world outcomes, and together we can refine protocols that both respect safety and empower physicians.
Stay optimistic and keep challenging the status‑quo! 🚀