Pramipexole Dose Calculator
Kidney Function Assessment
Enter your estimated glomerular filtration rate (eGFR) to calculate the appropriate pramipexole dose.
Note: eGFR should be determined by your healthcare provider using validated formulas like CKD-EPI.
Living with a chronic movement disorder means you’ll hear a lot about medication trade‑offs. One drug that shows up repeatedly is pramipexole. While it can smooth out tremors and stiffness, many patients wonder what happens after years of use. This guide breaks down the science, the pros and cons, and what you should keep an eye on if you stay on the drug long‑term.
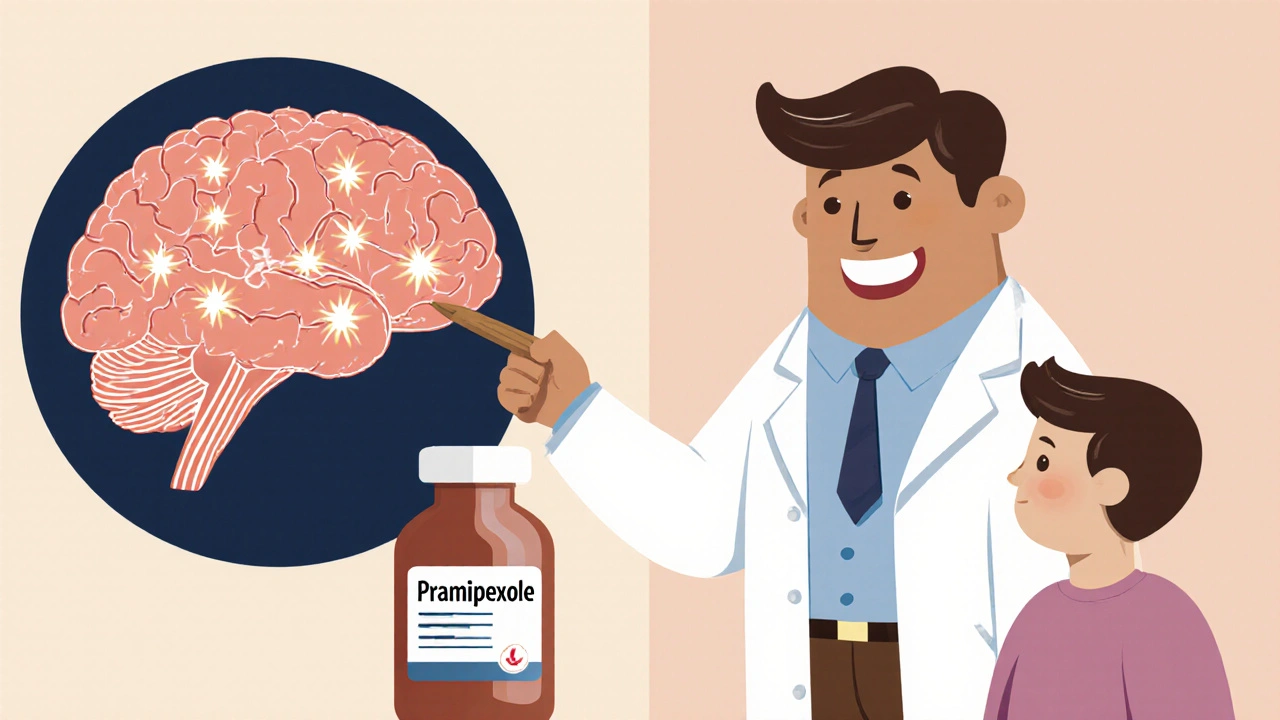
What Is Pramipexole?
Pramipexole is a non‑ergoline dopamine agonist that mimics dopamine activity in the brain. It was first approved by the FDA in 1997 for Parkinson’s disease and later for restless‑leg syndrome (RLS). By binding to dopamine D2 and D3 receptors, it helps restore the signaling that’s lost as nerve cells die.
How Pramipexole Works in the Brain
Dopamine is a key neurotransmitter for smooth, purposeful movement. In Parkinson’s disease, dopamine‑producing neurons gradually disappear, leading to stiffness, tremor, and slowed motion. Pramipexole’s job is to sit on the same receptors that dopamine would normally hit, keeping the motor circuit active even when natural dopamine levels are low.
Approved Uses and Typical Dosing
- Parkinson’s disease - started at 0.125 mg three times daily and titrated up to 4.5 mg/day depending on response.
- Restless‑leg syndrome - usually 0.125 mg once daily, increasing to a maximum of 0.5 mg/day.
Both conditions rely on gradual dose escalation to minimize early side effects such as nausea or dizziness.
Pharmacokinetics: How the Body Handles Pramipexole
Pramipexole is absorbed quickly, reaching peak plasma levels within 2-3 hours. It has a long half‑life of about 8-12 hours, allowing for multiple‑daily dosing. Roughly 90 % of the drug is eliminated unchanged via the kidneys, so kidney function must be checked regularly, especially in older adults.

Long‑Term Benefits: What the Evidence Shows
Studies following patients for up to 5 years report sustained improvements in motor scores (UPDRS Part III) and quality‑of‑life questionnaires. In the CALM‑PD trial, participants on pramipexole maintained a 30 % reduction in ‘off’ time compared with a 10 % reduction in the placebo group. For RLS, long‑term use reduces leg‑movement frequency by about 50 % and improves sleep efficiency.
Potential Long‑Term Risks
Every medication carries trade‑offs. Below are the most commonly reported issues after months or years of therapy.
- Impulse control disorders (ICDs) - gambling, compulsive shopping, or hypersexuality can emerge in 5‑10 % of patients, especially at higher doses.
- Hallucinations and psychosis - visual or auditory hallucinations rise in prevalence after 2‑3 years, particularly in those with dementia.
- Sudden sleep attacks - patients may fall asleep without warning, increasing fall risk.
- Orthostatic hypotension - a drop in blood pressure upon standing can cause dizziness or fainting.
- Cardiac valvulopathy - dopamine agonists have been linked to mild valve thickening; routine echocardiograms are advised for high‑risk individuals.
- Oxidative stress concerns - animal studies suggest prolonged dopamine agonist exposure may increase free‑radical formation, though human data are limited.
Monitoring Recommendations for Long‑Term Use
Regular check‑ups can catch problems early.
- Renal function: serum creatinine and estimated GFR every 6‑12 months.
- Cardiac screening: baseline echocardiogram, then repeat every 2 years if risk factors exist.
- Neuropsychiatric evaluation: ask about gambling, shopping urges, or unusual thoughts at each visit.
- Blood pressure: measure lying and standing scores to spot orthostatic drops.
- Motor assessment: UPDRS or MDS‑UPDRS scores quarterly to gauge effectiveness.
If any red flag appears, your doctor may lower the dose, switch to a different dopamine agonist, or add a levodopa regimen.
Pramipexole vs. Ropinirole: A Quick Comparison
| Attribute | Pramipexole | Ropinirole |
|---|---|---|
| Approved Indications | Parkinson’s disease, Restless‑leg syndrome | Parkinson’s disease, Restless‑leg syndrome |
| Typical Max Dose | 4.5 mg/day | 24 mg/day |
| Half‑Life | 8-12 hours | 6 hours |
| Renal Excretion | ~90 % | ~50 % |
| ICD Rate (high dose) | ~8 % | ~5 % |
| Common Side Effects | Nausea, dizziness, sleepiness | Dry mouth, fatigue, nausea |
Both drugs share the same class, but pramipexole’s higher renal clearance makes dose adjustments easier in patients with kidney issues. Ropinirole, on the other hand, offers more flexible dosing for those who need a lower pill burden.
Practical Tips for Patients on Pramipexole
- Start low, go slow - the titration schedule minimizes nausea and dizziness.
- Take doses with food if you experience stomach upset.
- Set a regular bedtime - the drug’s long half‑life can interfere with sleep cycles.
- Keep a side‑effect diary - note any urges to gamble, shop, or sudden sleep episodes and share with your clinician.
- Stay hydrated and rise slowly - helps prevent orthostatic drops.
- Inform caregivers - they can spot early signs of impulse control issues.
Frequently Asked Questions
Can I stop pramipexole suddenly?
No. Abrupt discontinuation can trigger a rebound of Parkinson’s symptoms and cause severe nausea. Taper the dose under medical supervision.
Is pramipexole safe for people with kidney disease?
Since about 90 % is cleared renally, dose reduction is usually required for GFR below 30 mL/min. Your doctor will calculate a safe regimen.
What should I do if I notice gambling urges?
Report it immediately. Reducing the dose or switching to another agent often resolves the behavior. A mental‑health professional can also help manage urges.
How often should I have cardiac imaging?
Baseline echo is recommended before starting therapy. If you have a history of heart disease, repeat every 1‑2 years; otherwise, every 3‑5 years is typical.
Can pramipexole cause weight gain?
Weight changes are not a primary side effect, but improved motor function can lead to increased appetite and modest weight gain in some patients.
Understanding the long‑term picture helps you balance the good with the bad. With regular monitoring and open communication, many people stay on pramipexole for years while enjoying steadier movement and better sleep.




Comments
It is essential to keep a regular schedule of renal and cardiac monitoring while on pramipexole. By checking serum creatinine every six months you can adjust the dose before toxicity develops. Likewise, a baseline echocardiogram followed by periodic repeats helps catch early valve changes. Maintaining a side‑effect diary empowers you to notice subtle urges or sleep attacks promptly. Together these steps create a solid safety net for long‑term therapy.
They don’t want you to know how quickly the industry can slip in hidden additives that amplify impulse‑control problems. Every time a new batch hits the shelves, covert trials are run to see if patients develop gambling urges faster. It’s a silent experiment that keeps the profit wheels turning while we suffer the side effects.
Renal clearance accounts for roughly ninety percent of pramipexole elimination, so a glomerular filtration rate below thirty milliliters per minute usually necessitates a 50 % dose reduction. The drug’s half‑life remains unchanged, but accumulation can occur if dosing is not adjusted. Monitoring creatinine clearance at each visit provides the data needed to keep plasma concentrations within the therapeutic window.
The moral responsibility of clinicians extends beyond merely prescribing a dopamine agonist; they must vigilantly guard against the insidious erosion of a patient’s autonomy. When impulse‑control disorders emerge, the individual’s freedom to make sound choices is compromised, and society bears the cost of gambling debts and broken relationships. It is not enough to hand over a medication and hope the patient will self‑monitor; proactive screening is a duty. Regular questionnaires about shopping urges, sexual behavior, and risk‑taking should be integrated into every visit. If red flags appear, dose reduction or a switch to levodopa is not a defeat but an ethical correction. Moreover, families deserve to be informed, because silent progression can devastate households. Transparency about the possible cardiac valvulopathy risk respects the patient’s right to informed consent. The healthcare system should allocate resources for periodic echocardiograms, especially for those with pre‑existing heart disease. In the grand scheme, safeguarding mental health preserves the dignity of those living with chronic movement disorders. Ultimately, the goal is not just smoother movement but a life lived with agency and respect.
Adhering to the monitoring schedule respects both the treatment plan and one’s cultural values of self‑care. Sharing experiences with community members can provide additional support.
Keep a daily log of how you feel after each dose.
Note any sudden drowsiness or unexpected naps.
Record any cravings to gamble, shop, or engage in risky behavior.
Write down blood pressure readings taken while lying down and after standing.
Track kidney function numbers from each lab visit.
Schedule an echocardiogram before starting therapy and repeat it every two years if you have heart risk factors.
Discuss any hallucinations or vivid dreams with your doctor immediately.
Make sure to take the medication with food if the stomach feels upset.
Set a consistent bedtime to help your body adjust to the drug’s half‑life.
Stay hydrated throughout the day to reduce orthostatic drops.
Involve a trusted family member in your appointments to catch subtle changes.
Use a pill organizer to avoid missed or double doses.
Combine physical therapy with medication for optimal mobility gains.
Celebrate small improvements in walking or sleep quality as milestones.
Remember that adjusting the dose is a sign of personalized care, not failure.
The data on cardiac valve thickening is flimsy and often overstated by alarmist blogs. Focus on measurable outcomes like UPDRS scores rather than speculative imaging findings.
I hear the concerns about impulse‑control disorders and sudden sleep attacks, and it’s understandable to feel uneasy. Regular check‑ups and open dialogues with your neurologist can ease that anxiety. Remember that many patients find a balance that maintains quality of life while minimizing risks. Your experience is valid, and you’re not alone in navigating these complexities.
Staying informed about dosage adjustments respects both medical guidance and personal well‑being. Sharing your monitoring results with the care team ensures a collaborative approach.
All of this monitoring is just a way to keep pharmaceutical profits afloat.