Folate Deficiency Risk Calculator
This calculator estimates your risk of folate deficiency and its potential impact on heart health based on key lifestyle and medical factors.
Your Risk Assessment
When your body lacks folate deficiency is a condition where blood levels of the B‑vitamin folate (also called vitamin B9) fall below the normal range, impairing many metabolic processes, your heart may silently pay the price.
Quick Takeaways
- Low folate raises homocysteine, a molecule that damages blood vessels.
- Elevated homocysteine is linked to hypertension, heart attacks, and strokes.
- Symptoms of deficiency are subtle - fatigue, mood changes, and occasional numbness.
- Simple blood tests (serum folate) reveal a shortfall before serious damage occurs.
- Leafy greens, legumes, and fortified foods can restore healthy levels; supplements work fast when needed.
What Is Folate Deficiency?
Folate lives in the bloodstream as folic acid (synthetic) or natural folate. Your body uses it to create DNA, repair cells, and, crucially, convert the amino acid homocysteine into methionine - a building block for proteins. When folate is scarce, that conversion stalls, and homocysteine builds up.
Risk factors include poor diet, excessive alcohol, certain medications (e.g., methotrexate), and genetic variants like MTHFR that limit folate processing.
Why Folate Matters for the Heart
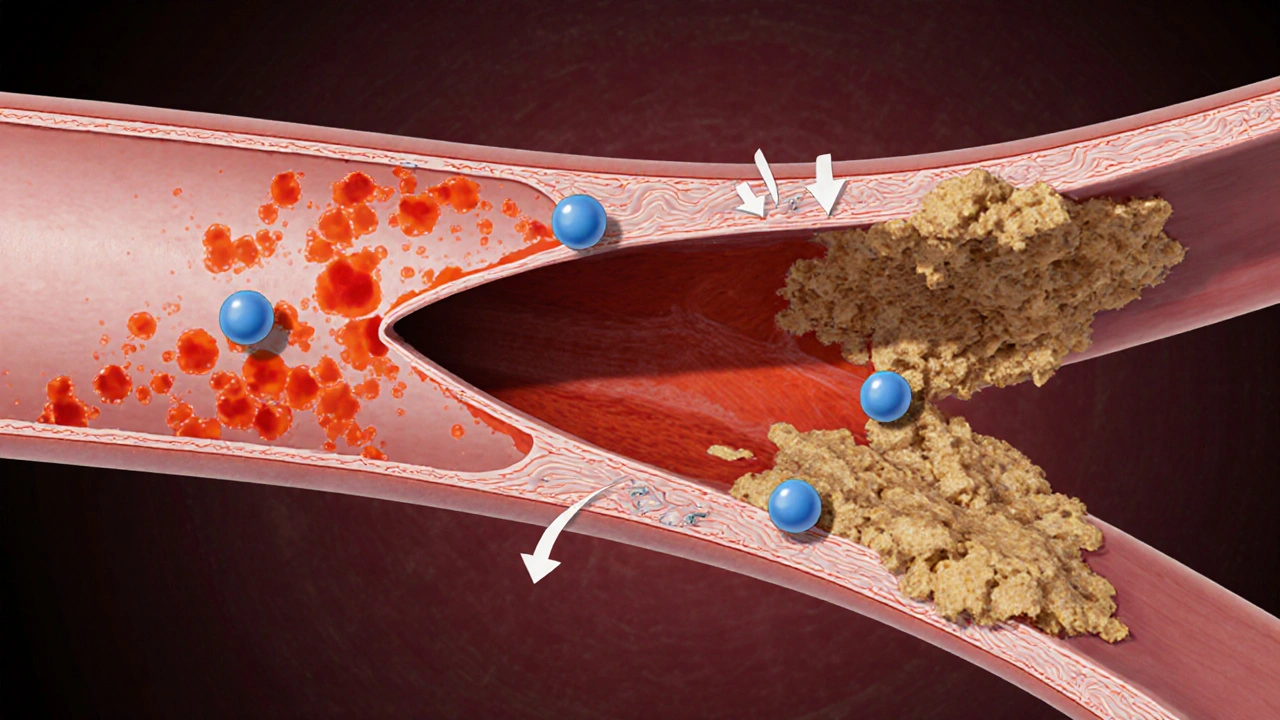
Enter homocysteine an amino acid that, at high levels, irritates the inner lining of blood vessels. When homocysteine spikes, it triggers oxidative stress, inflammation, and clot formation - all ingredients for cardiovascular disease.
Studies from the American Heart Association (2023) show that each 5µmol/L increase in homocysteine raises coronary artery disease risk by roughly 20%. The chain reaction is simple: low folate → high homocysteine → endothelial dysfunction → plaque buildup → heart trouble.
How Low Folate Increases Specific Cardiovascular Risks
1. Endothelial dysfunction - The endothelium (the thin lining of arteries) relies on nitric oxide to stay relaxed. Homocysteine reduces nitric oxide availability, causing vessels to stiffen.
2. Hypertension - Elevated homocysteine promotes arterial wall thickening, increasing resistance and blood pressure. A 2022 meta‑analysis linked folate supplementation to an average 3mmHg drop in systolic pressure.
3. Heart attack and coronary artery disease - Plaque‑forming cholesterol sticks more readily to damaged endothelium, accelerating atherosclerosis.
4. Stroke - Small clots formed from homocysteine‑induced platelet aggregation can travel to the brain, causing ischemic strokes. Research in Europe (2024) found that patients with folate deficiency had a 30% higher odds of first‑time stroke.
Recognizing the Signs of Deficiency
Folate shortage rarely announces itself with dramatic heart symptoms. Instead, watch for:
- Unexplained fatigue or shortness of breath
- Mood swings, irritability, or mild depression
- Glossy, sore tongue (glossitis)
- Occasional numbness or tingling in hands and feet
- Elevated heart rate without exertion (a subtle clue of vascular strain)
If you notice several of these, especially alongside a family history of heart disease, a check‑up is wise.
Testing & Diagnosis
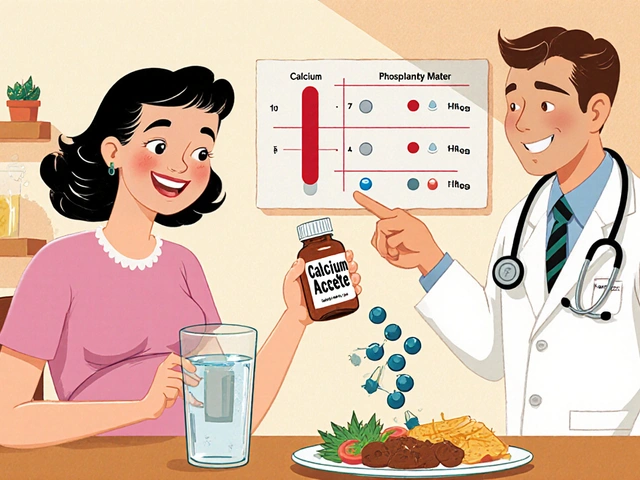
The gold standard is the serum folate test a simple blood draw that measures the amount of folate circulating in your bloodstream. Results below 3ng/mL generally indicate deficiency. Doctors may also order a homocysteine test - levels above 15µmol/L suggest folate‑related issues.
Because folate stores in red blood cells last longer, a red blood cell folate test can reveal chronic shortages, but it’s less common in routine care.

Boosting Folate: Food and Supplements
Whole foods beat pills for long‑term health. Below is a quick look at the top folate powerhouses.
| Food | Folate (µg) | Key Benefits |
|---|---|---|
| Spinach (cooked) | 194 | High iron, antioxidants |
| Lentils (cooked) | 181 | Plant protein, fiber |
| Black‑eye peas (cooked) | 162 | Low‑glycemic carbs |
| Asparagus (cooked) | 149 | Vitamin K, prebiotic fiber |
| Avocado | 81 | Healthy monounsaturated fats |
If you struggle to eat enough greens, a daily 400µg folic acid supplement (the amount recommended for most adults) can fill the gap. Pregnant women need 600-800µg, but anyone aiming to protect their heart should stay at least at the 400µg level.
Choose supplements labeled “certified USP” or “bio‑available methylfolate” for better absorption, especially if you have an MTHFR variant.
Common Pitfalls & When to Seek Professional Help
- Relying solely on multivitamins: Many contain only 200-400µg of folic acid, which may be insufficient if you have absorption issues.
- Over‑cooking vegetables: Heat destroys folate. Steam or eat raw when possible.
- Ignoring medication interactions: Anticonvulsants, sulfasalazine, and certain chemotherapy agents can deplete folate.
- Self‑diagnosing heart problems: If you experience chest pain, sudden weakness, or vision changes, call emergency services immediately - folate status is a long‑term factor, not an acute fix.
Schedule a blood test if you have any of the following:
- Family history of early heart disease or stroke
- Existing hypertension or high cholesterol
- Regular use of folate‑lowering medication
- Symptoms listed above persisting for more than a month
Your clinician can interpret both serum folate and homocysteine results, then tailor a diet‑plus‑supplement plan.
Frequently Asked Questions
Can folate deficiency cause a heart attack?
Low folate raises homocysteine, which damages the lining of arteries and promotes clot formation. While deficiency alone rarely triggers an immediate heart attack, it significantly ups the long‑term risk, especially when combined with high cholesterol or smoking.
How quickly can supplements lower homocysteine?
Clinical trials show a 20-30% reduction in homocysteine within 8-12 weeks of taking 400-800µg of folic acid daily, often alongside vitamins B6 and B12.
Are there risks to taking too much folic acid?
Excessive folic acid (over 1mg daily) can mask vitamin B12 deficiency symptoms and may be linked to a slight increase in certain cancers. Staying at the recommended 400µg for adults, unless advised otherwise by a doctor, is safest.
Is natural folate better than synthetic folic acid?
Natural folate (found in foods) is already in the reduced form that the body uses, so it bypasses the conversion step that some people struggle with. For those with MTHFR mutations, methylfolate supplements are often more effective.
Should I get my homocysteine level checked regularly?
If you have cardiovascular risk factors or a family history of early heart disease, testing every 1-2 years can help track progress after dietary changes or supplementation.





Comments
Skip your leafy greens, and you’ll gamble with heart disease.
I understand it can feel overwhelming, but adding a cup of cooked spinach to your meals can boost folate dramatically. Simple changes like swapping white rice for quinoa also help. Remember, consistency matters more than perfection.
When we look at the grand tapestry of human nutrition, folate emerges as a thread that binds the heart to the very pulse of life itself :) It is not merely a vitamin, but a silent guardian of our cellular symphonies, ensuring that DNA replication proceeds without a hitch. The deficiency, though subtle, can ripple through our arteries like a whispered warning, nudging the heart toward stress. Imagine a world where every plate is a canvas painted with leafy greens, lentils, and citrus – that is the promise of folate. Yet modern diets, awash in processed foods, often neglect this humble hero, leaving us vulnerable. Alcohol, for instance, plays a mischievous role, stripping away folate stores as if it were a thief in the night. Medications such as methotrexate add another layer of complexity, silently draining reserves. Genetics, too, whispers its own story, with certain polymorphisms making some people more prone to shortage. The calculator you’ve shared shines a light on these intertwined factors, offering a mirror to our habits. It reminds us that age and gender are not just numbers but clues in a larger puzzle. By recognizing the risk, we can act: supplement when needed, choose brighter plates, and perhaps even rethink lifestyle choices that silently erode our health. In the end, the heart beats strongest when nourished by a balanced diet, and folate is a key instrument in that rhythm 😊
Adding a daily serving of fortified cereal can cover most of the recommended folate intake without extra effort.
The calculator oversimplifies reality; risk scores don’t capture the nuanced interplay of genetics and diet.
Hey folks! 🌱 Remember, even a tiny bit of broccoli 🌳 can make a big diffrence – don’t underestimate the power of greens! 😊
In many Asian cuisines, fermented soy products naturally contain folate, showing how cultural dishes can support heart health.
Sure, because the government totally wants us to ignore folate and let big pharma profit from heart meds. 🙄
Great tool! Using it can motivate you to add more greens and keep that ticker happy.
Oh brilliant, another risk calculator – because we definitely needed more numbers to stress about.
One might argue that the very notion of "deficiency" is a cultural construct, a narrative woven by modern biochemistry to quantify the ineffable dance between organism and environment. Yet, when we peel back the layers, we encounter the stark reality that folate, a single-carbon donor, orchestrates the methylation symphony essential for genomic integrity. Its absence does not merely tip a scale; it rewrites the script of cellular destiny, setting the stage for homocysteine accumulation, endothelial dysfunction, and, inevitably, cardiovascular compromise. Consider the paradox of a society that champions convenience while silently sabotaging its own vascular architecture through processed indulgence. The calculators, though rudimentary, serve as mirrors reflecting this discrepancy, quantifying risk in discrete points-a reductionist attempt to capture complexity. However, each data point is a narrative fragment: age, gender, diet, alcohol, medications, familial predisposition-all converging to paint a portrait of vulnerability. In this mosaic, the humble leafy green becomes a hero, a silent sentinel guarding the heart's rhythm against the tide of oxidative stress. Conversely, heavy alcohol consumption acts as a rogue agent, depleting folate stores, amplifying homocysteine, and ushering in a cascade of endothelial injury. Medications, too, are double‑edged swords; antacids may impede folate absorption, while certain antimetabolites actively strip it away. The interplay of genetics adds another dimension-polymorphisms in MTHFR modulate the efficiency of folate metabolism, rendering some individuals intrinsically predisposed. Thus, the calculator's output is not merely a number; it is a call to introspection, urging us to recalibrate our dietary compass. Embrace fortified grains, relish the vibrancy of legumes, and honor the ancient wisdom embedded in traditional diets that prized folate-rich foods. In doing so, we transcend the calculator's numeric confines, weaving a lifestyle tapestry resilient against cardiac adversity. Ultimately, the heart thrives when nourished by a symphony of micronutrients, and folate stands as a keystone in this intricate architecture.