Strabismus, often called a squint, happens when your eyes don’t line up properly. One eye might turn inward, outward, upward, or downward while the other looks straight ahead. It’s not just a cosmetic issue-it affects how your brain processes what you see. If left untreated, it can lead to permanent vision problems like lazy eye or loss of depth perception. About 5 out of every 100 children develop it, and it can also show up in adults after a stroke, head injury, or nerve damage.
What Does Strabismus Actually Look Like?
You might notice one eye drifting while the other stays focused. In kids, it’s often noticed when they’re tired or looking at something far away. In adults, it usually comes on suddenly. The misalignment can be constant or come and go. There are four main types:- Esotropia (inward turning)-the most common, making up about half of all cases.
- Exotropia (outward turning)-often appears when a child is daydreaming or looking at distant objects.
- Hypertropia (upward turning) and hypotropia (downward turning)-less common, but can cause head tilting to compensate.
People with strabismus often report double vision, eye strain, headaches, or trouble reading. Kids might squint, close one eye in bright light, or tilt their head. Teachers sometimes notice children losing focus in class-not because they’re distracted, but because their eyes aren’t working together.
Why Does It Happen?
Most cases aren’t caused by weak eye muscles. They’re caused by the brain’s control system. The brain sends signals to the eye muscles to keep both eyes locked on the same spot. If that signal gets mixed up, one eye drifts. In about 30% of childhood cases, there’s a family history-meaning genetics play a role.In adults, the most common triggers are stroke, head trauma, or nerve damage. Paralytic strabismus, which happens when a cranial nerve (usually IV or VI) stops working, causes sudden misalignment, dizziness, and nausea. It’s rare but serious. About 12% of adult-onset cases fall into this category.
Non-Surgical Treatments: First Steps
Before surgery, doctors usually try simpler options. These aren’t just backups-they can work well, especially in kids.- Corrective glasses-if the misalignment is caused by farsightedness, glasses alone can fix it.
- Patching-covering the stronger eye forces the weaker one to work harder, helping prevent lazy eye.
- Vision therapy-a series of exercises designed to train the eyes to work together. Studies show it helps 60% of kids with intermittent exotropia avoid surgery entirely.
These methods work best when started early. A child diagnosed before age 2 has a much better chance of developing normal depth vision if treated quickly. But even older kids and adults can benefit. Vision therapy isn’t magic-it takes weeks of consistent practice, but it’s low-risk and often covered by insurance.
When Is Surgery Necessary?
Surgery isn’t the first choice-but it’s the right one when other treatments don’t work. Doctors recommend it when:- The eye misalignment is constant and more than 15 prism diopters (a unit that measures how far the eye is off).
- Double vision doesn’t go away with prism glasses.
- The person has to tilt their head constantly to see straight.
- There’s a risk of permanent vision loss from amblyopia (lazy eye).
For children with large-angle congenital esotropia, surgery is now recommended as early as 3 to 4 months old-much earlier than before. Research shows that getting the eyes aligned before the brain fully learns to ignore one eye gives the best shot at true binocular vision.
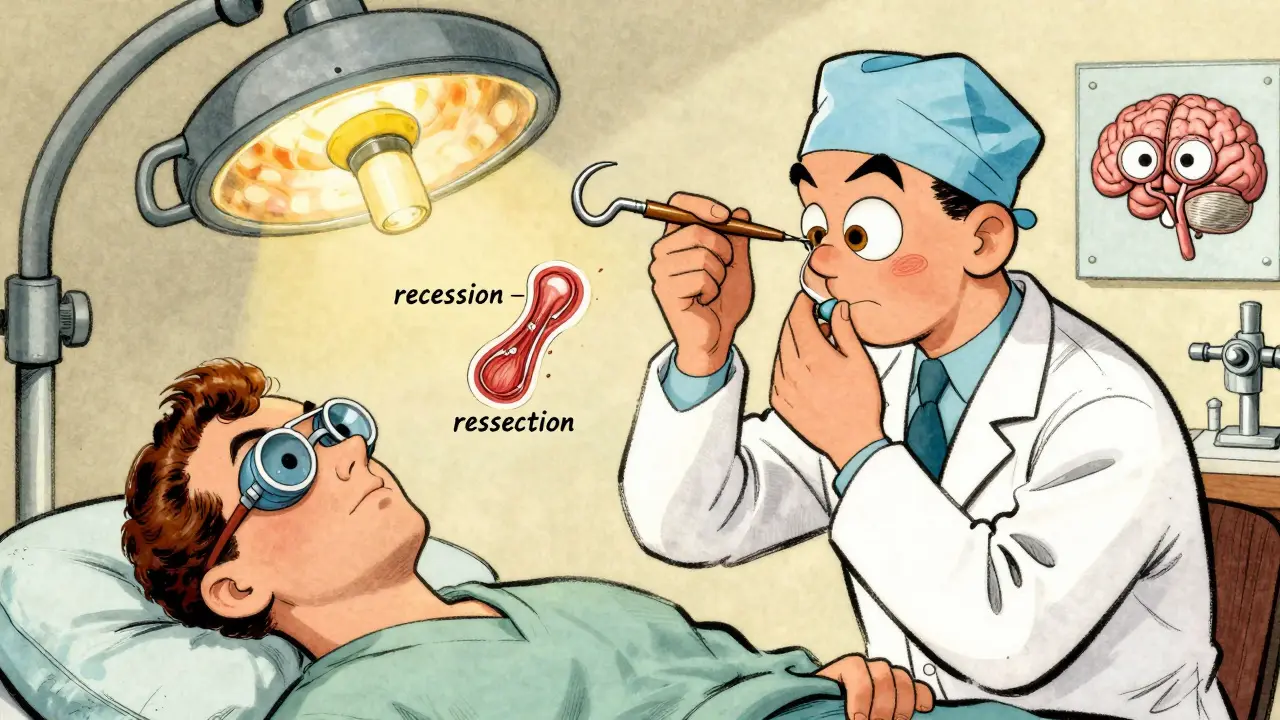
What Happens During Strabismus Surgery?
The surgery doesn’t involve the eyeball itself. It works on the muscles that move the eye. There are two main techniques:- Recession-the surgeon loosens a muscle by moving its attachment point farther back on the eye.
- Resection-the surgeon shortens a muscle to make it stronger.
For inward-turning eyes (esotropia), the most common procedure is a bilateral medial rectus recession. For outward-turning eyes (exotropia), the lateral rectus muscles are adjusted. The surgery takes 45 to 90 minutes, depending on how many muscles need work.
For kids, it’s done under general anesthesia. For adults, it’s usually local anesthesia with sedation. Many surgeons now use adjustable sutures-a technique used in 68% of adult cases. This means the eye’s alignment can be fine-tuned the same day or the next morning, while the patient is awake. That reduces the chance of needing a second surgery.
Success Rates and Risks
Surgery works well-but it’s not perfect. Success is measured by whether the eyes stay aligned within 10 prism diopters of each other.- Children under 2: 75-85% success rate.
- Adults: 55-65% success rate.
- Paralytic strabismus: Only 45% achieve full correction.
Complications are rare but real:
- Undercorrection (20-30% of cases)-the eye still turns, and another surgery may be needed.
- Overcorrection (10-15%)-the eye turns the opposite way.
- Temporary double vision-happens in 80% of patients right after surgery, but usually fades in days or weeks.
- Retinal detachment (0.1%) and endophthalmitis (0.04%)-extremely rare but serious.
One big mistake doctors see is focusing only on how the eyes look-not whether the person can use them together. About 28% of patients are unhappy after surgery, even if the eyes are straight, because their brain still can’t combine the images from both eyes.
Recovery and What Comes After
Recovery isn’t quick. You’ll need eye drops for two weeks. Redness and swelling fade over a few weeks. Most people go back to work or school in 3-7 days, but full healing takes 6-8 weeks.Here’s what most patients need after surgery:
- Follow-up visits at 1 day, 1 week, 3 weeks, and 6 weeks.
- Vision therapy starting 4-6 weeks after surgery-recommended for 85% of cases.
- Regular check-ups for months or even years to catch any drift early.
Patients who get pre-op counseling-knowing what to expect, including possible double vision or the need for more therapy-report 40% higher satisfaction. One Reddit user wrote: “I thought surgery would fix everything. It fixed the alignment, but I still needed months of vision therapy to read without double vision. I wish I’d known that sooner.”
Who Performs the Surgery?
Not all eye doctors do this. Only about 35% of general ophthalmologists are trained in strabismus surgery. The specialists are pediatric ophthalmologists or neuro-ophthalmologists who’ve completed extra fellowship training. They’ve typically supervised 50-75 surgeries before doing them alone.If you’re considering surgery, ask: “Do you specialize in strabismus?” and “How many of these do you do each year?”
What’s New in Strabismus Surgery?
The field is evolving. In 2023, the FDA approved a new tool called the Steger hook, which measures muscle tension down to 0.5 grams. That helps surgeons make more precise adjustments.Virtual reality training before surgery is showing promise. A 2023 study found it improved surgical success by 18% by helping the brain prepare for coordinated eye movement.
Botulinum toxin (Botox) injections are now used in some cases to temporarily weaken a muscle before surgery-cutting the amount of muscle adjustment needed. And robotic-assisted surgery is in early trials at Johns Hopkins, with results showing 32% greater precision in muscle placement.
Cost, Access, and Global Disparities
The global market for strabismus surgery is growing, projected to hit $1.8 billion by 2027. But access isn’t equal. In developed countries, 72% of children with constant strabismus get evaluated by age 5. In developing nations, that number drops to 28%.In the U.S., insurance often requires proof that glasses or vision therapy failed for at least six months before approving surgery. Medicare cut reimbursement by 4.2% in 2023. Private insurers are tightening rules too.
Non-profits like NORA help low-income families cover surgery costs. The National Eye Institute offers free guides on living with strabismus-downloaded over 12,500 times in 2022.
Real Stories, Real Outcomes
On patient forums, the most common feedback is about quality of life:- “I finally made eye contact during meetings without feeling like I was staring weirdly.”
- “I could read a book again after 30 years.”
- “I stopped getting headaches every afternoon.”
Eighty-two percent of patients on review sites say the surgery was “worth it.” But the ones who were happiest didn’t just fix their eyes-they prepared their brains. Vision therapy after surgery made the difference between “I’m aligned” and “I can see properly again.”
Strabismus isn’t just about looks. It’s about how your brain and eyes work together. Surgery can fix the alignment-but true healing often takes time, patience, and follow-up care.
Can strabismus go away on its own?
Rarely. While some mild cases of intermittent exotropia in young children may improve with glasses or vision therapy, true strabismus-where the eye consistently turns-does not resolve without treatment. Left untreated, it can lead to permanent vision loss in one eye (amblyopia) or loss of depth perception.
Is strabismus surgery painful?
The surgery itself isn’t painful because of anesthesia. Afterward, most people feel soreness, like a bruise behind the eye, for a few days. Pain is usually mild and controlled with over-the-counter medicine. The eye may feel scratchy or watery for a week or two. Severe pain is rare and should be reported to your doctor immediately.
Will I need glasses after surgery?
Possibly. Surgery corrects eye alignment but doesn’t fix refractive errors like nearsightedness or farsightedness. Many patients still need glasses for clear vision, especially if they had them before. Some may even need a new prescription after surgery because the eye’s focus has changed slightly.
Can adults benefit from strabismus surgery?
Yes. While children have a better chance of regaining full depth vision, adults often see major improvements in double vision, eye strain, and self-confidence. Many report better performance at work, especially in jobs requiring visual focus like driving, sewing, or computer work. Success rates are lower than in children, but quality-of-life gains are high.
How do I know if I need surgery or just vision therapy?
A comprehensive eye exam by a specialist is key. If your eyes are misaligned most of the time, especially if you have double vision or head tilting, surgery is likely needed. If the misalignment is occasional and you have good vision in both eyes, vision therapy may be enough. Your doctor will measure the angle of misalignment and test your binocular vision to decide.




Comments
Interesting post. In India, many families still think squint is just a phase kids grow out of. We don’t have enough specialists, and vision therapy is seen as ‘alternative medicine.’ But slowly, awareness is growing. My nephew got glasses at 3 and avoided surgery-now he plays cricket without squinting. Small wins matter.
bro i had this and my mom made me wear an eye patch for 6 months like a pirate 😅 it sucked but now i can see in 3d and it’s wild how my brain just… figured it out. also i still hate bright light.
if you think surgery is the answer you’re missing the point. your brain needs to relearn not your eyes. therapy first always. stop treating symptoms like they’re the disease.
my cousin got surgery at 45 and said the biggest change wasn’t how she looked-it was how people looked at her. like, suddenly she wasn’t ‘the weird one who stares off’ anymore. just small things, but they add up.
There’s a deeper metaphysical layer here that most medical literature ignores. Strabismus isn’t merely a misalignment of ocular muscles-it’s a fracture in the unity of perception. The brain, in its attempt to avoid cognitive dissonance, suppresses input from one eye, not because it must, but because it chooses to. We live in a world that rewards binocular harmony, yet the mind, in its solitude, often prefers the quiet of monocular vision. Is strabismus a defect-or a quiet rebellion against the pressure to see the world as everyone else does?
Let’s be real: 68% of adults get adjustable sutures? That’s not innovation-that’s just surgeons admitting they can’t do it right the first time. And 55-65% success rate in adults? That’s a 45% failure rate. You’re paying thousands to have a 1 in 2 chance of still needing another surgery. And don’t get me started on the insurance gatekeeping. This whole system is rigged to profit off desperation.
They never tell you the truth about the Steger hook. It’s not FDA-approved for precision-it’s a Trojan horse. The real tech is the AI algorithm that predicts muscle tension before the cut. They’re using military-grade neural net modeling from DARPA to predict how your eye will drift after surgery. And the VR training? It’s not just for surgeons-it’s for your brain. They’re pre-loading your visual cortex with synthetic binocular data. This isn’t medicine anymore. It’s neuro-engineering. And no one’s asking who’s controlling the simulation.
Strabismus surgery success depends heavily on surgeon specialization. Seek out pediatric ophthalmologists with fellowship training. Ask for annual volume. Avoid general ophthalmologists unless they have proven experience.
you guys are overthinking this. i got the surgery at 32, did therapy for 6 months, and now i can read without headaches. it’s not magic, but it’s worth it. just don’t skip the aftercare. that’s where people give up. keep going. you got this 💪👁️
I’ve been living with intermittent exotropia for 20 years. I never had surgery. I wear glasses, do basic eye exercises, and learned to tilt my head just right. It’s not perfect, but it’s mine. I wonder if the pressure to ‘fix’ everything isn’t just medical-it’s cultural. What if some of us aren’t broken, just different?