Every year, over 5.8 billion prescription drug packages move through the U.S. supply chain-from factories to warehouses, to pharmacies, and finally to patients. Behind this massive flow is a quiet but powerful system designed to stop fake, tainted, or stolen drugs from ever reaching your medicine cabinet. This isn’t science fiction. It’s the Drug Supply Chain Security Act (DSCSA), a 10-year regulatory overhaul that’s reshaped how drugs are tracked, verified, and protected from counterfeiters.
What Exactly Is the DSCSA?
Passed in 2013, the DSCSA didn’t just add a few new rules. It built a digital backbone for the entire U.S. pharmaceutical supply chain. Before this law, tracking a single pill from manufacturer to patient was nearly impossible. Paper records, inconsistent labeling, and disconnected systems made it easy for counterfeiters to slip fake drugs into the mix. The DSCSA changed that by requiring every prescription drug package to have a unique digital fingerprint. That fingerprint is a 2D barcode, called a Data Matrix, containing four key pieces of information: the National Drug Code (NDC), a unique serial number, the lot number, and the expiration date. Every time a package changes hands-whether it’s shipped from a factory, stored in a warehouse, or dispensed at a pharmacy-its data is scanned and recorded electronically. By November 2023, all trading partners were required to exchange this data electronically using a standard called EPCIS, making the whole system interoperable.How It Stops Counterfeit Drugs in Real Time
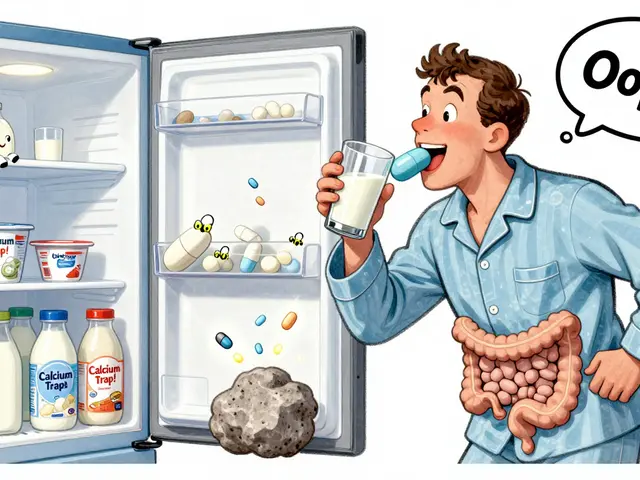
Counterfeit drugs don’t always look fake. Some are convincing replicas of real packaging. Others are repackaged expired pills or stolen products diverted from legitimate channels. The DSCSA tackles these threats in three ways: serialization, verification, and authorized trading partner checks. Serialization means every package has a unique ID. No two are the same. That’s critical because it lets pharmacies and distributors check if a package is real. When a pharmacist scans a bottle at the counter, the system instantly compares the serial number against the manufacturer’s database. If it doesn’t match-or if the package was already sold and decommissioned-the system flags it as suspect. Verification isn’t just a one-time check. It’s an ongoing process. If a distributor receives a shipment with odd serial numbers or mismatched data, they’re required to investigate within 24 hours. In 2022, this process helped stop around 12,000 suspect product incidents before they reached patients. That’s not a number you hear often-but it’s real. Then there’s the Authorized Trading Partner (ATP) system. Only companies registered with the FDA can legally handle prescription drugs. The ATP system checks every supplier’s credentials before any transaction is allowed. In 2023, over 50,000 ATP verifications happened daily, with a 99.8% success rate. If someone tries to sell drugs without being registered, the system blocks them.Real-World Impact: When the System Worked
The DSCSA isn’t just theoretical. It’s saved lives. During the 2022 infant formula crisis, when contaminated batches were identified, the system traced affected products to specific lots and locations within 72 hours. Before DSCSA, that process took an average of two weeks. Faster recalls mean fewer people are exposed to dangerous products. In 2021, during the peak of the COVID-19 vaccine rollout, the same system tracked over 98.7% of vaccine shipments in real time. That level of visibility kept counterfeit or mishandled vaccines out of circulation. Dr. Margaret Hamburg, former FDA commissioner, called this infrastructure “invaluable” for public health. Even smaller players benefit. Independent pharmacy owner David Chen says his store’s DSCSA-compliant scanner caught a suspicious shipment from an unregistered supplier last year. “It wasn’t a big deal-just one box-but if we hadn’t scanned it, that fake drug could’ve gone to an elderly patient,” he said.
Where the System Still Has Gaps
Despite its successes, the DSCSA isn’t perfect. One major weakness is repackaged drugs. When a hospital or pharmacy repackages pills into blister packs or unit-dose containers, the original barcode is often destroyed. That breaks the chain of traceability. The FDA acknowledges this gap, and some companies are testing new labels that stick to repackaged containers, but it’s still a vulnerability. Another issue is cost. For small pharmacies, DSCSA compliance can cost up to $18,500 a year in software, scanners, and staff training. That’s 3.2% of net profit for some. Many independent pharmacies struggled to meet the 2023 deadline, and the National Community Pharmacists Association estimates $1.2 billion is still needed by 2027 for smaller players to fully comply. Even the technology isn’t flawless. About 12.7% of barcodes fail to scan due to poor printing or damage. And false positives happen-8.3% of flagged products turn out to be legitimate after investigation. That creates extra work for pharmacists who are already stretched thin.How the U.S. Compares to the Rest of the World
The U.S. isn’t alone in fighting counterfeit drugs. The European Union uses the Falsified Medicines Directive (FMD), which also requires unique identifiers and tamper-proof packaging. But there’s a big difference: the EU uses a centralized database that all pharmacies connect to, while the U.S. uses a decentralized system where each company exchanges data directly. That makes the U.S. system more flexible but harder to coordinate. The EU’s model is simpler for pharmacies but more rigid for manufacturers. Meanwhile, countries like China forced serialization overnight in 2019, which caused massive supply chain disruptions. The U.S. took a slower, phased approach-giving companies time to adapt. That’s why compliance rates in the U.S. are now over 90% for manufacturers and 87% for wholesalers. But international trade remains a weak spot. A drug made in India and shipped to the U.S. must meet both DSCSA and local regulations. There’s no global standard yet, so companies spend 22% more to comply across borders, according to PwC.What’s Next? The Road to 2027
The final deadline is November 2027. By then, every single transaction in the U.S. drug supply chain must be electronic. No more paper invoices, no more manual logs. Everything will be digital, secure, and instantly verifiable. New tech is already emerging. Some companies are testing blockchain to make data tamper-proof. Others use AI to spot unusual patterns-like a sudden spike in serial numbers from one supplier-that could signal fraud. IoT sensors are being added to cold-chain shipments to track temperature and humidity, ensuring drugs like insulin don’t spoil. The goal isn’t just to catch fakes-it’s to predict them. McKinsey predicts that by 2030, the system will evolve into a predictive analytics platform, reducing counterfeit incidents by 95% and saving $8.7 billion annually in efficiency gains.What Patients Need to Know
You don’t need to scan barcodes or check serial numbers. That’s the job of pharmacies and distributors. But you can stay safe by:- Only buying prescription drugs from licensed pharmacies-online or in person.
- Being wary of deals that seem too good to be true, especially for expensive medications.
- Checking if an online pharmacy is verified by the National Association of Boards of Pharmacy (NABP).
- Reporting suspicious packaging or pills to your pharmacist or the FDA.
Final Thoughts
Counterfeit drugs are a global problem. But the U.S. has built one of the most advanced defenses in the world. It’s not perfect, and it’s expensive-but it’s working. Since 2015, counterfeit drug seizures have dropped by 63%. That’s not just a statistic. It’s thousands of people who didn’t get poisoned, didn’t get sicker, didn’t die because a fake pill slipped through. The system is still evolving. It’s getting smarter, faster, and more connected. And for patients, that means one thing: your medicine is safer today than it was a decade ago.How does the DSCSA stop counterfeit drugs from reaching patients?
The DSCSA requires every prescription drug package to have a unique 2D barcode with a serial number, lot number, expiration date, and NDC. Every time the package changes hands, this data is scanned and recorded electronically. Pharmacies and distributors can verify the serial number against the manufacturer’s database in seconds. If the number is fake, duplicated, or already used, the system flags it as suspect and blocks distribution. This prevents counterfeit, stolen, or expired drugs from entering the supply chain.
Are all drugs in the U.S. covered by the DSCSA?
No. The DSCSA applies only to prescription drugs distributed in the U.S. It does not cover over-the-counter (OTC) medications, veterinary drugs, blood products, or medical gases. However, most prescription medications-including antibiotics, insulin, heart medications, and cancer treatments-are fully tracked under the system.
Can I check if my medicine is real myself?
Not directly. The verification system is designed for pharmacies and distributors, not consumers. But you can look for signs of tampering-broken seals, unusual packaging, or pills that look different than usual. If something seems off, ask your pharmacist to verify the batch. They’re trained to use the DSCSA system and can check the serial number for you.
Why do some pharmacies still have problems with DSCSA compliance?
Small, independent pharmacies often struggle with the cost and complexity. Installing barcode scanners, upgrading software, training staff, and integrating with new data systems can cost up to $18,500 a year. Many also use outdated IT systems that don’t easily connect to modern EPCIS platforms. While larger chains had resources to adapt, smaller pharmacies needed more time-and financial support-to meet the 2023 deadline.
What happens if a counterfeit drug gets past the system?
The DSCSA includes rapid recall protocols. If a counterfeit drug is discovered after distribution-whether through patient reports, lab testing, or a supplier alert-the manufacturer must notify all trading partners within 24 hours. The system then traces every package with that serial number and removes it from shelves. In 2022, this process helped remove over 12,000 suspect products before they reached patients. While no system is 100% foolproof, the speed and precision of this response have dramatically reduced harm.





Comments
so this dscsa thing is kinda wild tbh. like, imagine every pill has its own tiny digital passport. i never thought about how hard it must be to track billions of these. still, sometimes i wonder if the real problem is just... too many people trying to profit off sick folks. not sure the barcode fixes that.
also, typo: 'dscsa' not 'dscsa'... again. sorry.
The implementation of the Drug Supply Chain Security Act represents a monumental stride in public health governance. By mandating serialization and electronic data interchange, the United States has aligned itself with global best practices in pharmaceutical integrity. This systemic rigor not only deters illicit actors but also reinforces institutional trust - a commodity increasingly rare in modern healthcare. One must acknowledge the diligence of regulators and industry stakeholders who executed this transition with remarkable precision.
It is fascinating to contemplate the philosophical underpinnings of this system: the notion that identity, even at the molecular level of a pharmaceutical compound, can and should be uniquely traceable. In doing so, we are not merely securing supply chains - we are asserting a moral imperative that human life, in its most vulnerable state, deserves an unbroken chain of accountability. Yet, the cost burden on small pharmacies raises an ethical paradox: who bears the price of safety? Is it just that those on the frontlines pay while the systemic beneficiaries remain insulated?
EPCIS interoperability remains a fragmented mess despite the mandate. The lack of standardized schema enforcement across ERP platforms creates latent data drift - especially in legacy HL7 integrations. False positives at 8.3% are unacceptable from a TCO perspective. And don't get me started on the IoT cold-chain telemetry being bolted on like an afterthought. Real-time traceability requires deterministic data lineage, not just barcode scans. We're optimizing for compliance, not resilience.
Yeah sure, it's all very impressive until you realize this whole system exists because pharmaceutical companies spent decades lobbying to avoid real price regulation. Now they get to charge $1000 for insulin and then brag about how they 'prevent counterfeits.' Meanwhile, people are still splitting pills or skipping doses because they can't afford the real ones. This isn't safety - it's branding.
Okay but like... why does every pill need a barcode? 🤨 I just want my anxiety meds to not be poison. Also, why is this only for prescriptions? My OTC painkillers are way more likely to be bought off some sketchy website. This feels like a solution looking for a problem... or maybe just a way to make tech vendors rich.
I’ve worked in a pharmacy for 12 years. The scanners are a nightmare. We get 12 false alerts a day. Half the time it’s just bad printing. The staff are already burned out. This system adds stress, not safety, for the people on the ground. I’m glad it works for big chains. But for us? It’s another tax on compassion.
The ATP verification system is actually one of the quietest success stories here. 99.8% accuracy at 50k checks/day? That’s clean. And the 2022 infant formula trace-back? Perfect example of why this matters. Small wins add up.
Honestly I didn’t even know this existed until I read this. But now I’m weirdly impressed. Like, I trust my insulin more. And the fact that they tracked 98.7% of vaccines during COVID? That’s insane. We need more systems like this - just... less jargon.
You people are all just patting yourselves on the back. But let’s be real - if this system was so great, why are we still seeing fake opioids in rural towns? Why are people still dying from counterfeit Xanax? This isn’t protection. It’s theater. And the FDA’s ‘success rate’ is just PR spin wrapped in a barcode.