Medication Emergency Checker
Check for Emergency Symptoms
Select any symptoms you or someone else is experiencing that started within 72 hours of starting a new medication or changing your dose.
Select symptoms to get results
Most people know that medications can cause side effects - nausea, dizziness, dry mouth. But when does a side effect become a life-threatening emergency? The difference isn’t always obvious. You might wait too long thinking it’s just a bad reaction, only to realize later you needed help right away. Every year, over 100,000 people in the U.S. die from adverse drug reactions. Many of these deaths are preventable - if you know what to watch for.
What Counts as a Medication Emergency?
Not every bad reaction needs the ER. But some symptoms mean your body is shutting down. These aren’t "maybe" situations. They’re red flags that demand immediate action.- Difficulty breathing or wheezing - even if it feels like an asthma attack
- Swelling of your lips, tongue, or throat
- Blue or gray lips or fingernails
- Severe rash with blistering or peeling skin
- Sudden, crushing chest pain or pressure
- Slurred speech, weakness on one side of your body, or sudden confusion
- Heart rate below 50 or above 110 beats per minute
- Blood pressure above 180/120 with headache, dizziness, or vision changes
- Temperature above 102°F with confusion or stiff neck
- Loss of consciousness or collapse
If you’re taking a new medication - or if your dose was just changed - and you develop any of these within 72 hours, don’t wait. Call emergency services. These aren’t side effects you can "wait out." They’re signs your body is having a dangerous reaction.
Anaphylaxis: The Silent Killer
Anaphylaxis is the most dangerous allergic reaction to medications. It can start with mild itching or a rash, then turn deadly in minutes. People often mistake it for anxiety, a cold, or a bad flu. That’s why it’s misdiagnosed in 35% of cases.Penicillin, sulfa drugs, and certain antibiotics are the most common triggers. But even over-the-counter painkillers like ibuprofen can cause it. The key is speed. If you have an epinephrine auto-injector (like an EpiPen), use it immediately. Then call 911. Even if you feel better after the shot, you still need emergency care. A second wave of symptoms can hit hours later.
One patient on Reddit shared how she waited four hours after starting amoxicillin because she thought the rash was "just an allergy." By the time she got to the ER, her throat was closing. She survived - but barely.
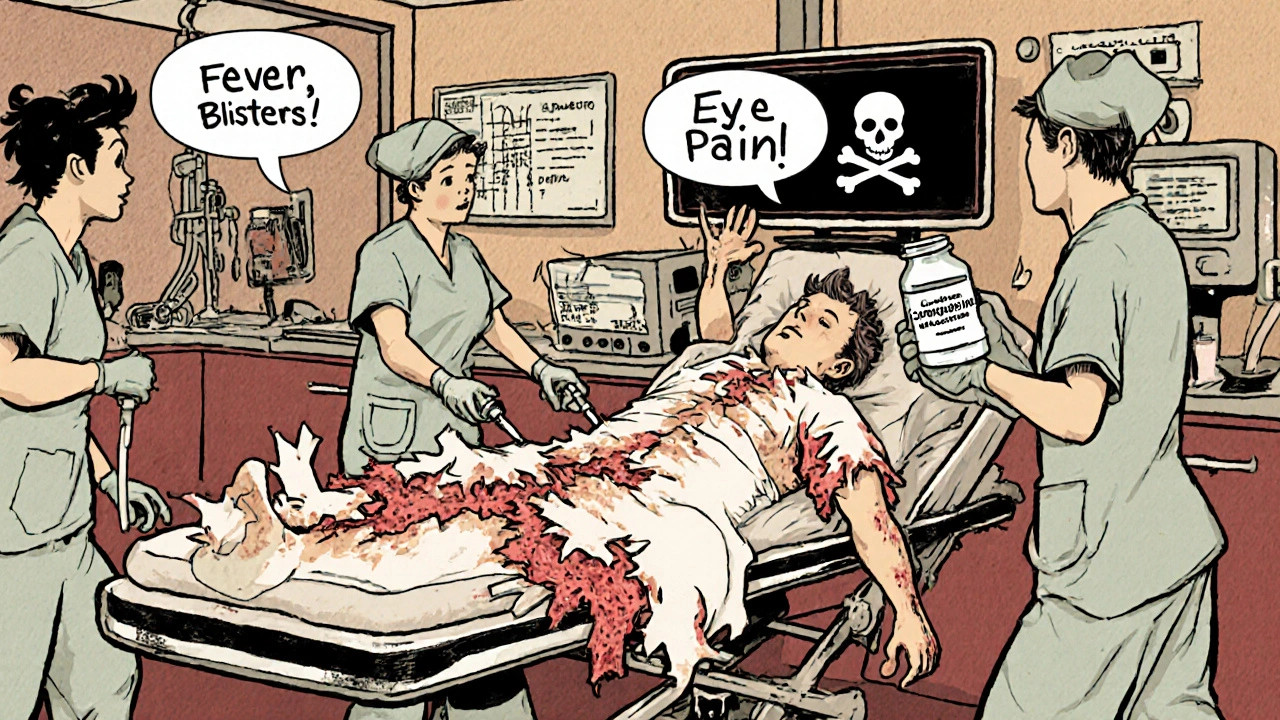
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis
These are rare but deadly skin reactions. They often start like the flu - fever, sore throat, fatigue. Then, within days, your skin begins to blister and peel. Your eyes, mouth, and genitals can become covered in painful sores.Drugs linked to these conditions include antibiotics (like sulfonamides), anticonvulsants (like carbamazepine), and pain relievers like allopurinol. If you notice your skin turning red, blistering, or peeling - especially if you also have mouth sores or eye pain - go to the ER. This isn’t a rash you can treat with cream. It’s a medical emergency that requires hospitalization.
Drug Interactions That Can Kill
Most adverse reactions aren’t allergies. They’re interactions. If you’re taking three or more medications, your risk jumps dramatically. Over 15,000 drug interactions are documented. About 700 are serious enough to cause death.One of the most dangerous combinations? Warfarin (a blood thinner) with NSAIDs like ibuprofen or naproxen. Studies show this mix increases bleeding risk by 50%. Another deadly combo: warfarin with antibiotics like ciprofloxacin. These can spike your INR (a blood clotting test) to dangerous levels within 24 to 48 hours - leading to internal bleeding or stroke.
Herbal supplements are just as risky. St. John’s Wort, often taken for depression, can interfere with antidepressants, birth control, and heart medications. It’s not "natural" in the safe sense - it’s a powerful drug that can change how your body handles other medicines.
High Blood Pressure and Stroke Risk
A blood pressure reading of 180/120 sounds scary. But if you’re not dizzy, confused, or having trouble speaking, you might not need the ER - yet. That’s a hypertensive urgency, not an emergency.But if that same number comes with slurred speech, sudden weakness, vision loss, or a severe headache? That’s a stroke waiting to happen. It’s called a hypertensive emergency. You need IV medication in the hospital - right now.
Many people with high blood pressure don’t feel symptoms until it’s too late. That’s why checking your pressure regularly matters - especially if you’ve recently started or changed a medication like a steroid, decongestant, or NSAID.
What to Do If You’re Unsure
You’re not supposed to be a doctor. But you are responsible for your own safety. Here’s a simple rule: if you’re asking yourself, "Should I go to the ER?" - the answer is probably yes.Ask yourself these questions:
- Did this start within 72 hours of starting a new drug or changing a dose?
- Is it getting worse fast - not better?
- Are you having trouble breathing, speaking, or thinking clearly?
- Do you feel like you’re going to pass out?
If you answered yes to any of these, don’t call your doctor’s office. Don’t wait until morning. Call 911 or go to the nearest emergency room.
Even if it turns out to be nothing, you’re safe. But if you wait and it’s something serious - you might not get a second chance.
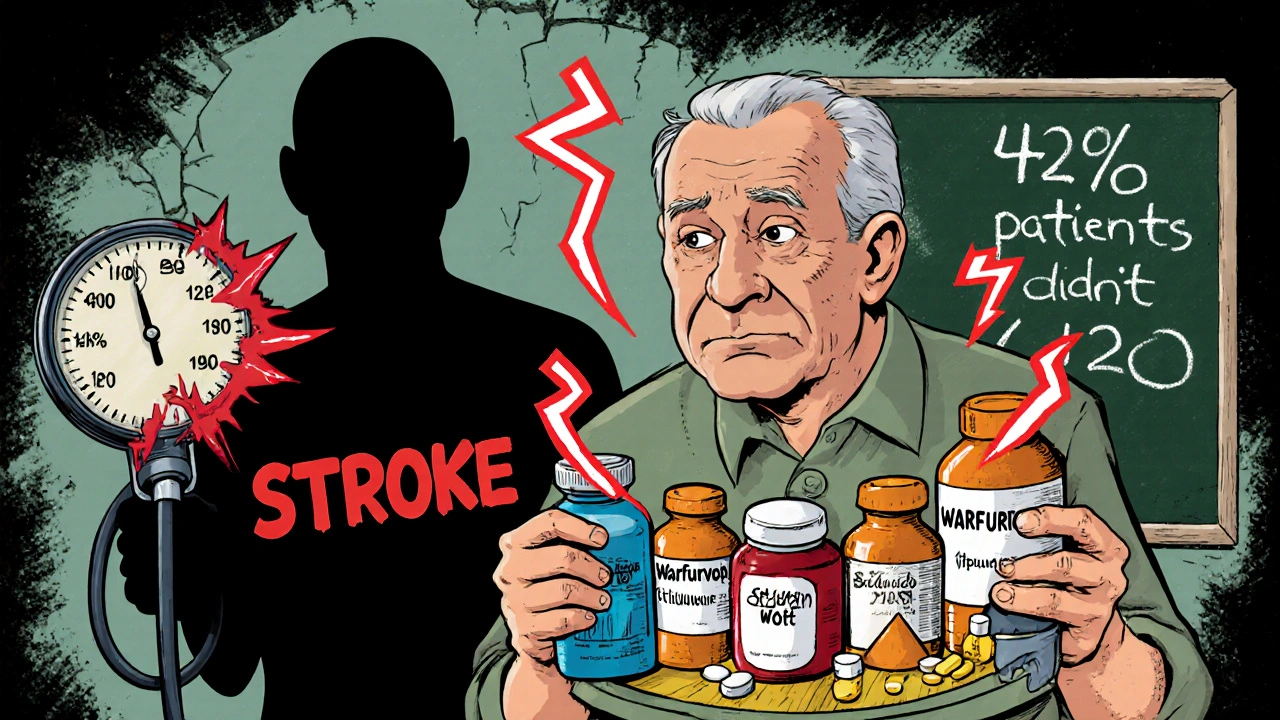
Why So Many People Get It Wrong
Only 42% of patients get clear instructions from their doctor or pharmacist about when to seek emergency care. Most medication labels just say "call your doctor if side effects occur." That’s not enough.Patients often confuse expected side effects with dangerous ones. Mild nausea with antibiotics? Normal. Vomiting nonstop for 12 hours with dizziness and dry mouth? That’s dehydration - and it can lead to kidney failure.
One Mayo Clinic survey found that 61% of patients didn’t know whether their symptoms required emergency care. That’s not their fault. It’s a system failure.
How to Protect Yourself
You can’t control every drug interaction - but you can control your awareness.- Keep a list of every medication you take - including supplements, vitamins, and herbal products. Bring it to every appointment.
- Ask your pharmacist: "What are the red flags I should watch for with this medicine?"
- If you’re on blood thinners, know your target INR range and when to get tested.
- If you have a history of severe allergies, carry an epinephrine auto-injector and wear a medical alert bracelet.
- Don’t mix new medications without checking with a professional - even if they’re "over-the-counter."
Medication safety isn’t just about taking pills correctly. It’s about knowing when to act - fast.
What’s Being Done to Fix This
Hospitals and pharmacies are starting to catch on. The FDA now requires clearer emergency warning labels on 78% of new drugs - up from 42% in 2018. Pharmacist-led medication reviews are now covered by Medicare for high-risk patients, and they’ve reduced ER visits for drug reactions by 18%.AI tools are being tested to predict who’s most at risk based on their genetics and medication history. These systems can flag dangerous combinations before you even take the pill.
But until these systems are everywhere, the most powerful tool you have is your own awareness. You’re the first line of defense.
Can I wait to see my doctor if I think I’m having a bad reaction to a medication?
No - not if you’re experiencing symptoms like trouble breathing, swelling, chest pain, slurred speech, or loss of consciousness. These are emergency signs. Calling your doctor’s office or waiting for an appointment could cost you your life. Go to the ER or call 911 immediately. Mild side effects like nausea or dizziness can wait, but life-threatening reactions cannot.
What if I’m not sure whether my reaction is serious?
If you’re unsure, err on the side of caution. Emergency care is for when you’re asking yourself, "Should I go?" - not when you’re certain you’re fine. Many people who survive severe reactions say they delayed help because they thought it was "just a side effect." When in doubt, call emergency services. It’s better to be checked and found safe than to wait and risk irreversible damage.
Are herbal supplements safe to take with prescription drugs?
No - not without checking. Supplements like St. John’s Wort, ginkgo biloba, and garlic can dangerously interact with blood thinners, antidepressants, and heart medications. They’re not regulated like prescription drugs, so their strength and effects vary. Always tell your doctor and pharmacist exactly what supplements you’re taking - even if you think they’re "natural" or "harmless."
How long after starting a new medication should I be worried about side effects?
The highest risk window is the first 72 hours after starting a new medication or changing the dose. That’s when 68% of severe reactions occur. But dangerous reactions can still happen days or weeks later, especially with drugs like antibiotics, blood thinners, or anticonvulsants. Stay alert for the first two weeks, and don’t ignore new symptoms - even if they seem minor at first.
Can I use an epinephrine auto-injector if I think I’m having an allergic reaction?
Yes - if you have one and you’re experiencing signs of anaphylaxis (swelling, trouble breathing, dizziness, rash), use it immediately. Epinephrine is the only treatment that can stop a deadly allergic reaction. Don’t wait to see if it gets worse. After using it, call 911. Even if you feel better, you need to be monitored - a second wave of symptoms can happen hours later.




Comments
This is so important 🚨 I had a friend go into anaphylaxis from ibuprofen and she thought it was just a rash. Took her 3 hours to get help. Don't wait. Period.
Ugh. Another ‘you’re not a doctor’ lecture. Newsflash: most people don’t need a PhD to know when their lips are swelling shut. The real problem? Doctors who treat meds like candy and don’t even mention the red flags. I’ve seen it a hundred times - ‘oh it’s just side effects’ - until the patient’s in a body bag. Stop normalizing ignorance.
stevens johnson is legit terrifying. my cousin got it from allopurinol. skin started peeling off like a sunburn but 100x worse. he was in icu for 3 weeks. no joke - if your skin looks like it’s melting, GO. NOW. not tomorrow. not after work. now.
i didn't know warfarin and ibuprofen could be deadly together. i've been taking both for years. i'm gonna call my pharmacist tomorrow. thanks for the heads up. this stuff should be on every prescription bottle.
Let’s be brutally honest: 61% of patients don’t know what to do? That’s not a failure of education - it’s a failure of the American healthcare system’s inability to communicate in plain language. We’ve got AI predicting drug interactions, yet patients are left to Google symptoms at 2 a.m. while their INR skyrockets. This isn’t just negligence - it’s systemic malpractice dressed up as ‘informed consent.'
There’s a quiet truth here: we’re taught to trust pills, not our bodies. We’re told side effects are normal, so we numb ourselves to warning signs. But your body doesn’t lie - it screams in ways we’ve been trained to ignore. The real emergency isn’t the reaction. It’s the culture that tells us to wait it out.
St. John’s Wort is a sneaky one - it’s not ‘natural’ like herbal tea, it’s a potent CYP450 modulator that can tank your SSRIs or birth control efficacy. If you’re on anything metabolized by the liver, treat supplements like pharmaceuticals. I’ve seen patients crash into serotonin syndrome because they thought ‘botanical’ meant ‘safe.’ Spoiler: it doesn’t.
I just started a new blood pressure med and I’ve been checking my numbers twice a day. I didn’t know the 72-hour window was so critical. This post made me feel less alone. Thanks for writing this. I’m sharing it with my mom.