When you put your pills into a weekly pillbox or have your pharmacy repackage your meds into smaller vials, you’re not just making life easier-you’re changing the medicine itself. The container your drug came in wasn’t chosen by accident. It was designed to protect it from light, moisture, air, and temperature shifts. Once you move it out of that original packaging, everything changes. And that’s where things get dangerous if you don’t know what to look for.
Why Original Packaging Matters
Your prescription bottle isn’t just a container. It’s part of the medicine. Manufacturer packaging uses special materials like high-density polyethylene (HDPE) with built-in desiccants to keep moisture out. Some bottles have child-resistant caps with sealed liners. Others are amber-colored to block UV light. These features aren’t optional-they’re science-backed protections.Take albuterol sulfate tablets. In their original HDPE bottle with a desiccant, they lose less than 3% of potency after 90 days. But when repackaged into a standard pharmacy vial without a desiccant? That number jumps to over 15%. That’s not a small difference. That’s enough to make a rescue inhaler less effective during an asthma attack.
The FDA makes this clear: if the drug leaves its original container, the manufacturer’s expiration date no longer applies. That’s not a suggestion. It’s a regulation. Yet, a 2020 survey by the Institute for Safe Medication Practices found that 32% of community pharmacies had no formal process to determine expiration dates for repackaged meds. That’s not negligence-it’s a systemic blind spot.
What Degradation Looks Like
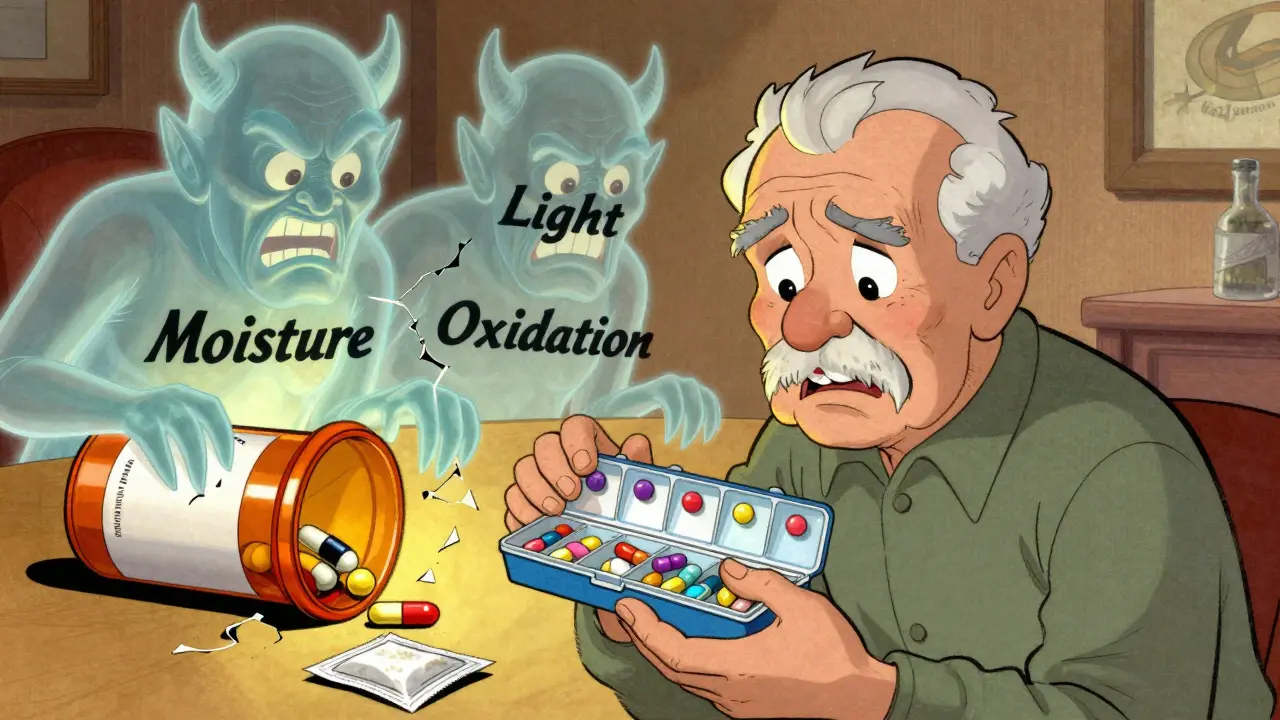
Medications don’t just expire on a calendar. They break down. And how they break down depends on their chemistry and their new environment.Moisture is the biggest enemy for most solid oral medications. Drugs like amoxicillin, levothyroxine, and metformin are hygroscopic-they suck water out of the air. Once they absorb moisture, they can clump, discolor, or chemically degrade. A tablet that looks fine might have lost 20% of its active ingredient without any visible signs.
Light-sensitive drugs like nifedipine, nitroglycerin, or riboflavin can break down within days if exposed to sunlight or fluorescent lighting. You won’t see it. You won’t smell it. But your blood pressure or energy levels might feel the effect.
Then there’s oxidation. Drugs with iron, sulfur, or unsaturated bonds-like some statins or beta-blockers-can react with oxygen. This creates new compounds that may be inactive… or toxic. High-performance liquid chromatography (HPLC) is the only way to detect these changes at low levels, but most pharmacies don’t have that equipment.
Physical changes matter too. If your pills stick together in the pillbox, if the coating cracks, or if the color shifts from white to yellow or brown-stop using them. These aren’t just cosmetic issues. They’re warning signs.
Pillboxes Are a Different Risk
Pillboxes aren’t just repackaged meds-they’re mixed bags. You’re putting ten different drugs from ten different manufacturers into one plastic tray. And that creates problems no one tested.A 2022 study from the American Pharmacists Association found that 18.7% of pillbox combinations showed physical interactions within two weeks. One patient’s pillbox had metoprolol and lisinopril stacked together. The moisture from the lisinopril tablet caused the metoprolol to soften and stick. Another had levothyroxine next to a calcium supplement-resulting in a chalky residue that coated the tablet. Neither looked broken. Both were less effective.
There’s also the risk of contamination. A pillbox used for antibiotics one week might hold blood thinners the next. Even with cleaning, residue builds up. And if someone drops a pill in the tray and pushes it back in? That’s a cross-contamination hazard.
And don’t assume your pillbox is sterile. Most are plastic trays bought at a drugstore. They’re not medical-grade. They’re not sealed. They’re not tested for chemical leaching. They’re convenient. That’s it.

How to Actually Test Stability
You don’t need a lab to start evaluating stability-but you do need a system.Start with this simple checklist:
- Check the original packaging. Did it have a desiccant? Was it in an amber bottle? Write it down.
- Use the right container. For moisture-sensitive drugs, use vials with desiccant packs. For light-sensitive drugs, use amber glass or opaque containers. Avoid clear plastic.
- Store properly. Keep repackaged meds in a cool, dry place-not the bathroom, not the kitchen counter, not the car. A bedroom drawer is better than most.
- Label with a new expiration date. Don’t use the manufacturer’s date. Use a date based on the drug’s known stability.
Here’s what experts recommend for common drugs:
- Amoxicillin - 30 days max in non-original packaging
- Nifedipine - 60 days, must be in amber container
- Atenolol - 90 days, stable if kept dry
- Levothyroxine - 30 days, extremely moisture-sensitive
- Metformin - 60 days, prone to clumping
These aren’t guesses. They’re based on real stability data from the Parenteral Drug Association and the University of Florida’s Web-based Stability Database, which now tracks over 1,800 repackaged medication scenarios.
What Pharmacies Should Be Doing
Hospitals and large chains often have stability protocols. Independent pharmacies? Not so much. A 2023 survey showed only 28% of independent pharmacies have access to HPLC testing. That means most are guessing.The ASHP recommends a tiered approach:
- High-risk drugs (warfarin, digoxin, chemotherapy, insulin): Must be tested with HPLC before repackaging. No exceptions.
- Medium-risk drugs (blood pressure meds, antidepressants): Use bracketing-group drugs with similar chemical properties and test one representative. If it holds, the others likely will too.
- Low-risk drugs (vitamins, fiber supplements): Can use manufacturer’s expiration date if stored properly, but still need a repackaging date.
And desiccants? They’re not optional. A multicenter trial with over 8,400 repackaged units showed that adding a desiccant pack extended stability by 47%. For a $0.10 item, that’s a massive safety win.
What You Can Do Right Now
You don’t have to wait for your pharmacy to get it right. Here’s what you can do today:- Ask your pharmacist: “What’s the expiration date you’re assigning to this repackaged medication?” If they say “the same as the bottle,” walk out.
- Check your pillbox every week. Look for color changes, stickiness, powdering, or odd smells.
- Store your pillbox away from heat and humidity. Don’t leave it on the sink.
- Replace your pillbox every 30 days-even if it looks clean.
- If you’re unsure, throw it out. A few dollars on a new prescription is cheaper than an ER visit.
There’s no magic formula. No app that scans your pills and tells you if they’re still good. Stability isn’t about dates on a label. It’s about conditions, chemistry, and care.
What’s Changing in 2026
The rules are tightening. The USP is finalizing General Chapter <1790> in late 2024, which will require pharmacies to test at least three timepoints for any repackaged drug with a shelf life under 90 days. The FDA’s new draft guidance demands container integrity testing using vacuum decay methods with 5-micron sensitivity. And starting in 2024, PCAB-accredited pharmacies must complete 8 hours of stability training every year.These aren’t bureaucratic hoops. They’re responses to real harm. In 2023, the FDA shut down a major pharmacy chain for failing to assign proper expiration dates. Lab tests showed 22% of their repackaged meds degraded beyond safe limits. That’s not a rare outlier. That’s the norm in unregulated settings.
For now, the gap between regulation and reality is wide. But you don’t have to wait for the system to catch up. You can protect yourself-by asking questions, watching your meds, and refusing to assume that just because it looks the same, it still works the same.
Can I use the manufacturer’s expiration date on repackaged pills?
No. The manufacturer’s expiration date only applies if the drug stays in its original container with the original closure system and desiccant. Once you transfer it-even into a pharmacy vial-that date is no longer valid. The FDA explicitly states this in its compliance guidance. Using the original date on repackaged meds is a violation of federal standards and puts patients at risk.
How do I know if my pill has degraded?
Look for changes in color, texture, or smell. White pills turning yellow or brown, tablets cracking or crumbling, powdery residue inside the container, or a strange odor are all red flags. Some drugs, like levothyroxine or amoxicillin, may not show visible changes even when they’ve lost potency. If you’re unsure, don’t take it. A simple test: if it doesn’t look exactly like it did when you got it, assume it’s no longer safe.
Are pillboxes safe for long-term use?
Pillboxes are convenient but not designed for long-term storage. Most are made of low-grade plastic that doesn’t protect against moisture or light. They also allow cross-contamination between drugs. Experts recommend replacing pillboxes every 30 days and using them only for short-term use-like a week or two. For ongoing medication management, ask your pharmacy about blister packs or unit-dose packaging, which are sealed and labeled with expiration dates.
What should I do if my pharmacy won’t give me a repackaging expiration date?
Ask for the pharmacy’s written policy on repackaged medication stability. If they can’t provide one, request that your meds stay in their original containers. If they refuse, switch pharmacies. You have the right to know how long your medication is safe to take. If they’re not tracking it, they’re not following best practices. Your health isn’t worth the risk.
Do desiccant packs really help?
Yes. A 2023 trial involving over 8,400 repackaged medication units showed that adding a desiccant pack extended stability by 47%. For moisture-sensitive drugs like levothyroxine or metformin, this can mean the difference between a safe dose and a failed treatment. Always ask your pharmacist to include a desiccant in repackaged containers. If they say it’s not standard, insist. It’s a low-cost, high-impact safety step.
If you take multiple medications, your pillbox isn’t just a convenience-it’s a potential risk. Treat it like the medical device it is. Don’t wait for a disaster to realize you should’ve asked more questions. Your body doesn’t know the difference between a pill that’s expired and one that’s degraded. It just knows whether it works-or doesn’t.



Comments
Man, I never thought about how much the bottle itself is part of the drug. I’ve been dumping my levothyroxine into a pillbox for months like it’s cereal. Now I’m sweating. That 15% potency drop? That’s like taking half a dose every time. I’m switching to amber vials with desiccants tomorrow.
Let’s be real - this isn’t about science, it’s about profit. Pharmacies repack because it’s cheaper than labeling, testing, or training staff. The FDA doesn’t enforce this because they’re too busy chasing vape pens. You think they care if your blood pressure med turns to dust? Nah. They care about lawsuits. So you’re on your own. And if you’re lucky, you’ll notice the side effects before your heart gives out.
i never knew pills could get sad from moisture 😅 i just thought they expired on the date. now i check my pillbox every morning like its a plant that needs watering. levothyroxine is my baby now. no more bathroom counter. drawer only. even if its weird to talk to my meds
so like... if my metformin looks kinda dusty but still white and hard... im fine right? i mean it dont smell like death or anything. i got a whole week left on this bottle and i aint got time for pharmacy drama
from india we use so many repackaged meds because original bottles are too expensive. we put pills in small ziplock bags. sometimes with a piece of tissue as desiccant. its not perfect but its all we got. i hope one day we have better systems. thank you for sharing this. i will try to get amber vials next time
OMG this is so important 😱 I just realized I’ve been storing my nifedipine next to my coffee maker. The light + heat + steam… I’m literally poisoning myself. Switching to a locked drawer tonight. Also buying amber vials. This post just saved my life 🙏
why are we even talking about this like its some big secret. every pharmacy does this. its a scam. they know the pills degrade. they just dont tell you because they make more money selling you new ones every month. the system is rigged. your meds are not safe. stop trusting anyone. buy your own desiccants. hide your pills. trust no one
Did you know that some pillboxes are made with phthalates? Those chemicals leach into meds over time. And no one tests for it. Not the FDA. Not the pharmacy. Not even the manufacturer. This isn’t just about potency - it’s about endocrine disruption. Your thyroid isn’t the only thing being sabotaged. Your hormones are slowly turning to sludge. And you’re the one holding the plastic tray.
While the technical and regulatory details presented here are both compelling and well-documented, I would like to emphasize the broader ethical imperative: patient autonomy requires transparency. When a medication’s stability is compromised by repackaging, the onus is on the provider to disclose this - not on the patient to discover it through anecdotal observation or internet research. This is not merely a pharmacological issue - it is a fiduciary one. We owe our patients more than convenience. We owe them truth.
so you’re telling me my $2 pillbox from walgreens is basically a chemical death trap? and the pharmacist just shrugs and says ‘eh, it’s fine’? wow. i feel so safe. guess i’ll start carrying my meds in a lead-lined briefcase like a spy. next thing you know they’ll say coffee stains on pills are ‘part of the flavor profile’
lol the FDA is gonna make pharmacies test everything? sure. next they’ll require every pill to have a QR code that plays a lullaby when you open it. meanwhile my neighbor takes his blood pressure meds out of a cereal box and says ‘if it fits, it ships’. this whole thing is a distraction. the real problem? people don’t take their meds at all. who cares if it’s 95% or 85% potent if you’re not even swallowing it?