Sinus Infection Symptom Checker
This tool helps you assess if your eye swelling is related to a sinus infection and whether you need medical attention. Based on your symptoms and their duration, it provides guidance on whether your condition is likely viral or bacterial.
Remember: This tool is not a substitute for professional medical advice. Always consult a healthcare provider for serious symptoms.
Seek immediate medical attention if you have:
- Severe eye pain or tenderness
- Redness spreading to the sclera
- Vision changes (blurred, double vision)
- Fever over 38°C (100.4°F) with facial pain
- Rapidly worsening swelling
These signs may indicate serious conditions like orbital cellulitis that require urgent medical care.
Your Assessment
Ever noticed puffiness around your eyes right after a bout of sinus trouble? You’re not alone. Eye swelling often shows up as a side‑effect of sinus infections, but the link isn’t always obvious. This guide walks through why the nose and eyes are so tightly linked, what signs to watch, when to call a doctor, and how to ease the puffiness without over‑reacting.
Eye Swelling is a condition where the tissue around the eye-known as the periorbital area-becomes enlarged due to fluid buildup. It can feel soft or tight and may range from barely noticeable to seriously uncomfortable. Sinus Infection (or sinusitis) refers to inflammation of the sinus cavities, commonly caused by viruses, bacteria, or allergens. When the sinus lining swells, pressure builds up and can spill over into nearby structures, including the eyes.
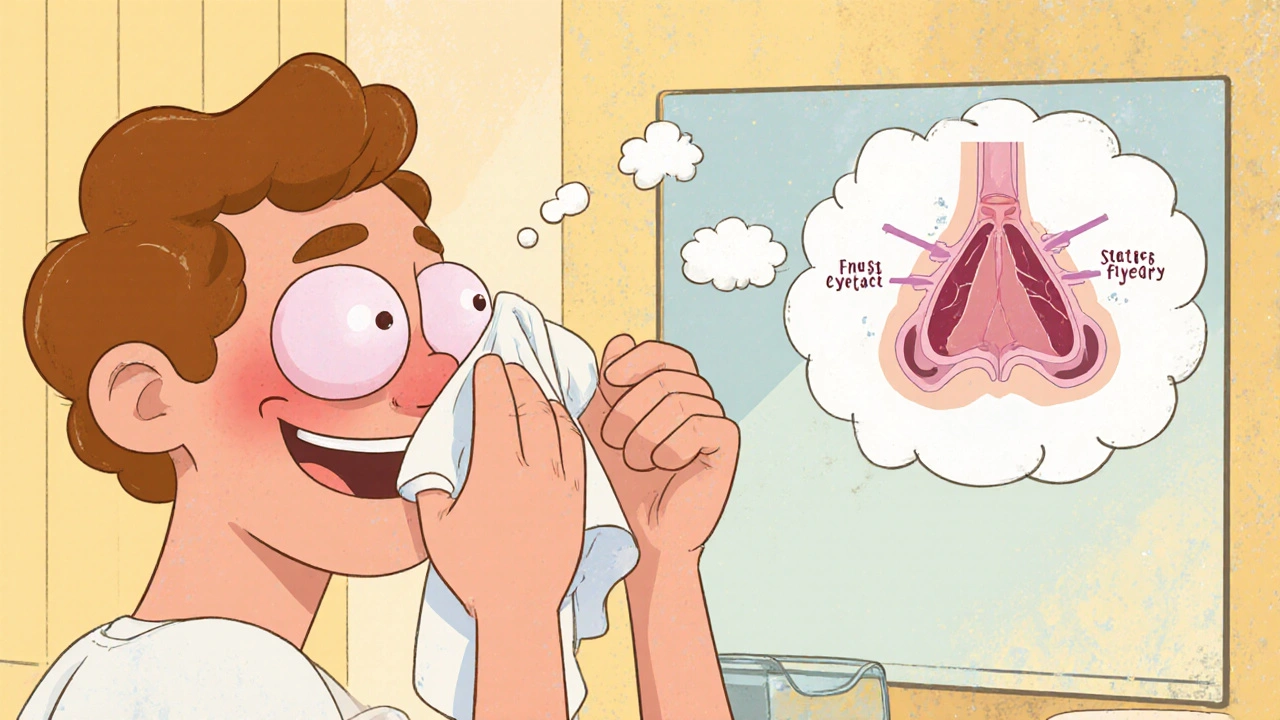
How Sinus Infections Lead to Eye Swelling
The sinuses sit just behind the cheeks, forehead, and the thin bone that separates them from the eyes. When they fill with mucus and become inflamed, several mechanisms can push fluid toward the periorbital space:
- Allergic Rhinitis triggers an immune response that releases histamine, increasing blood vessel permeability. The extra fluid can travel through tiny channels called ethmoidal foramina and cause periorbital edema.
- In bacterial sinusitis, Bacterial Sinusitis produces thick pus that blocks normal drainage. The blockage raises pressure in the maxillary and ethmoid sinuses, forcing fluid into the orbital tissues.
- A viral infection often leads to Viral Sinusitis, where swollen mucosa reduces airflow. The resulting congestion limits the sinus’s ability to equalise pressure, and the excess fluid leaks toward the eyes.
- Sometimes, infection spreads beyond the sinus walls into the eye socket, causing Orbital Cellulitis. This is a serious bacterial infection that directly inflames the tissues around the eye, leading to rapid and painful swelling.
Because the orbit shares blood vessels and lymphatic drainage with the sinuses, any inflammation in one area can quickly affect the other. That’s why a “sinus headache” often feels like a pressure behind the eyes.
Common Causes of Periorbital Edema Linked to Sinus Issues
Not every case of eye puffiness comes from an infection, but here are the most frequent culprits that tie back to sinus problems:
- Acute viral upper respiratory infection - The common cold can cause both nasal congestion and mild eye swelling within days.
- Bacterial sinusitis - Usually follows a viral cold and brings thicker discharge, fever, and more noticeable eye puffiness.
- Allergic reactions - Seasonal pollen or indoor dust can inflame the nasal lining and the eyelids simultaneously.
- Dry indoor air - Low humidity dries out sinus membranes, prompting compensatory swelling that may extend to the eyes.
- Dental infections - Upper tooth abscesses sit close to the maxillary sinus and can trigger radiating inflammation toward the eyes.

When to Seek Medical Care
Eye swelling can be benign, but certain signs signal a need for professional evaluation:
- Severe pain or tenderness around the eye, especially if it worsens with eye movement.
- Redness that spreads to the white of the eye (sclera) or the inner eyelid.
- Vision changes-blurry vision, double vision, or loss of peripheral sight.
- Fever above 38°C (100.4°F) accompanied by facial pain.
- Swelling that develops rapidly within a few hours rather than gradually.
If any of these occur, a doctor may order a CT scan to rule out orbital cellulitis or a subperiosteal abscess-both of which need prompt antibiotics or surgical drainage.
Treatment Options for Eye Swelling Caused by Sinusitis
Management hinges on the underlying cause. Below is a quick decision‑tree you can follow at home before seeing a clinician:
| Feature | Viral Sinusitis | Bacterial Sinusitis |
|---|---|---|
| Onset | Gradual (2-4 days) | Often follows a viral cold, worsens after 5-7 days |
| Discharge | Clear or thin yellow | Thick green/yellow, possibly foul‑smelling |
| Fever | Rare | Common (≥38°C) |
| Eye Swelling | Mild, often bilateral | More pronounced, may be unilateral |
For viral infections, the body usually clears the virus in 7‑10 days. Supportive care includes:
- Stay hydrated to thin mucus.
- Use a Warm Compress on the eyes for 10‑15 minutes, 3‑4 times a day to encourage fluid drainage.
- Apply an over‑the‑counter Nasal Steroid Spray (e.g., fluticasone) to reduce mucosal swelling.
If a bacterial infection is suspected, a doctor will prescribe a short course of antibiotics-typically amoxicillin‑clavulanate or a doxycycline alternative. Alongside antibiotics, these measures help reduce eye puffiness:
- Elevation of the head while sleeping to improve venous return. \n
- Gentle sinus irrigation with a saline neti pot to flush mucus.
- Anti‑inflammatory pain relievers like ibuprofen, which also lower swelling.

Prevention Tips to Keep Both Sinuses and Eyes Happy
Stopping the cycle before it starts saves you from both a stuffy nose and puffy eyes. Try these daily habits:
- Humidify indoor air-Aim for 40‑50% relative humidity, especially in winter when heating dries out the nasal passages.
- Allergy‑proof your home-Use HEPA filters, wash bedding weekly in hot water, and keep windows closed during high pollen days.
- Stay hydrated-At least 2 liters of water a day keeps mucus thin.
- Practice proper nasal hygiene-Gentle saline rinses once daily reduce bacterial load and keep the sinus lining supple.
- Avoid smoking and second‑hand smoke-Tobacco irritates both nasal and ocular mucosa, increasing inflammation.
When you feel a cold coming on, start these measures early. Early intervention can prevent the sinus cavity from becoming a breeding ground for bacteria, which in turn keeps eye swelling at bay.
Frequently Asked Questions
Can sinus infections cause one‑sided eye swelling?
Yes. If the infected sinus is on the same side as the swelling-usually the maxillary or ethmoid sinus-the fluid tends to collect in the adjacent periorbital tissue, leading to unilateral puffiness.
Is a warm compress safe for an infected eye?
A warm compress is safe for mild swelling caused by sinus pressure. However, if you suspect orbital cellulitis-painful, red, and rapidly expanding swelling-skip home remedies and seek urgent care.
Do antihistamines help with eye swelling from sinusitis?
Antihistamines reduce allergic inflammation, which can lessen both nasal congestion and eyelid edema. They’re most effective when the swelling is allergy‑driven rather than purely bacterial.
How long does sinus‑related eye swelling usually last?
Mild swelling often resolves within 3‑5 days as the sinus infection clears. Persistent or worsening swelling after a week warrants medical evaluation.
Can dental infections cause eye swelling?
Upper teeth share roots with the maxillary sinus. An abscess can push infection into the sinus, which may then track up to the orbit, causing eye puffiness.
Understanding the tie between sinuses and eyes empowers you to act fast, keep discomfort low, and know exactly when professional help is needed.




Comments
When your sinuses get blocked, the pressure can push fluid into the soft tissue around the eye. This is why you often see that puffy, tender feeling under the brow after a cold. The fluid collects in the periorbital space because the bone separating the sinuses from the orbit is very thin. Keeping the nasal passages clear can help the fluid drain back where it belongs. Warm compresses and a good saline rinse are simple ways to speed up that process.
The whole situation feels like a slow leak that never stops, draining any optimism you might have. Even a mild sinus flare can turn your face into a swamp of moisture and frustration. It’s hard to ignore the constant tug of discomfort that seems to follow you around. You end up waiting for relief that seems perpetually out of reach.
Did you ever notice how the big pharma lobby pushes a narrative that downplays the real link between sinus infections and eye swelling? They want you to think it’s just a harmless side effect, while the truth is a coordinated campaign to sell you endless decongestant sprays. The secret is that the same inflammatory pathways are being weaponized to keep you dependent. If you look deeper, you’ll see the hidden agenda to keep the market saturated with over‑the‑counter remedies. It’s almost as if they’re feeding the cycle on purpose, ensuring you never get a clean break.
Let’s break down what’s actually happening in clinical terms. The ethmoidal foramina act as conduits for excess interstitial fluid when the mucosal lining swells, allowing periorbital edema to develop. Nasal steroid sprays can down‑regulate the cytokine cascade, reducing both sinus congestion and the secondary eye puffiness. Meanwhile, gentle sinus irrigation helps clear the bacterial load, decreasing the pressure gradient that pushes fluid toward the orbit. These interventions target the root cause rather than just masking the symptoms.
The sinus‑eye nexus is a well‑documented anatomical fact.
Ah, the ever‑so‑trivial observation of the sinus‑eye connection, how utterly groundbreaking.
One would think that after centuries of medical research, we’d have moved beyond such elementary remarks.
But fine, let’s keep patting ourselves on the back for stating the obvious.
Actually the information you shared is correct and helpful for anyone dealing with periorbital edema
It’s important to recognize that the relationship between sinus pathology and ocular manifestations is not merely anecdotal but supported by a cascade of physiological mechanisms.
First, the mucosal lining of the paranasal sinuses becomes inflamed during viral or bacterial infections, leading to increased vascular permeability.
This permeability allows plasma proteins and fluid to exude into the surrounding interstitial spaces.
Because the ethmoidal and maxillary sinuses lie in direct proximity to the orbital septum, the excess fluid can track along the perivascular sheaths into the periorbital region.
Furthermore, the lymphatic drainage of the sinuses shares common pathways with the orbital lymphatics, meaning that any bottleneck in sinus drainage can cause a backup that manifests as eyelid swelling.
Clinically, patients often report a sensation of pressure behind the eyes that worsens when they bend forward, highlighting the gravitational component of fluid migration.
Therapeutic strategies, therefore, must address both the primary sinus inflammation and the secondary orbital edema.
Topical nasal corticosteroids act by downregulating NF‑κB signaling, thereby reducing cytokine production and edema formation at the source.
Simultaneously, applying warm compresses to the eyelids promotes vasodilation, enhancing reabsorption of the accumulated fluid.
Saline irrigation can mechanically clear mucus plugs, re‑establishing patency of the ostiomeatal complex and alleviating the pressure gradient that drives fluid into the orbit.
Patients should also be advised to maintain head elevation during sleep to facilitate venous drainage from the periorbital tissues.
In cases where bacterial superinfection is suspected-evidenced by purulent discharge and fever-empiric antibiotics covering Streptococcus pneumoniae and Haemophilus influenzae are warranted.
However, indiscriminate antibiotic use should be avoided to prevent resistance.
Finally, if rapid progression of swelling is observed, especially with pain on eye movement or visual disturbances, urgent imaging is essential to rule out orbital cellulitis or abscess formation.
In summary, a multimodal approach that combines anti‑inflammatory therapy, mechanical drainage, and vigilant monitoring offers the best chance for rapid resolution of sinus‑related eye swelling.
One could argue that the eye, as a reflective surface, mirrors the internal turbulence of our sinus passages.
The swelling becomes a physical manifestation of the unseen battles waged within the mucosa.
When the pressure escalates, it is as if the body signals its fragility through the most vulnerable window.
Understanding this interplay invites a more compassionate approach to self‑care.
Thus, simple measures like hydration and gentle warmth become not just remedies but gestures of respect toward our own physiology.