Many older adults take five or more medications every day. Some of these drugs were prescribed years ago for conditions that have changed-or even disappeared. Yet they’re still on the list. This isn’t rare. It’s common. And it’s risky. Taking too many medications can lead to dizziness, confusion, falls, kidney damage, and hospital visits. The good news? You don’t have to keep taking them all. You can talk to your doctor about cutting back. But it’s not as simple as saying, ‘I want fewer pills.’ You need to talk the right way.
Why Deprescribing Matters
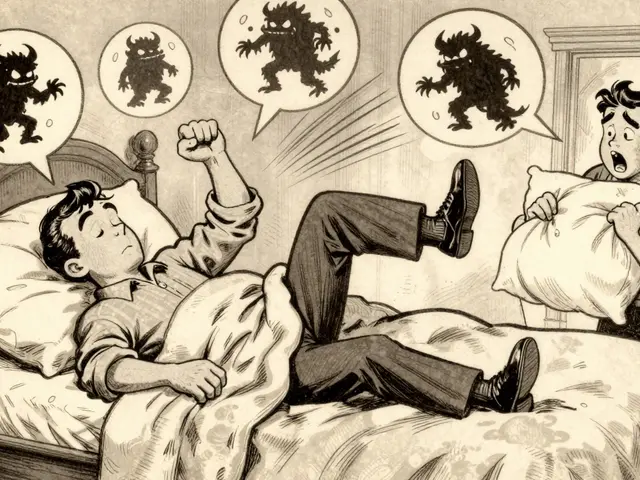
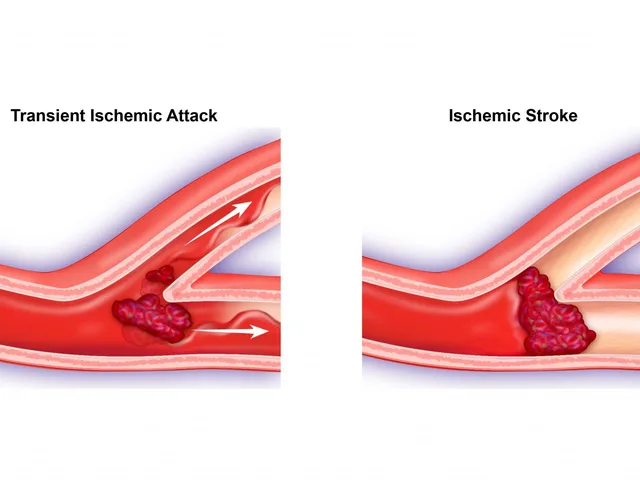
Deprescribing isn’t about stopping medicine because it’s cheap or inconvenient. It’s about making sure every pill you take still does more good than harm. For seniors, especially those with multiple chronic conditions, some drugs stop being helpful over time. A blood pressure pill that kept your numbers in check at 70 might now be pushing you too low at 85. A sleep aid that helped you rest at 70 might be fogging your brain at 80. A statin that lowered cholesterol after a heart attack might not be needed anymore if your risk has dropped.Studies show that 15% of seniors on five or more medications experience serious side effects each year. Many of those side effects are preventable. The goal of deprescribing is simple: keep what helps, remove what doesn’t. And it’s not just about safety-it’s about quality of life. Do you want to feel alert enough to walk your grandkids to school? To garden without getting dizzy? To sleep through the night without taking three different pills? Those are the goals that matter.
What Most People Get Wrong
A lot of patients go into their doctor’s office and say, ‘I think I’m on too many meds.’ That sounds reasonable. But it rarely works. Why? Because it’s vague. It doesn’t connect to anything real in their life. Doctors hear that all the time. And when they hear it, they often think, ‘They’re just complaining.’ Or worse-they assume it’s about cost, not care.One study found that only 23% of patients who asked for fewer pills got any changes. But when patients linked their request to a specific goal-like ‘I want to stop feeling dizzy when I stand up so I can keep walking in the park’-the success rate jumped to 74%. That’s not a coincidence. It’s how communication works. Doctors respond to clarity. They respond to personal stakes. They respond to evidence-not just feelings.
Another mistake? Waiting for the doctor to bring it up. Research shows that 68% of seniors would like to take fewer medications-but only 12% ever hear their doctor suggest it. That means the ball is in your court. You have to start the conversation. And you have to do it right.
How to Prepare Before Your Appointment
You wouldn’t walk into a car repair shop without knowing what’s wrong with your engine. Don’t walk into your doctor’s office without knowing what’s in your medicine cabinet.Here’s exactly what to do before your visit:
- Write down every medication you take. This includes prescriptions, over-the-counter pills, vitamins, supplements, and herbal remedies. Don’t skip anything. Many people forget their daily aspirin or their magnesium pill. That’s often the one causing problems.
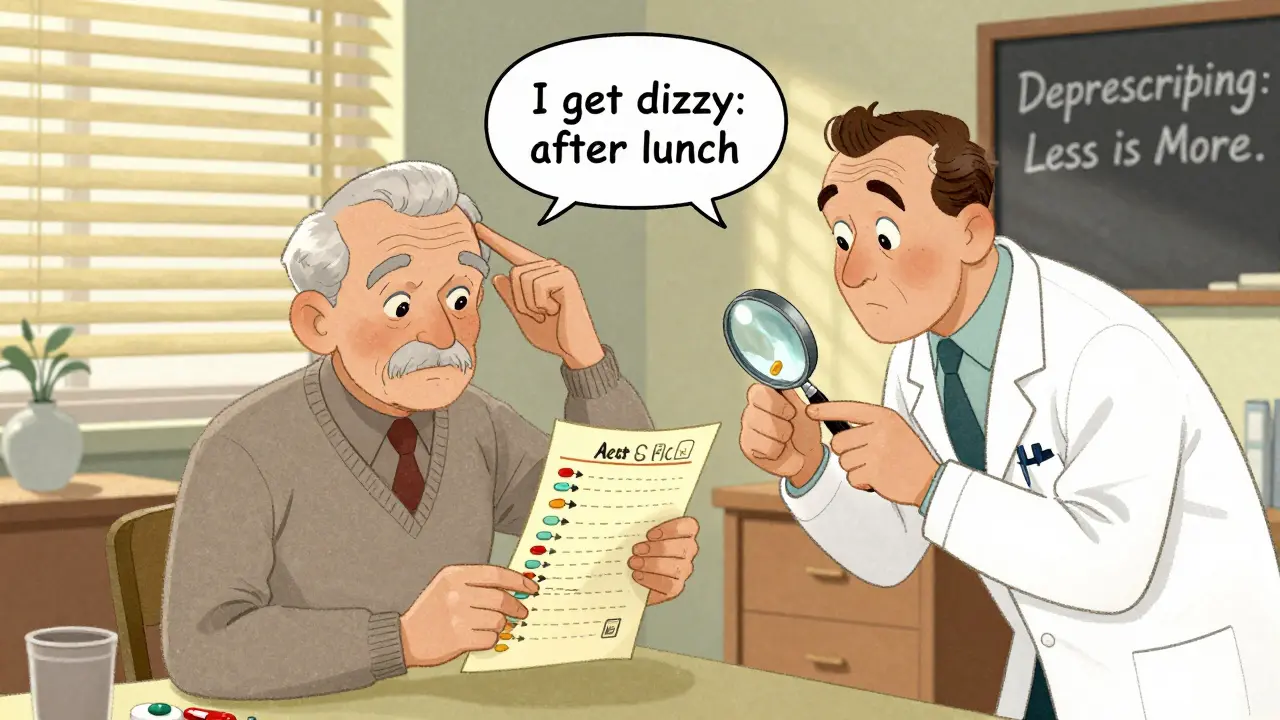
- Track side effects. Don’t say ‘I feel tired.’ Say: ‘I get dizzy two hours after taking my blood pressure pill, and I’ve nearly fallen three times this month.’ Include timing, frequency, and what you couldn’t do because of it.
- Choose 1-2 meds to focus on. Pick the ones you suspect are causing trouble. Maybe it’s the sleeping pill that leaves you groggy all day. Or the painkiller that makes you nauseous. Don’t try to tackle everything at once. Start small.
- Write down your goal. What do you want to be able to do? Walk without fear? Play with your grandkids? Sleep through the night? Make it specific. ‘I want to stop feeling like I’m walking through fog’ is better than ‘I want fewer pills.’
- Bring printed info. Print out the Canadian Deprescribing Guidelines for the specific class of medication you’re concerned about. For example, if you’re on a benzodiazepine for sleep, look up the section on sedative-hypnotics. It shows evidence for safe tapering. Doctors respect this. It shows you’ve done your homework.
People who do this are 37% more likely to have at least one medication reduced. That’s not luck. It’s preparation.

What to Say During the Appointment
The way you frame your request makes all the difference. Don’t lead with ‘Can I stop this?’ Lead with ‘I’m worried this might be hurting me.’Use this simple structure: Ask - Tell - Ask
- Ask: ‘What’s your view on how my medications are working for me right now?’
- Tell: ‘I’ve noticed that since I started taking [medication name], I’ve been getting dizzy after lunch. I’ve had two near-falls this month. I really want to keep walking in the park with my grandkids, but I’m scared I’ll fall. I’m wondering if this medicine might be making that worse.’
- Ask: ‘Could we try reducing the dose slowly to see if my balance improves? What would a safe plan look like?’
This approach works because it’s not confrontational. It’s collaborative. You’re not telling your doctor what to do. You’re inviting them to help you solve a problem you both care about.
Studies show that phrases like ‘This medicine may be hurting you more than helping you’ are 78% more effective than talking about cost or life expectancy. And phrases that include a personal goal-like ‘I want to be able to walk to the mailbox without help’-are 89% more likely to lead to action.
Don’t say: ‘I just want to take fewer pills.’
Do say: ‘I want to feel steady on my feet so I can keep doing the things I love.’
What to Expect After the Conversation
Deprescribing doesn’t happen overnight. Almost 86% of successful cases involve gradual reduction-not sudden stops. Your doctor will likely suggest a slow taper. Maybe reducing your dose by 25% every month. Or switching to a lower-strength pill. They might ask you to keep a symptom diary for a few weeks to track how you feel.Be ready for questions like:
- ‘What happens if your blood pressure goes up again?’
- ‘What if your pain comes back?’
- ‘Are you sure you want to do this?’
These aren’t doubts. They’re safeguards. Your doctor isn’t trying to talk you out of it-they’re making sure you’re safe. Answer them with your goal: ‘I’m okay with a little more pain if it means I’m not dizzy all day. I can manage the pain with walking and heat packs.’
Ask for a follow-up plan. Say: ‘Can we schedule a check-in in six weeks to see how I’m doing?’ Most doctors will agree if you ask.
What If They Say No?
Sometimes, your doctor will say no. Maybe they’re worried about rebound symptoms. Maybe they’re not trained in deprescribing. That’s okay. It doesn’t mean you’re wrong.Ask: ‘Is there a specialist who could help me review my medications?’
Ask: ‘Could I get a referral to a geriatric pharmacist?’
Many hospitals and clinics now have geriatric pharmacists who specialize in medication reviews. They work with doctors to find safer regimens. In Australia, these services are often covered by Medicare under the Chronic Disease Management plan.
If your doctor dismisses you, don’t give up. Find another. There are doctors who specialize in senior care and deprescribing. They know this stuff inside and out.
What’s Changed in 2026
The system is starting to catch up. Since 2023, Medicare’s Annual Wellness Visit now includes a required medication review. Electronic health records now flag potentially risky medications for seniors automatically. The CDC’s ‘Right Size My Meds’ campaign has reached over 12 million seniors. And more doctors are getting trained.But the biggest change? Patients are starting to lead the conversation. And that’s what makes the difference.
One woman in Perth, 78, brought her doctor a journal showing how each pill affected her balance. She cut three medications over six months. Now she walks three miles a week. Another man stopped his sleeping pill and his muscle relaxant. His memory cleared up. He started reading to his grandchildren again.
It’s not magic. It’s communication.
Final Thought: You’re Not Asking for Less Care. You’re Asking for Better Care.
Some people worry that reducing medications means their doctor doesn’t care anymore. That’s a myth. Taking fewer pills isn’t giving up. It’s choosing quality over quantity. It’s choosing clarity over confusion. It’s choosing life over side effects.You’ve lived long enough to know what matters. Now it’s time to make sure your medicine supports that-not fights against it.


Comments
I took 12 pills a day for 8 years. One day I just said ‘enough.’ Now I walk 5 miles, cook for my grandkids, and don’t need an alarm to remember which pill does what. 🙌💊 #DeprescribingIsLiving
OMG YES. My mom stopped her benzos and now she remembers my birthday. Like, actually remembers. We cried. Then we ate tacos. 🌮❤️ You don’t need more meds-you need more LIFE.
I tried this. Doctor said no. I went to a geriatric pharmacist. Cut two meds. No more dizziness. Now I garden. That’s it.
This is the most practical guide I’ve seen. The Ask-Tell-Ask framework is gold. I’ve used it with my elderly patients. When they tie it to real-life goals-walking the dog, playing with grandkids-it clicks. Doctors respond to specificity. Not complaints. Evidence. Preparation. It’s not magic. It’s medicine.
The pharmacokinetic profiles of polypharmacy in geriatric populations are non-linear and often exhibit inverted U-shaped dose-response curves, particularly with CNS-depressant agents. The risk-benefit calculus must be recalibrated via longitudinal CYP450 phenotyping and functional status metrics.
The act of deprescribing is not merely a clinical intervention-it’s a metaphysical reclamation of agency in a system that commodifies pharmaceutical dependency. We are not patients. We are sentient beings entangled in a pharmacological hegemony. 🌌💊 #ExistentialTaper
i cant belive people still take so many pills... my aunt died from a drug interaction and people still dont get it?? its not just about being old its about being lazy and letting doctors run your life. i dont even take tylenol anymore. i drink ginger tea. and i live. #wakeupeveryone
This is why we’re in a healthcare crisis. You can’t just ‘cut meds’ because you’re tired. What if you have a silent arrhythmia? What if your BP drops and you stroke out? This isn’t wellness influencer advice. It’s dangerous. I’ve seen people die because they listened to Reddit.
You think your doctor cares? They’re paid to prescribe. They get bonuses for hitting cholesterol targets. They don’t want you off meds. They want you on more. This whole post is a scam. I’ve been in the system. I know how it works. Don’t trust anyone who says ‘talk to your doctor.’ They’re part of the machine.