Medication Review Tool
Medication Review
This tool helps identify medications that may be inappropriate for older adults based on evidence-based guidelines. Always consult your healthcare provider before making any medication changes.
Deprescribing Assessment
Current Medications
0 medicationsEvery year, millions of older adults take more medications than they need. Some of these drugs were prescribed years ago for conditions that no longer exist. Others were meant to be temporary but became permanent. And many of them are causing more harm than good. This isn’t laziness or neglect-it’s a systemic problem called polypharmacy. When someone takes five or more medications, their risk of side effects, falls, confusion, and hospitalization jumps dramatically. The solution isn’t always adding more pills. Sometimes, it’s taking them away.
What Is Deprescribing?
Deprescribing isn’t just stopping a pill. It’s a careful, step-by-step process of reviewing every medication a person takes and deciding which ones can be safely reduced or stopped. It’s not about cutting corners. It’s about doing the opposite: being more thoughtful. The goal? Reduce side effects, improve quality of life, and avoid unnecessary risks-all without leaving health conditions untreated. This approach became formalized around 2012, led by researchers in Canada like Barbara Farrell and Cara Tannenbaum. Today, deprescribing.org is the go-to resource for evidence-based guidelines. These aren’t opinions. They’re clinical protocols built on systematic reviews and real-world trials. And they’re backed by data: a 2023 study in JAMA Internal Medicine showed that when older adults had medications carefully reduced, their risk of side effects dropped-with no increase in hospitalizations or deaths.Why Do People Take Too Many Medications?
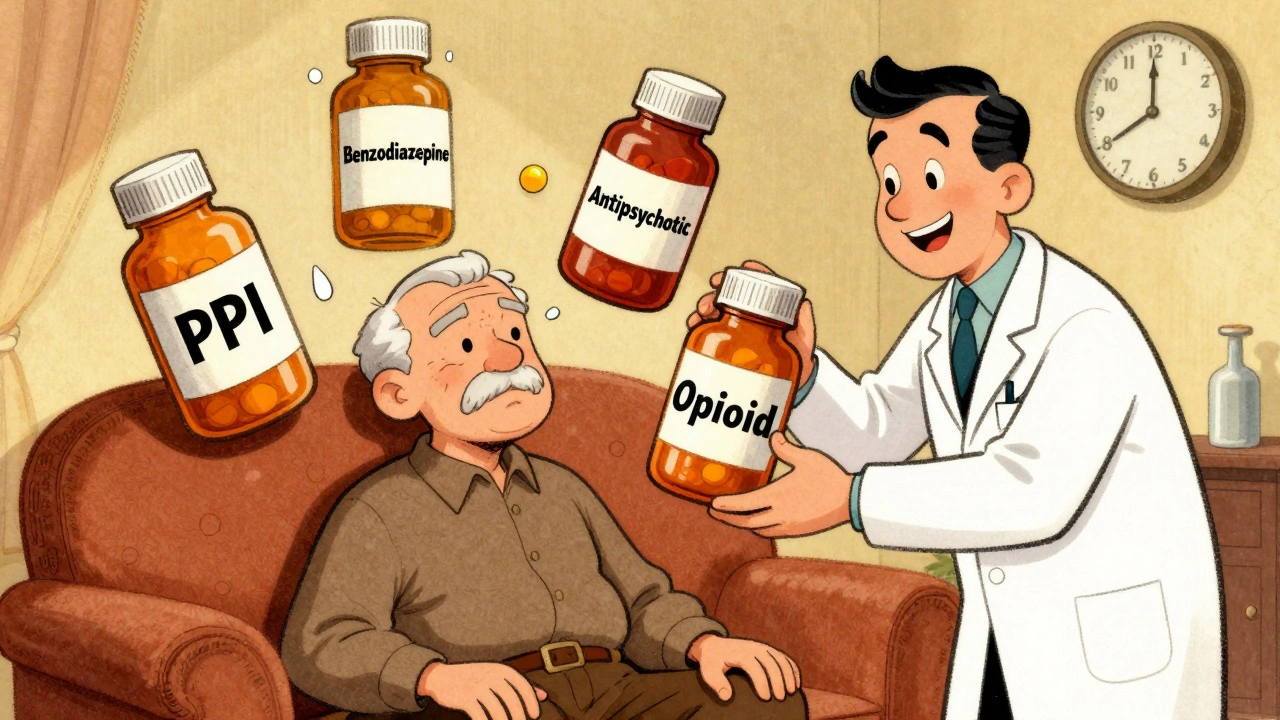
It’s not because doctors are careless. The problem is structural. A patient sees a cardiologist, a rheumatologist, a neurologist, and a primary care doctor. Each one prescribes what they think is best for their specialty. No one steps back to look at the full picture. Over time, medications pile up. Some become redundant. Others lose their purpose. A proton-pump inhibitor (PPI) for occasional heartburn becomes a daily habit. A benzodiazepine for short-term anxiety turns into a long-term sleep aid. An antipsychotic for agitation in dementia gets carried forward even after symptoms fade. The World Health Organization reports that nearly 40% of older adults globally are taking potentially inappropriate medications. In hospitals and nursing homes, up to 30% of admissions in people over 65 are linked to medication harm. That’s not just a health issue-it’s a safety crisis.Which Medications Are Most Often Deprescribed?
Not all drugs are equal when it comes to risk. Five medication classes have clear, evidence-based deprescribing guidelines:- Proton-pump inhibitors (PPIs) - Often prescribed for heartburn, but long-term use increases risk of bone fractures, kidney disease, and infections. Many people don’t need them after 4-8 weeks.
- Benzodiazepines and sleep meds (BZRAs) - These can cause dizziness, confusion, and falls. The risk rises with age. Tapering over weeks reduces withdrawal symptoms and improves balance.
- Antipsychotics - Used off-label for dementia-related agitation. Studies show they increase stroke risk and death. Non-drug approaches often work better.
- Antihyperglycemics - Blood sugar drugs like sulfonylureas can cause dangerous lows in older adults. Tight control isn’t always better, especially with limited life expectancy.
- Opioid analgesics - Long-term use for chronic pain increases tolerance, dependence, and overdose risk. Alternatives like physical therapy or low-dose antidepressants often help more safely.
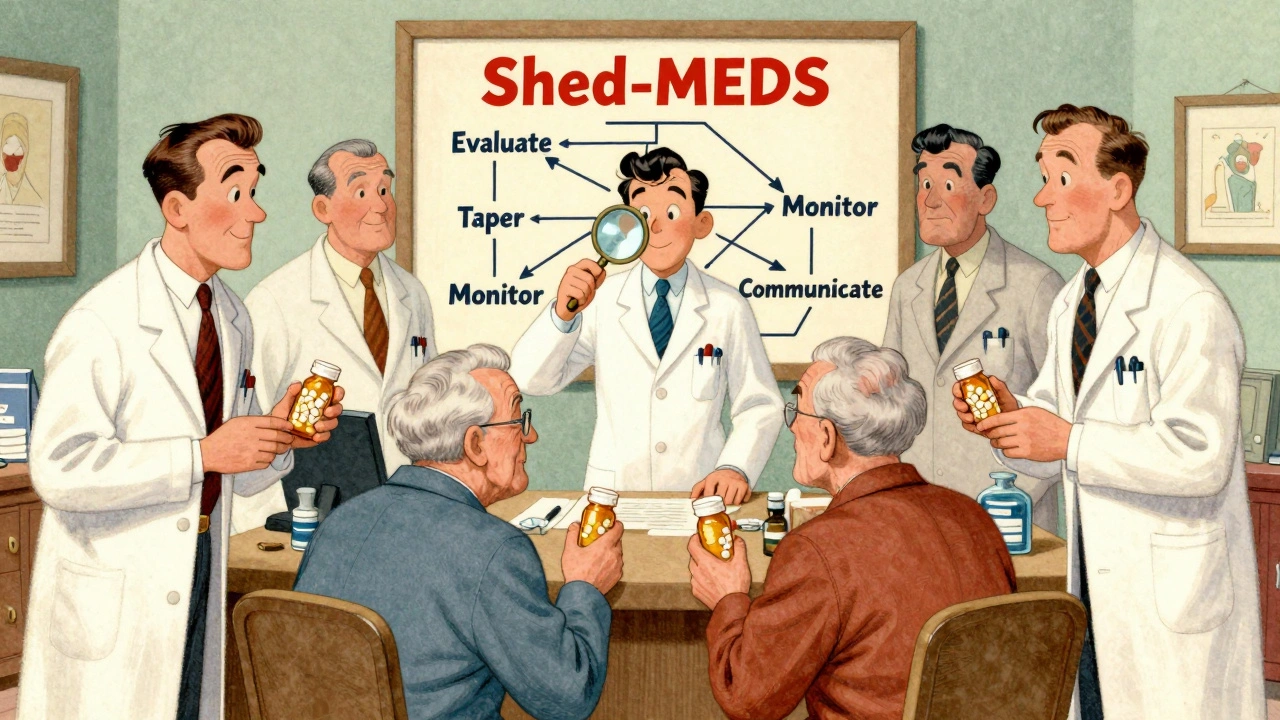
How Do You Actually Do It? The Shed-MEDS Framework
One of the most validated tools is the Shed-MEDS framework. It’s simple, practical, and proven in clinical trials:- Best Possible Medication History - Get a full list of everything the patient takes, including over-the-counter pills, supplements, and creams. Don’t trust memory. Check pharmacy records.
- Evaluate - For each drug, ask: Is it still needed? Is it working? Is it causing harm? Is there a safer alternative? Use tools like the Beers Criteria or STOPP/START guidelines.
- Deprescribing Recommendations - Prioritize drugs with the highest risk and lowest benefit. Start with one. Don’t try to change everything at once.
- Synthesis - Document the plan, share it with the patient and other providers, and schedule follow-up. Make sure the patient understands why and how.
Who Should Be Leading This?
Deprescribing doesn’t work in a vacuum. It needs teamwork. Pharmacists are the unsung heroes here. In settings where pharmacists lead the review-like in nursing homes or hospital discharge teams-medication reductions are 35-40% higher than in clinics without them. Why? Because pharmacists have the training. They know drug interactions. They understand tapering schedules. They can spot red flags others miss. But in most primary care offices, doctors have just 7-8 minutes per visit. That’s not enough time to review 12 medications, explain why one might be stopped, and address patient fears. That’s why successful programs include:- Pharmacists trained in medication therapy management (150+ hours of specialized training)
- Physician champions who advocate for deprescribing
- Nurses who monitor for withdrawal symptoms like anxiety, insomnia, or rebound pain
- Electronic health records that flag high-risk prescriptions and suggest alternatives
What About Patient Fear?
Stopping a medication can scare people. Especially if they’ve taken it for 10 or 20 years. “This pill keeps me alive,” they say. But often, it’s just keeping them from feeling worse-while making them feel worse in other ways. A 2022 study found that 65% of older adults felt relieved after reducing their pill burden. But 22% were anxious. They worried about symptoms coming back. Or worse-dying. That’s why communication matters more than the protocol. You can’t just hand someone a taper schedule. You need to explain:- Why this drug might not be helping anymore
- What signs to watch for
- How to get help if something goes wrong
- That stopping isn’t failure-it’s progress
What’s Holding Deprescribing Back?
Even with strong evidence, adoption is slow. Why?- Guidelines are fragmented. Out of 3,569 recommendations in clinical guidelines, only 7% mention deprescribing. Most focus on adding drugs, not removing them.
- Electronic health records don’t help. Only 32% of clinicians feel their EHR supports deprescribing. Most systems are designed to prompt prescribing, not deprescribing.
- Time is scarce. Primary care visits are too short. Shared decision-making takes 20-30 minutes-not 7.
- There’s no reimbursement. Insurance doesn’t pay for medication reviews. Pharmacists can’t bill for them. Doctors aren’t rewarded for stopping drugs.
- Doctors fear lawsuits. “What if they get worse?” is a real concern-even if the evidence says they’re more likely to get better.
What’s Next?
The future of deprescribing is digital. Researchers are building AI tools that scan EHRs and flag medications that should be reviewed. The NIH has funded projects to create guidelines for antidepressants, anticoagulants, and other classes that currently lack clear protocols. By 2030, experts predict deprescribing assessments will be as routine as checking blood pressure. That’s not a fantasy. It’s inevitable. With 1 in 6 people globally expected to be over 65 by 2030, we can’t keep treating aging like a disease to be medicated into submission. The real breakthrough won’t come from a new drug. It’ll come from a new mindset: that less can be more. That safety isn’t just about preventing disease-it’s about preventing harm from the very treatments meant to help.Where to Start
If you’re a patient or caregiver:- Ask your doctor: “Are all these medications still necessary?”
- Bring a full list-every pill, patch, and supplement.
- Ask: “What happens if I stop this one?”
- Don’t stop anything on your own. Tapering safely matters.
- Use deprescribing.org’s free algorithms.
- Start with one class-PPIs or sleep meds are easiest.
- Partner with your pharmacy team.
- Document your decisions. It protects you and helps future care.
Key Tools and Resources
- deprescribing.org - Free, evidence-based guidelines for five drug classes.
- STOPP/START Criteria (Version 3, 2021) - Tools to identify potentially inappropriate prescribing and missed treatments.
- Beers Criteria (2023 Update) - Lists 34 medications to avoid in older adults.
- Shed-MEDS Framework - Proven 4-step process for clinical teams.





Comments
Been using the Shed-MEDS framework in my rehab unit for a year now and it’s a game-changer. We started with PPIs and benzodiazepines-cut meds by 2.1 per patient on average. No spikes in ER visits. Patients sleep better, walk steadier, and actually remember their grandkids’ names. Pharmacists are the real MVPs here. Give them time, give them authority, and watch the magic happen. 🙌
Oh, another neoliberal technocratic solution to the structural collapse of geriatric care. Deprescribing? How quaint. We’ve reduced complex human beings to algorithmic pharmacokinetic variables. The real crisis isn’t polypharmacy-it’s the commodification of aging under late-stage capitalism. You can’t deprescribe the neoliberal condition with a checklist. 🤡
I’ve been on 14 pills for 17 years. My doctor says I can stop 6. But I’m terrified. What if I die? What if I wake up and my heart just stops? I don’t want to be one of those statistics. I just want to live. Please tell me it’s safe. I’m so scared.
Deprescribing is the ultimate epistemic humility maneuver. You’re not just reducing polypharmacy-you’re rejecting the hegemony of biomedical reductionism. The Shed-MEDS framework is essentially a Foucauldian biopolitical intervention: reclaiming agency from the pharmaceutical-industrial complex. The real innovation? It’s not clinical-it’s ontological. We’re not just weaning off pills; we’re weaning off the myth of medical omnipotence.
My mom took 11 meds. We stopped 5. She cried for two weeks. Then she started gardening again. She said, ‘I didn’t know I could feel my toes.’ I wish I’d done this sooner. I feel guilty for not asking earlier. I’m so sorry, Mom.
Western medicine has become a temple of pharmaceutical dogma. In India, our elders use turmeric, yoga, and Ayurveda. We don’t need 12 pills to manage ‘chronic inflammation.’ Deprescribing is just the West finally catching up to what ancient systems knew: less is more. But you still won’t fix the root problem: the profit motive in drug development.
My dad’s doctor just told him to stop his statin. He was scared too. We sat down with the pharmacist. She showed him the data. Said his risk of heart attack was lower than his risk of falling from dizziness. He’s been off it for 3 months. No chest pain. And he’s walking his dog every morning. That’s all that matters. Just talk to someone who knows the meds.
My grandma’s on 8 meds. We’re starting with the PPI. She says she’s been taking it since 2010 for ‘a little heartburn.’ Turns out she hasn’t had heartburn since 2012. We’re all shocked. 🤯 But we’re doing it slow. Pharmacist gave us a chart. I’m so proud of us for even trying.
People think stopping meds is dangerous but honestly most of these pills are just placebo with side effects. My uncle took 12 pills and could barely walk. Cut it to 3. Now he’s playing golf. Who’s the real danger here? The doctor who prescribed it or the system that lets it happen? 🤷♂️
My mom’s on 11. I asked if she needed them all. She said yes. I didn’t push. I’m not her doctor.
It’s not just about the drugs. It’s about the ritual. For so many older people, their meds are a routine that gives structure to their day. The pillbox is their calendar. The pharmacist’s voice on the phone is their only human interaction. When you take away the pills, you have to replace the meaning. You can’t just say ‘stop this’ and expect them to be fine. You need to sit with them. Listen. Offer walks. Offer tea. Offer presence. The deprescribing protocol is just the first step. The real work is relational. And that’s the part no one funds. No one bills for. No one measures. But it’s the only thing that matters.
Let me guess-you’re one of those people who thinks ‘less is more’ and believes doctors are just pill-pushers. Newsflash: not everyone has the luxury of being healthy enough to stop meds. Some of us need every single one. Don’t act like you know better because you read a blog post. This isn’t a wellness trend. It’s medicine. And it’s complicated.
While the empirical data presented is statistically significant, the underlying epistemological framework remains dangerously reductionist. The deprescribing paradigm assumes a homogenous geriatric population with linear pharmacodynamic responses, which is patently false. The conflation of statistical outcomes with clinical wisdom ignores heterogeneity in frailty, comorbidity burden, and psychosocial determinants. Furthermore, the reliance on EHR-based algorithms perpetuates algorithmic bias and undermines clinical autonomy. This is not progress-it is medical automation masquerading as patient-centered care.