For decades, proving that a generic drug works just like its brand-name counterpart meant running expensive, time-consuming clinical trials with human volunteers. You’d measure blood samples over hours, compare absorption rates, and hope the numbers lined up. But that’s changing - fast. Since 2023, bioequivalence testing has been transformed by new tools that don’t just speed things up, they make them smarter, more precise, and far less costly. The goal hasn’t changed: ensure every pill you take performs the same way. But how we prove it? That’s been completely rewritten.
AI Is Now the Default Assistant in Bioequivalence Labs
The FDA’s BEAM a data and text analysis tool launched in Q2 2024 isn’t science fiction - it’s in daily use. BEAM automates the grunt work: pulling data from hundreds of studies, flagging inconsistencies, even suggesting statistical adjustments. Before BEAM, reviewers spent over 60 hours per application just sorting through raw data. Now, that’s cut to under 10. In pilot testing, reviewer workload dropped by 52 hours per application. That’s not efficiency - it’s a revolution.
Behind BEAM is machine learning trained on over 12,000 historical bioequivalence studies. It doesn’t just find patterns - it predicts them. If a dissolution profile looks odd, BEAM cross-references it with thousands of similar cases and flags potential issues before a human even sees it. This isn’t replacing scientists; it’s giving them superpowers. By 2030, experts predict AI-driven analysis will handle 75% of standard generic applications. For simple small-molecule drugs, this means faster approvals and lower costs. For patients, it means getting affordable meds sooner.
Virtual Trials Are Replacing Human Studies - For Some Drugs
Remember when you needed 50-100 healthy volunteers to test a generic? Now, for certain complex products, you might not need any. The virtual bioequivalence platform a FDA-funded project launched in August 2024 uses computer models to simulate how a drug behaves in the body. It combines pharmacokinetic data, tissue absorption models, and real-time physiological variables to predict bioavailability without a single blood draw.
This isn’t theoretical. In a 2025 FDA pilot, virtual BE reduced the need for clinical endpoint studies by 65% for oral extended-release formulations. That’s huge. For drugs like those used in epilepsy or blood thinners - where tiny differences can be dangerous - this level of precision was impossible before. Now, regulators can simulate hundreds of virtual patients with different body types, metabolisms, and gut conditions. If the model predicts consistent performance across all scenarios, clinical trials become unnecessary.
But it’s not for everything. For transdermal patches or inhalers, where skin adhesion or lung deposition matters, virtual models still need real-world validation. That’s why the FDA is also investing in advanced imaging.
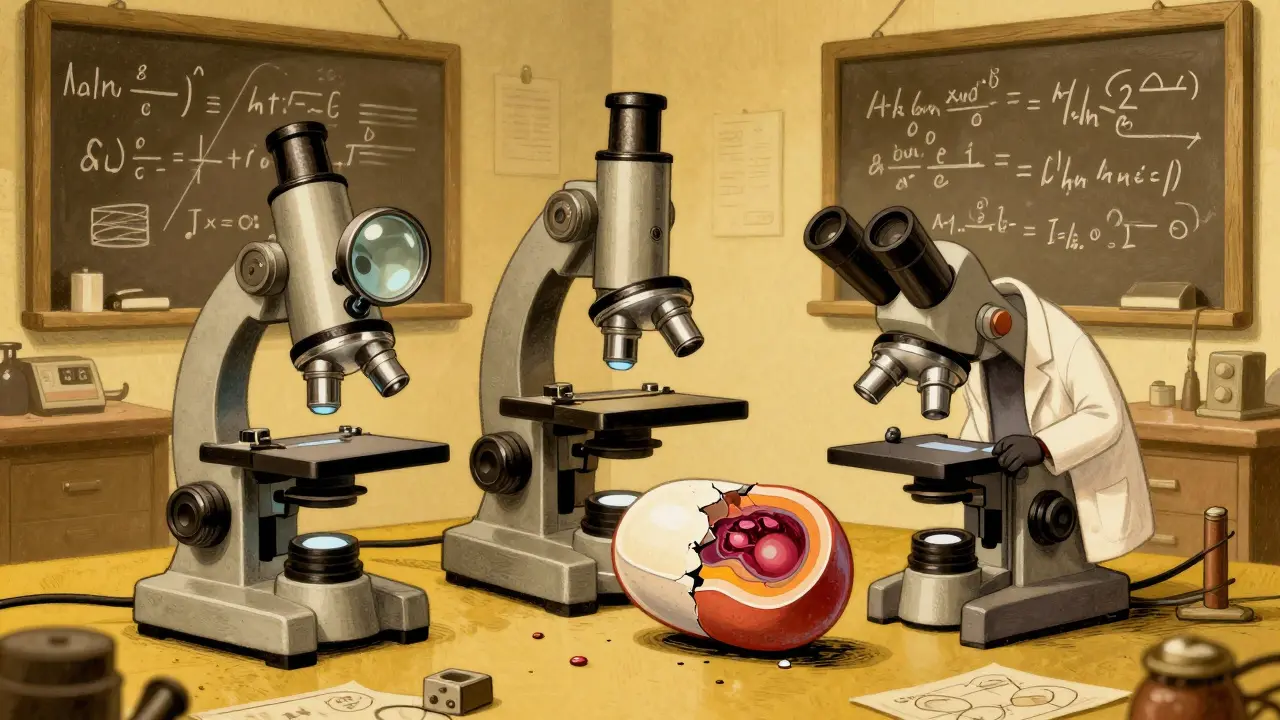
Seeing the Unseen: Imaging Tech That Reveals Drug Behavior
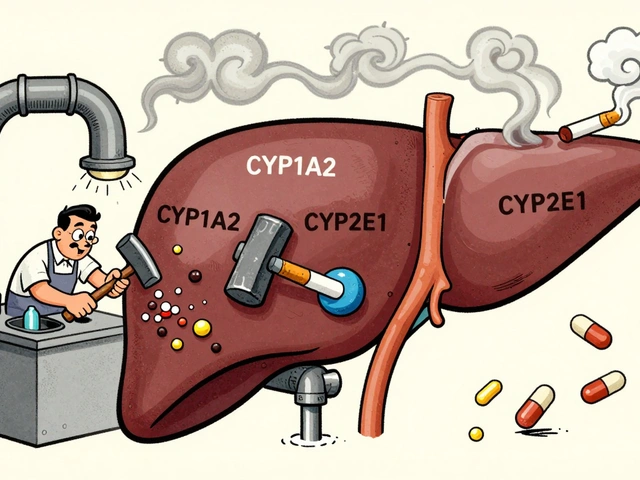
Traditional dissolution tests just measure how fast a pill breaks down in a beaker. But pills don’t dissolve in beakers - they dissolve in the stomach, with bile, enzymes, and varying pH levels. That’s why the Dissolvit system a proprietary in vitro dissolution testing system for complex formulations was developed. It mimics real human digestive conditions with precision.
But Dissolvit alone isn’t enough. To truly understand how a drug behaves, scientists now use tools like:
- Scanning electron microscopy (SEM) - to see how coating layers crack under simulated stomach conditions
- Optical coherence tomography - to track how a patch adheres to skin in real time
- Atomic force microscopy infrared spectroscopy - to map chemical distribution within a tablet down to the micrometer
These aren’t just fancy microscopes. They’re diagnostic tools that reveal why a generic might fail - not because the active ingredient is wrong, but because the coating, particle size, or manufacturing process is slightly off. One 2025 study showed that a generic inhaler looked identical under standard tests but had 12% less drug delivery to the lungs. SEM caught the issue: uneven particle clustering. Without imaging, that difference would’ve gone unnoticed - and patients would’ve been underdosed.
Regulatory Harmonization: One Rule for the Whole World
Before 2024, getting a generic approved in the U.S. and Europe meant jumping through two different sets of hoops. The FDA had one set of bioanalytical standards. The EMA had another. Validation took longer. Data had to be re-run. Costs piled up.
That changed with the adoption of the ICH M10 guideline a unified framework for bioanalytical method validation adopted by FDA in June 2024. Now, labs worldwide follow the same rules for validating tests - from sample handling to data reporting. The result? A 62% drop in method validation discrepancies between regions. That means faster global approvals, fewer redundant tests, and lower prices for patients everywhere.
This harmonization also helps smaller countries. In the Middle East and Africa, governments are using ICH M10 as a blueprint to build their own bioequivalence labs. Saudi Arabia’s Vision 2030 and UAE partnerships with global CROs have led to new testing centers in Riyadh and Dubai. This isn’t just about compliance - it’s about access.
Costs Are Falling - But Not for Everything
Here’s the math: a traditional bioequivalence study for a simple generic still costs $1-2 million. Add AI, imaging, and virtual modeling? That jumps to $2.5-4 million. So why switch?
The answer is volume. For a company making 10 generics a year, using advanced methods might cost more upfront. But with BEAM cutting review time by 50% and virtual BE eliminating 65% of clinical trials, the total time-to-market drops from 18 months to under 10. That’s a $10 million savings in lost sales alone.
For biosimilars - complex biologic drugs that mimic biologics like Humira or Enbrel - the savings are even clearer. There’s no way to test these with old methods. They’re too big, too fragile. AI-driven IVIVC (in vitro-in vivo correlation) models are the only way forward. As of October 2025, the FDA had approved 76 biosimilars - up from just 12 in 2020. Most of them relied on these new technologies.
But here’s the catch: for simple, small-molecule generics, old-school PK studies are still cheaper. If your drug is a 500mg tablet of ibuprofen, you don’t need SEM or AI. A standard crossover trial works fine. The tech is saving money - but only where it matters most.
What’s Still Holding Back the Future?
Not everything is solved. The FDA’s October 2025 pilot program requires bioequivalence testing to be done in the U.S. using only domestically sourced active pharmaceutical ingredients (APIs). That’s a big hurdle for global manufacturers. It also means labs outside the U.S. can’t yet use these advanced tools to support U.S. approvals.
Then there’s the risk of over-reliance. Dr. Michael Cohen of ISMP warned that for drugs with a narrow therapeutic index - like warfarin or digoxin - skipping clinical correlation could be dangerous. If a virtual model says a generic is equivalent, but real patients react differently? That’s a safety gap. That’s why the FDA still requires at least one clinical study for high-risk products - even when using AI.
And for transdermal systems? Adhesion and skin irritation are still messy. No imaging tool can perfectly predict how a patch will behave over 72 hours on different skin types. The FDA is still working on standardized methods for this.
What’s Next? The Road to 2027 and Beyond
The FDA’s roadmap is clear: by 2027, 90% of generic applications must be reviewed within 10 months. That’s only possible with AI and virtual models. BEAM will be rolled out nationwide by Q2 2026. New in vitro models for peptides, oligonucleotides, and ophthalmic drugs are in development. The goal? To eliminate the need for human trials for 80% of generic drugs.
But the real win isn’t just speed or cost. It’s accuracy. These tools catch problems that humans miss. They prevent underdosed inhalers, inconsistent patches, and faulty coatings before they reach patients. In the end, bioequivalence testing isn’t just about proving drugs are the same - it’s about proving they’re safe. And with these advances, we’re getting better at that every day.
What is bioequivalence testing and why does it matter?
Bioequivalence testing proves that a generic drug delivers the same amount of active ingredient into the bloodstream at the same rate as the brand-name version. If two drugs are bioequivalent, they’re expected to have the same clinical effect. This is critical because patients rely on generics for affordable, consistent treatment - especially for chronic conditions like high blood pressure or diabetes.
How is AI changing bioequivalence testing?
AI tools like BEAM automate data analysis, flag inconsistencies, and predict outcomes based on thousands of past studies. This cuts review times by 40-50% and reduces human error. Instead of manually comparing blood concentration curves, reviewers now get AI-generated insights that highlight risks and similarities - making approvals faster and more reliable.
Can virtual bioequivalence replace human trials entirely?
For some complex products - like extended-release tablets or certain inhalers - yes. Virtual BE platforms simulate how a drug behaves in the body using advanced modeling. In FDA trials, this reduced the need for clinical studies by 65%. But for high-risk drugs (like blood thinners) or delivery systems with variable absorption (like patches), at least one human study is still required to ensure safety.
Why are advanced imaging techniques like SEM important?
Traditional dissolution tests only measure how fast a pill dissolves in liquid. But real bodies aren’t beakers. SEM, optical coherence tomography, and other imaging tools show how coatings crack, how particles cluster, and how drugs release in real-time under realistic conditions. This catches manufacturing flaws that standard tests miss - preventing underdosed or ineffective generics from reaching patients.
What’s the biggest challenge facing new bioequivalence technologies?
The biggest challenge is regulatory and practical overlap. While AI and virtual models work well for oral drugs, they struggle with transdermal systems (patches), inhalers, and topical creams where skin or lung behavior is complex. Also, the FDA’s new rule requiring U.S.-based testing with domestic APIs limits global participation. Balancing innovation with patient safety - especially for narrow therapeutic index drugs - remains the tightrope walk.