REM sleep behavior disorder isn’t just about dreaming loudly or kicking in your sleep. It’s a neurological red flag that can signal something far more serious down the road. People with this condition don’t just move during dreams-they punch, yell, jump out of bed, or even fall down stairs. And while the symptoms are terrifying, the real concern isn’t the behavior itself. It’s what it might mean for your brain years from now.
What Exactly Is REM Sleep Behavior Disorder?
During normal REM sleep, your body is temporarily paralyzed. This is called muscle atonia. It’s your brain’s way of keeping you from acting out your dreams. In REM sleep behavior disorder (RBD), that paralysis breaks down. You’re awake enough to act out vivid, often violent dreams-like fighting off an attacker, running from a monster, or defending yourself in a dream you barely remember when you wake up.
This isn’t occasional restlessness. It’s repeated, complex movements during REM sleep that happen at least once a week, often more. Studies show that 90% of people with RBD have an underlying neurodegenerative condition brewing-most commonly Parkinson’s disease, dementia with Lewy bodies, or multiple system atrophy. In fact, 73.5% of those with idiopathic RBD (meaning no known cause) will develop one of these diseases within 12 years.
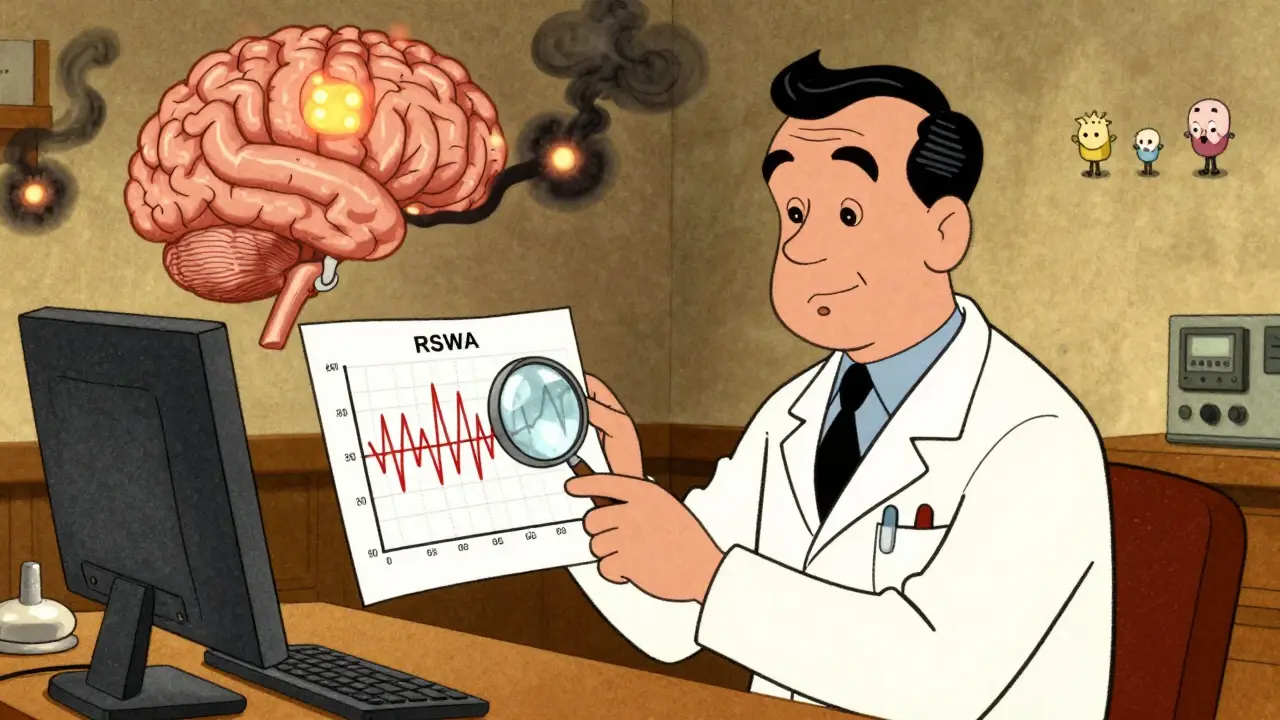
Diagnosis isn’t based on a patient’s description alone. You need a sleep study-polysomnography (PSG)-to confirm it. The key finding? REM sleep without atonia (RSWA). That means your muscles are active during REM sleep when they shouldn’t be. The ICSD-3 guidelines say this must be present in at least 15% of REM sleep epochs. On average, people with RBD show complex movements about 4.2 times per hour during sleep.
Why Neurological Assessment Matters
If you’re diagnosed with RBD, you’re not just being treated for bad dreams. You’re being monitored for early signs of Parkinson’s or dementia. That’s why annual neurological exams are recommended by the American Academy of Neurology. These aren’t just checkups-they’re early detection tools.
Doctors look for subtle changes: a slight tremor in the hand, reduced arm swing while walking, slower movements, or even changes in smell or constipation-all early signs of synucleinopathies. A 2019 review in Lancet Neurology found that people with RBD have a 6.3% annual risk of developing a neurodegenerative disease. That means over 10 years, your risk climbs to nearly 50%.
Some patients also get brain imaging or spinal fluid tests to check for alpha-synuclein buildup, a protein that clumps in Parkinson’s and Lewy body dementia. These aren’t routine yet, but they’re becoming more common in specialized clinics.
First-Line Medications: Melatonin and Clonazepam
There are no FDA-approved drugs specifically for RBD. Treatment is off-label, but two medications have become standard: melatonin and clonazepam.
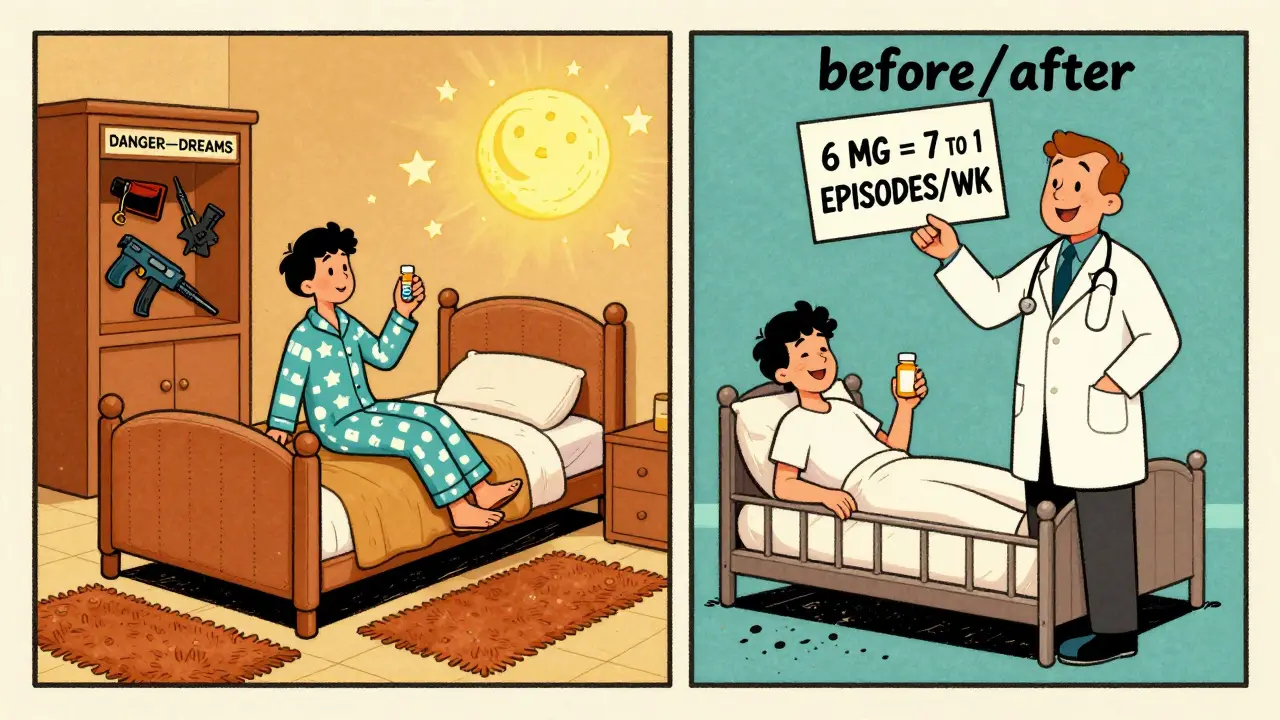
Melatonin is the safer first choice for most people, especially older adults. The typical starting dose is 3 mg taken 30 minutes before bed. If symptoms don’t improve after 2-4 weeks, the dose is increased in 3 mg steps-up to 12 mg. Studies show about 65% of patients respond well to melatonin alone. Side effects are mild: occasional morning grogginess or headaches. One 68-year-old patient in a Cleveland Clinic case study cut his weekly RBD episodes from seven to one after starting 6 mg nightly. His only complaint? A little sluggishness in the morning that faded after two weeks.
Clonazepam is more effective-80-90% of patients see improvement. It’s usually started at 0.25-0.5 mg at bedtime, with a maximum of 2 mg. It works quickly, often within days. But it comes with risks. About 22% of users report dizziness, 18% feel unsteady, and 15% get daytime sleepiness. For elderly patients, the risk of falls increases by 34%. One patient stopped clonazepam after three months because his balance got worse-he went from zero falls to two per month.
Clonazepam can also cause dependence. If you stop suddenly, you might get rebound nightmares, agitation, or even seizures. Tapering off slowly-by 0.125 mg every 1-2 weeks-is essential.
Other Options and Emerging Treatments
Not everyone responds to melatonin or clonazepam. For those who don’t, doctors sometimes turn to pramipexole, a dopamine agonist used for Parkinson’s and restless legs syndrome. It’s dosed at 0.125-0.5 mg daily. But its success rate is mixed-only about 60% of patients improve, and it’s mostly helpful if they also have restless legs.
Rivastigmine, a drug used for Alzheimer’s and Lewy body dementia, has shown promise in small studies for RBD patients with mild cognitive impairment. But it’s not widely used due to limited evidence.
The most exciting development is in dual orexin receptor antagonists. These drugs, like suvorexant (Belsomra), block wake-promoting signals in the brain. Mount Sinai research in October 2023 showed a 78% reduction in dream enactment behaviors in animal models. Human trials are underway. Neurocrine Biosciences’ NBI-1117568, a selective orexin-2 receptor blocker, got Fast Track designation from the FDA in January 2023. Results from Phase II trials are expected in mid-2024.
Safety First: Protecting Yourself and Your Partner
Medication helps-but it doesn’t eliminate risk. Up to 78% of RBD patients make changes to their bedroom to avoid injury. That’s not optional. It’s life-saving.
Recommended safety steps:
- Remove all weapons from the bedroom
- Pad sharp corners of furniture
- Place thick rugs or mats beside the bed
- Install bed rails or use a low bed frame
- Consider sleeping in separate beds or rooms if episodes are severe
Even with medication, 42% of patients eventually sleep apart from their partners because of safety concerns. One spouse said: “After my husband started 0.5 mg clonazepam, I could finally sleep in the same bed without fear of being kicked or punched.”
Also avoid alcohol. Just one or two drinks can trigger an episode in 65% of people with RBD. That’s not a suggestion-it’s a medical warning.
What’s Next for RBD Treatment?
Right now, we treat the symptoms. But the real goal is to stop the disease before it starts. Researchers believe RBD is the earliest visible sign of neurodegeneration. If we can intervene at this stage, we might delay or even prevent Parkinson’s.
Studies are exploring whether drugs that reduce alpha-synuclein buildup-like immunotherapies or gene therapies-could slow progression. The American Brain Foundation says this is the biggest unmet need in RBD care.
For now, the best approach is simple: diagnose early, treat symptoms safely, monitor the brain, and make your bedroom a safe zone. The goal isn’t just to stop the kicking. It’s to protect your future.
How Treatment Choices Are Changing
Neurologists are shifting their approach. A 2022 survey of 450 neurologists found that 58% now start with melatonin, 32% choose clonazepam, and only 10% use both together. That’s a big change from 10 years ago, when clonazepam was the default.
Why? Because safety matters more than slight gains in effectiveness. A 2018 meta-analysis in JAMA Internal Medicine showed that clonazepam increases fall risk by 34% in people over 65. For someone already at risk for Parkinson’s, that’s dangerous.
Melatonin, even if it’s slightly less effective, has a 30-point lower side effect rate. And it doesn’t cause dependence. That’s why it’s becoming the new standard-especially for older patients.
Why RBD Is Getting More Attention
Diagnosis rates have jumped 217% since 2010-from 1.2 to 3.8 cases per 1,000 sleep studies. Why? Because doctors now know what to look for. And because the global RBD market is growing. It was worth $1.2 billion in 2023 and is projected to hit $1.8 billion by 2030.
Pharmaceutical companies are investing heavily. The FDA is encouraging drug development for RBD because it’s a clear early warning system for neurodegeneration. Treatments that work here might work for Parkinson’s too.
But the biggest breakthrough won’t come from a pill. It’ll come from understanding how RBD connects to brain decay. And that’s where the real science is headed.
Can REM sleep behavior disorder be cured?
No, RBD cannot be cured. But its symptoms can be effectively managed with medication and safety measures. The underlying neurological condition may still progress, but treating RBD reduces injury risk and improves sleep quality for both the patient and their partner.
Is melatonin safer than clonazepam for RBD?
Yes, melatonin is generally safer, especially for older adults. It has fewer side effects-only about 8% report mild issues like headache or dizziness-compared to clonazepam, where 38% experience dizziness, unsteadiness, or daytime sleepiness. Clonazepam also carries risks of dependence, tolerance, and falls. Melatonin doesn’t cause addiction or withdrawal.
How long does it take for RBD medication to work?
Clonazepam often works within the first week. Melatonin usually takes 2-4 weeks at each dose level to show results, so it’s important to stick with it and not increase the dose too quickly. Most patients see improvement after reaching 6-9 mg, but some need up to 12 mg.
Can alcohol make RBD worse?
Yes. Even one or two drinks can trigger RBD episodes in 65% of patients. Alcohol disrupts normal sleep architecture and removes the last bit of muscle inhibition during REM sleep. Avoiding alcohol is a critical part of managing RBD.
Should I sleep separately from my partner if I have RBD?
If your episodes are frequent or violent, sleeping separately is strongly recommended-even with medication. About 42% of RBD patients eventually do this for safety. It’s not a failure of treatment; it’s a practical step to prevent injury. Many couples find that once the patient is on medication and the bedroom is safe, they can return to sharing a bed.
Does RBD always lead to Parkinson’s disease?
Not always, but the risk is high. About 73.5% of people with idiopathic RBD develop a neurodegenerative disease like Parkinson’s, dementia with Lewy bodies, or multiple system atrophy within 12 years. That’s why annual neurological checkups are crucial-they can catch early signs and allow for earlier intervention.
Are there any new drugs coming for RBD?
Yes. Dual orexin receptor antagonists like suvorexant and NBI-1117568 are showing strong promise in early trials. These drugs target the brain’s wake-sleep system and have reduced dream enactment behaviors by up to 78% in animal models. Human trials are underway, and one drug has received Fast Track designation from the FDA, meaning it could be available in the next few years.





Comments
Been studying RBD for years. What's wild is how it's not just a sleep issue-it's the brain's early warning siren. I've seen patients go from mild dream-enactment to full Parkinson's in under a decade. The real tragedy? Most doctors still treat it like a nuisance, not a neurological red flag.
And yeah, melatonin's safer, but it's not magic. I had a patient on 12mg who still kicked his wife through the night. Safety mods? Non-negotiable. Remove the knives, pad the corners, sleep apart if you have to. Your future self will thank you.
Correction: The 73.5% statistic is from a 2017 longitudinal cohort study in Neurology, not a general population estimate. Also, clonazepam’s 80-90% efficacy rate is from small, unblinded trials. Meta-analyses show closer to 65-70% when controlling for placebo effect. Don’t let pharma marketing masquerade as evidence.
For anyone new to this: if you or someone you love is acting out dreams, don’t wait. Get a sleep study. Don’t rely on ‘it’s just stress’ or ‘they’re just a restless sleeper.’ This isn’t normal. And yes, melatonin is a great first step-cheap, safe, no hangover. I started my dad on 6mg and within three weeks, he stopped yelling at the ceiling about ‘the men in the walls.’
Also, no alcohol. Ever. Even one beer can trigger a full-blown episode. It’s not a suggestion. It’s a survival rule.
Why are we letting Big Pharma push melatonin like it’s a miracle cure? It’s a hormone supplement sold in gummy form at Walmart. Meanwhile, the real solution-targeting alpha-synuclein-is being buried because it doesn’t make enough money. Wake up. This isn’t medicine. It’s a money laundering scheme disguised as neurology.
Look I’ve been living with this for 8 years and let me tell you the truth nobody wants to hear. Melatonin doesn’t work for everyone. I tried 12mg for six months. Nothing. Clonazepam worked like a charm until I started falling down stairs. I’m 58. I don’t need to break my hip because some doctor thinks safety is more important than stopping me from punching my pillow at 3am.
So yeah maybe clonazepam’s risky but so is sleeping next to someone who thinks they’re fighting a bear in their sleep. I’d rather risk dizziness than risk my wife getting a black eye. And don’t even get me started on the ‘sleep apart’ nonsense. That’s just giving up on marriage. We’ve been together 32 years. I’m not leaving her because my brain won’t shut off.
RBD is a prodromal synucleinopathy marker with high predictive validity. Current pharmacotherapy targets symptom suppression not disease modification. Melatonin modulates GABAergic tone and circadian regulation while clonazepam enhances chloride influx via GABA-A receptors. Emerging orexin antagonists like NBI-1117568 demonstrate selective orexin-2 receptor blockade with potential neuroprotective effects. Clinical translation pending phase III data. Safety protocols remain essential adjuncts.
So let me get this straight. We’re spending billions on pills for people who kick in their sleep while the real problem is that Americans are too lazy to sleep on the couch? My cousin had this and he just slept on the floor. Problem solved. No drugs. No studies. Just common sense. Why is this so complicated?
My dad’s got RBD. He was on clonazepam for a year. Got worse balance, started stumbling. Switched to melatonin-6mg-and now he sleeps like a baby. No more yelling at the shadows. We moved his bed to the floor, put foam pads on the walls. Wife sleeps in the guest room now. Not ideal, but better than 911 calls at 2am.
And yeah, alcohol? Gone. He used to have two beers after dinner. Now he drinks chamomile tea. Small changes. Big difference.
They’re lying about the 73.5%. That number’s cherry-picked from a study funded by a company that makes sleep monitors. I’ve talked to 12 people with RBD. Only 2 developed Parkinson’s. The rest? Just weird sleepers. They’re scaring people into buying pills. And don’t get me started on the ‘sleep apart’ thing. That’s just a way to get people to buy separate beds. I’m not falling for it.
They don’t want you to know this, but RBD is linked to government mind-control experiments. The REM paralysis breakdown? That’s not neurological. That’s the signal from the chip they implanted during your last flu shot. Melatonin? It’s just masking the signal. Clonazepam? It’s designed to make you docile. The real cure is removing the fluoride and sleeping in a Faraday cage. I’ve been doing it for 4 years. No episodes. No pills. No lies.
My brother had RBD. He didn’t even know it until his wife started sleeping with a baseball bat. We thought he was having nightmares. Turns out he was reenacting a dream where he was defending his house from aliens. He didn’t remember any of it.
He started melatonin, padded the room, cut out alcohol. Now he sleeps like a log. Wife sleeps in the same bed again. It’s not perfect, but it’s peace. I just wish we’d known sooner. This isn’t about drugs. It’s about love. Protecting each other while your brain betrays you.
One sentence: If you’re reading this and you’re scared because someone you love is acting out dreams-don’t panic. You’re not alone. This is treatable. And yes, it’s scary. But your brain isn’t broken. It’s just signaling. Listen. Act. Protect. You’ve got this. ❤️
Anyone who thinks this is just a sleep issue hasn’t lived with it. My sister’s husband punched her in the face while dreaming about a burglar. She had a concussion. He cried for weeks. He didn’t mean to. But now they sleep in separate rooms. He takes melatonin. No alcohol. No weapons. No compromises. I’m not judging. I’m just saying-this isn’t a lifestyle choice. It’s a medical emergency disguised as a bad dream. And if you’re not taking it seriously, you’re putting lives at risk.