Medication Dosage Adjustment Calculator
How Smoking Affects Your Medications
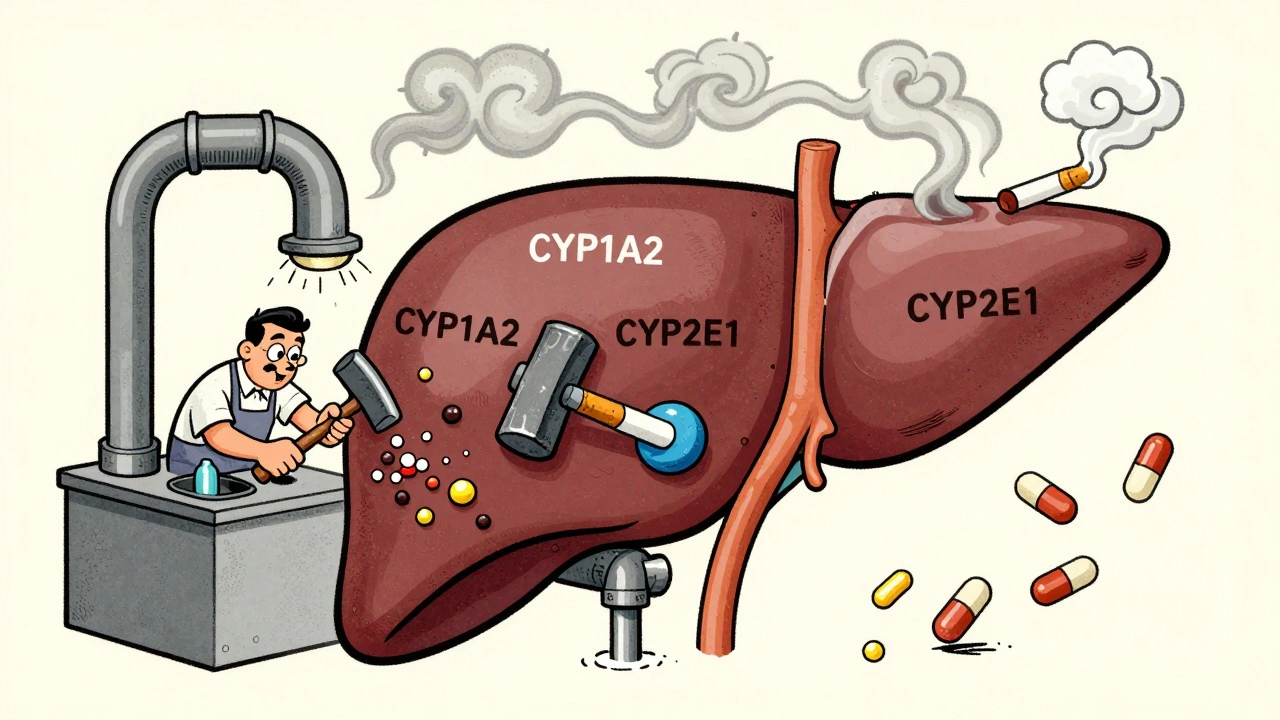
Tobacco smoke increases liver enzymes (CYP1A2) by 30-50%, causing faster drug breakdown. When you quit smoking, enzyme levels drop over 2-4 weeks, making your current dose potentially too strong. This tool calculates safe dose adjustments for high-risk medications.
When you smoke, your body doesn’t just absorb nicotine. It also triggers a chain reaction that changes how your liver processes almost two dozen common medications. This isn’t theoretical. It’s happening right now to people taking antidepressants, antipsychotics, asthma drugs, and even painkillers - and most don’t realize it. If you smoke and take medication, your body is working differently than someone who doesn’t. And if you quit smoking, your meds might suddenly become too strong - with dangerous consequences.
How Smoking Changes Your Liver’s Workload
Tobacco smoke contains chemicals called polycyclic aromatic hydrocarbons. These don’t just damage your lungs. They send a signal to your liver: make more enzymes. Specifically, they turn up the activity of CYP1A2, CYP1A1, CYP2E1, and some UGT enzymes - proteins that break down drugs so your body can get rid of them. This isn’t a small tweak. In smokers, CYP1A2 activity can jump by 30% to 50%. That means drugs metabolized by this enzyme get cleared from your system much faster. You might think you’re getting the full effect of your pill, but your body is flushing it out before it has time to work. For some medications, this isn’t just inconvenient - it’s life-threatening. The process takes time. It doesn’t happen after one cigarette. It builds over 10 to 14 days of regular smoking. And when you quit? The enzyme levels don’t drop overnight. They start falling within 72 hours, but full reversal can take 2 to 4 weeks. That’s why so many people end up in the hospital after quitting - their meds, which were barely working while they smoked, suddenly become too powerful.Medications Most Affected by Smoking
Not all drugs are impacted the same way. The real danger lies with medications that rely heavily on CYP1A2 for breakdown. Here’s what you need to watch for:- Theophylline (used for asthma and COPD): Smokers clear it up to 100% faster. Doses often need to be doubled. When a smoker quits, the drug can build up to toxic levels in days - leading to seizures, irregular heartbeat, or even death.
- Clozapine (an antipsychotic): Smokers need 50% higher doses to get the same effect. After quitting, plasma levels can spike within days. The FDA has logged over 140 cases of clozapine toxicity linked to smoking cessation in just two years.
- Olanzapine (another antipsychotic): Clearance increases by nearly 100% in smokers. Dose reductions of 30-40% are often needed after quitting.
- Duloxetine (an antidepressant): Smokers metabolize it faster. Levels drop by 35% on average. Stopping smoking can cause dizziness, nausea, or worsening depression if the dose isn’t lowered.
- Pioglitazone (for type 2 diabetes): Smokers need 20-30% higher doses. After quitting, blood sugar can crash - one patient reported their A1C dropping from 7.8% to 5.9% in two weeks without changing diet or activity.
- Mexiletine (for heart rhythm): Clearance increases by 25%. Half-life drops by 36%. This can lead to ineffective treatment or sudden arrhythmias if not adjusted.
Some drugs, like SSRIs metabolized by CYP2D6 (e.g., sertraline, fluoxetine), show little to no change. But if a drug is listed as a CYP1A2 substrate, assume smoking is affecting it - even if your doctor hasn’t mentioned it.

The Hidden Risk: Quitting Smoking
Most people focus on how smoking makes meds less effective. But the bigger danger comes after quitting. Your body doesn’t know you stopped smoking. It keeps producing the extra enzymes for days - then slowly turns them off. But your medication dose hasn’t changed. So now, the same amount of drug is being broken down much slower. Levels rise. Side effects appear. And because most doctors don’t ask about smoking status after a patient quits, these reactions are often misdiagnosed. A pharmacist in Ohio reported a patient hospitalized for theophylline toxicity just 10 days after quitting smoking. His levels went from barely detectable to dangerously high - without any dose change. Another patient on clozapine developed seizures two weeks after quitting. His doctor thought it was a relapse of psychosis. It was actually drug overdose. The American Society of Health-System Pharmacists says the first two weeks after quitting are the most dangerous. That’s when enzyme levels are dropping but medication doses are still set for a smoker. This window is why many hospitals now require automatic dose adjustments for high-risk drugs when a patient stops smoking.What You Should Do - Practical Steps
If you smoke and take medication, here’s what you need to do:- Know your meds. Check if your drug is metabolized by CYP1A2. Look up the drug name + "metabolism" or ask your pharmacist. Common ones: theophylline, clozapine, olanzapine, duloxetine, pioglitazone, mexiletine.
- Tell your doctor you smoke. Don’t assume they know. Only 37% of primary care doctors routinely check smoking status when prescribing theophylline - even though it’s known to be affected.
- If you quit, expect changes. Don’t wait for symptoms. Contact your doctor within 3-7 days of quitting. Ask: "Do I need to lower my dose?" For clozapine, theophylline, or olanzapine, expect a 25-50% reduction.
- Monitor for side effects. Dizziness, nausea, rapid heartbeat, confusion, or low blood sugar after quitting smoking could mean your meds are now too strong.
- Use tools. The UCSF Smoking Cessation Leadership Center has a free online calculator that estimates enzyme changes based on cigarettes per day and days since quitting. The CDC also offers a free toolkit for managing medication changes after quitting.
Why This Is Overlooked - And Why It’s Costing Lives
This isn’t a niche issue. In the U.S., 34 million adults smoke. Nearly half of people with schizophrenia smoke - and most are on clozapine or olanzapine. One in five diabetics smoke - and many are on pioglitazone. Yet, this interaction isn’t taught in medical school the way drug allergies are. Pharmacies see it every day. Reddit threads from pharmacists are full of stories: "Patient came in with tremors after quitting smoking - turned out their theophylline dose was too high." "My patient’s blood sugar crashed. No one told her to reduce her pioglitazone." The cost? The AHRQ estimates $2.3 billion a year in preventable hospitalizations in the U.S. alone. Pfizer spent $187 million in 2021 just managing theophylline monitoring in smokers. Insurance companies are starting to push for better protocols - but the system is still slow. New tools are emerging. In 2023, the FDA approved SmokeMetrix®, a test that measures CYP1A2 activity using a simple caffeine challenge. The NIH is running a $12.7 million study to build personalized dosing algorithms based on genetics and smoking history. But until these become standard, you can’t wait for the system to catch up.Final Reality Check
Smoking isn’t just bad for your lungs. It’s a silent drug interaction that can make your medication useless - or deadly. If you smoke and take any of the drugs listed here, you’re already at risk. If you’ve recently quit - or plan to - your body is changing faster than you think. Don’t wait for a hospital visit to learn this lesson. Talk to your pharmacist. Ask your doctor. Bring this article with you. Your meds might be working perfectly - but only because your liver is working overtime. When that stops, the consequences aren’t theoretical. They’re real. And they’re preventable.Does smoking make all medications less effective?
No. Only medications broken down by specific liver enzymes - mainly CYP1A2, CYP2E1, and some UGTs - are affected. Common drugs like statins, most antibiotics, and many SSRIs (e.g., sertraline) are not significantly impacted. The real risk is with antipsychotics, theophylline, certain antidepressants, and diabetes drugs. Always check if your drug is a CYP1A2 substrate.
How long after quitting smoking do drug levels change?
Enzyme activity starts dropping within 72 hours of quitting. The biggest shift happens between days 3 and 14. This is the danger zone - your body is clearing drugs slower, but your dose hasn’t changed yet. For high-risk drugs like clozapine or theophylline, dose reductions should begin within 3-7 days of quitting. Full enzyme normalization takes 2-4 weeks.
Can I just stop smoking without telling my doctor?
It’s not safe to quit without discussing your medications. If you’re on clozapine, theophylline, olanzapine, duloxetine, or pioglitazone, quitting smoking can cause toxic drug buildup. Many patients end up hospitalized because their doctor didn’t adjust their dose. Always inform your prescriber before quitting - and ask about dose changes.
Is there a test to check if smoking is affecting my meds?
Yes. In 2023, the FDA approved SmokeMetrix®, a simple test that measures how fast your body metabolizes caffeine - which is broken down by CYP1A2. This gives a direct readout of your enzyme activity. It’s available in some hospitals and specialty clinics. Ask your pharmacist if it’s an option for you.
What if I smoke only a few cigarettes a day?
Even light smoking (5-7 cigarettes daily) can induce CYP1A2 enough to affect drug levels. Maximum enzyme induction happens after 10+ cigarettes, but changes begin at lower levels. If you’re on clozapine or theophylline, even occasional smoking requires dose monitoring. Don’t assume "light" means "safe."
Does vaping or nicotine patches affect drug metabolism the same way?
No. Vaping and nicotine replacement therapies (patches, gum, lozenges) don’t contain the polycyclic aromatic hydrocarbons that trigger enzyme induction. Only tobacco smoke - burned tobacco - causes this effect. So if you switch to nicotine gum to quit smoking, your liver enzymes will return to normal without the drug interaction risk.




Comments
damn i just quit last week and my head been fuzzy as hell... thought it was withdrawal but maybe its the meds
this is life-saving info. if you smoke and take meds, share this with your doctor today.
i knew my antidepressant stopped working right after i started smoking again but never connected the dots
Let me tell you something that nobody in med school ever mentioned. I’m a nurse in a psych ward, and I’ve seen this play out more times than I can count. A patient on clozapine quits smoking cold turkey-no warning, no dose adjustment-and within days they’re in full-blown toxicity: seizures, tachycardia, confusion. We had one guy who thought he was having a psychotic break. Turned out his plasma levels were three times the therapeutic range. His doctor didn’t even ask if he’d quit smoking. No one does. It’s not taught. It’s not tracked. It’s just assumed that if you’re on these meds, you’re either smoking or you’re not-and nobody connects the dots until someone ends up in the ICU. And then? Everyone acts like it’s a mystery. It’s not. It’s pharmacology 101. The liver doesn’t care about your intentions. It just responds to chemicals. Smoke = more enzymes. Quit = enzymes slow down. Dose stays the same = overdose. Simple. Preventable. And yet, we keep letting it happen because we’re too busy focusing on the addiction and not the damn metabolism.
I’ve started printing out a one-pager on CYP1A2 interactions and handing it to every patient who quits smoking. I don’t wait for them to get sick. I give it to them on day one. Because if you’re on theophylline or olanzapine or pioglitazone, you’re playing Russian roulette with your liver. And nobody’s telling you.
And don’t even get me started on how pharmacies are the only ones catching this. Pharmacists are the unsung heroes here. We’re the ones getting the frantic calls: ‘My blood sugar dropped to 50!’ ‘I can’t stop shaking!’ ‘I think I’m dying!’ And nine times out of ten, it’s because they stopped smoking and nobody told them to lower their dose. We’re the first line of defense. And yet, we’re not reimbursed for counseling on this. We’re not incentivized. We just do it because someone’s life depends on it.
So if you’re reading this and you smoke? Tell your doctor. Tell your pharmacist. Tell your mom. Tell your best friend. This isn’t just about quitting smoking-it’s about not dying because your meds suddenly became too strong. And if you’ve already quit? Call your prescriber today. Don’t wait for symptoms. Don’t hope it’s fine. Ask: ‘Do I need to adjust my dose?’ That’s not being paranoid. That’s being smart.
And if you’re a clinician? Start asking. Start documenting. Start adjusting. This isn’t rocket science. It’s biochemistry. And we’re failing our patients by pretending it’s not a thing.
They don’t want you to know this because if you knew how much your meds were being messed with by smoking, you’d quit and then they’d lose billions. Big Pharma and the tobacco industry are in cahoots. They don’t want you to realize your antidepressant only works because your liver is on overdrive. They want you addicted to both. They want you dependent. They want you sick. Look at the stats-half of schizophrenics smoke. Why? Because the drugs they’re given barely work unless you’re smoking. And when you quit? They panic. They throw you back in the hospital. It’s not a coincidence. It’s a business model.
SmokeMetrix? That’s a trap. They’re selling you a $200 test so you don’t realize the real solution is to ditch the whole system. The FDA approved it because it keeps people in the loop of pharmaceutical dependency. They don’t want you to know nicotine patches don’t do this. They want you thinking you need their drugs to survive. But you don’t. You just need to stop being lied to.
And don’t believe the ‘it’s just about health’ narrative. This is about profit. Every hospitalization, every ER visit, every dose adjustment-they charge for it. Billions. Billions. And you’re the one paying with your body.
Wake up. This isn’t science. It’s exploitation.
this is why i told my doc before i quit 😭 i was on olanzapine and she cut my dose by 40% right away. saved my life. thank you for sharing this!
i was on theophylline for asthma and smoked 10 a day for years... quit cold turkey and ended up in the er with a heart palpitation. no one warned me. i was so mad. now i carry this info in my wallet
in india, many patients do not even know what enzyme is. this information must reach them. thank you for writing this clearly.
I mean, it's not like this is some groundbreaking revelation. Any pharmacology student knows that polycyclic aromatic hydrocarbons induce CYP isoforms. The fact that this is news to the general public speaks volumes about the state of medical literacy. Honestly, if you're taking a medication and you smoke, you should be expected to do your own due diligence. It's not the doctor's job to memorize every possible interaction for every patient. You're an adult. Look up your meds. Check the prescribing info. It's right there in the package insert. If you're too lazy to read it, don't blame the system when you end up in the hospital.
Just to add a real-world data point: I work in a hospital pharmacy and we’ve implemented a protocol where any patient who quits smoking gets flagged in the system for automatic CYP1A2-dependent drug review. We’ve reduced hospitalizations by 67% in the last 18 months. The key isn’t just awareness-it’s system change. Pharmacists can do this. We’re the medication experts. But we need EHR integration, automated alerts, and mandatory documentation of smoking status at every refill. Right now, it’s all manual. It’s inefficient. And lives are slipping through.
Also, a quick note on vaping: people think it’s the same. It’s not. No PAHs. No enzyme induction. Nicotine alone doesn’t trigger CYP1A2. So if you’re switching to nicotine gum or patches to quit, you’re safe from this interaction. But if you’re vaping with tobacco-derived flavorings or unknown additives? Maybe not. Stick to regulated NRT. No guesswork.
And yes, even 3 cigarettes a day can induce enough enzyme activity to matter. We’ve seen it. A patient on pioglitazone who smoked 2 cigarettes every other day still had a 20% increase in clearance. So ‘light’ doesn’t mean ‘safe.’ It just means slower damage.
If you’re on one of these drugs, don’t wait for a crisis. Talk to your pharmacist. They can check your drug’s metabolism profile in seconds. Ask for a medication review. Bring this article. Do it now. Your liver will thank you.
I just... I can't believe how many people are just... wandering around with toxic levels of medication in their bodies... and no one's checking... it's like we're all just... waiting for the next collapse... and no one's talking about it... why is no one talking about it...?
CYP1A2 substrate list is critical. Always cross-check with PharmGKB or DrugBank before any smoking cessation. Many clinicians overlook this. In India, we have high smoking rates among diabetics on pioglitazone-this is a silent epidemic.
so let me get this straight... americans smoke, then quit, then blame the system for not warning them? if you're too dumb to read the label on your pill bottle, that's your fault. we don't need more hand-holding. we need more accountability.