When you start taking a blood thinner-whether it’s for a blood clot, atrial fibrillation, or another condition-you’re told to watch for signs of bleeding: bruising, nosebleeds, or cuts that won’t stop. But one of the most common and disruptive side effects? Heavy menstrual bleeding. And most women aren’t warned about it.
Here’s the reality: if you’re a woman of reproductive age on a blood thinner, there’s a 70% chance your periods will get dramatically heavier. That’s not a rare side effect-it’s the norm. And yet, a 2023 survey found that 68% of women said their hematologist never asked about their periods after starting anticoagulants. That’s a gap in care that’s leaving women stuck with soaked pads, missed workdays, and constant anxiety about leaks.
Why Blood Thinners Make Periods So Heavy
Blood thinners-also called anticoagulants-work by slowing down your body’s ability to form clots. That’s great for preventing strokes or pulmonary embolisms. But when it comes to your uterus, that same mechanism means the lining doesn’t clot and shed neatly. Instead, it bleeds out slowly over days, sometimes hours. The result? Periods that last longer than seven days, needing a pad or tampon change every 30 minutes, or even leaking through clothes.
It’s not just about discomfort. This kind of bleeding can lead to iron deficiency anemia-fatigue, dizziness, heart palpitations. A 2020 study found that nearly half of women on anticoagulants with heavy bleeding developed low iron levels. And because many women assume heavy periods are just "normal," they wait months-or years-before saying anything to a doctor.
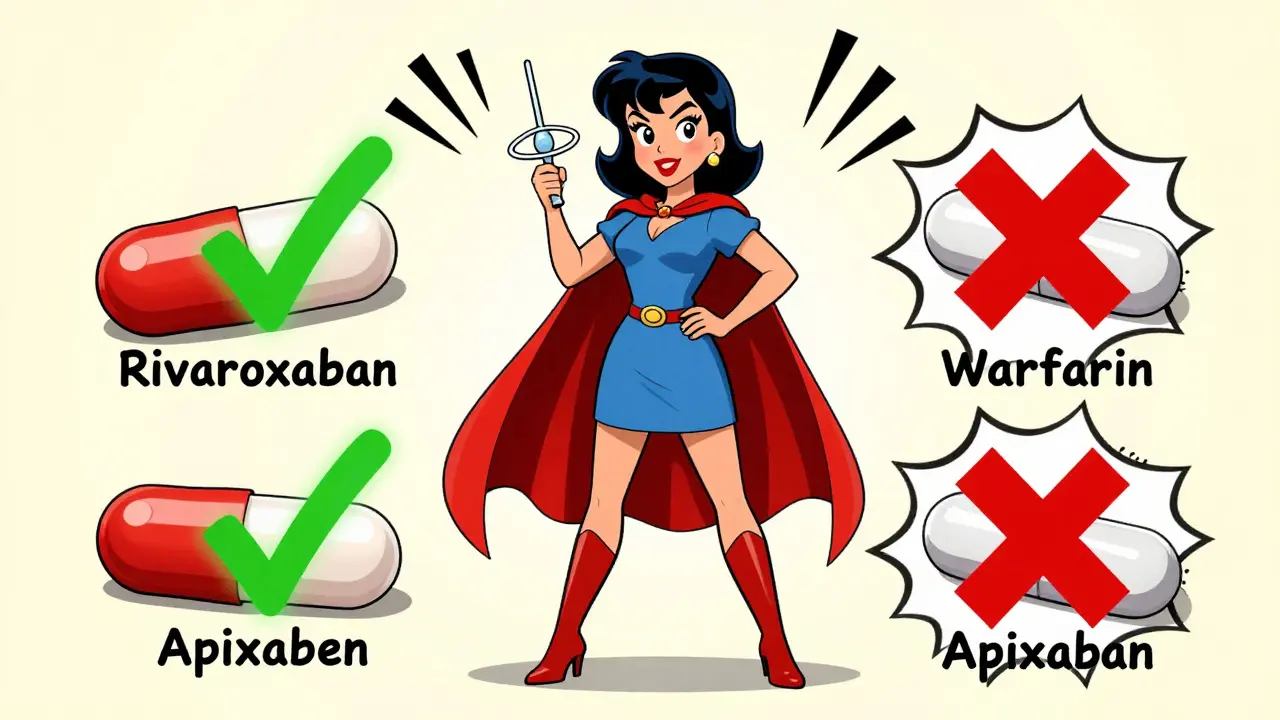
Not All Blood Thinners Are Equal
Not every blood thinner carries the same risk. Research from Blood Advances and the American Society of Hematology shows that your choice of medication matters a lot.
- Rivaroxaban has the highest association with heavy menstrual bleeding.
- Apixaban and dabigatran are linked to significantly lower rates of HMB.
- Warfarin (the older blood thinner) also causes heavy bleeding, but the risk is similar to rivaroxaban.
That means if you’re newly prescribed a blood thinner and you’re concerned about your periods, asking your doctor about switching to apixaban or dabigatran might be the first step-not waiting until you’re exhausted from bleeding all day.
What Actually Helps: Proven Treatment Options
The good news? You don’t have to suffer. There are several effective, safe ways to manage heavy bleeding-without stopping your blood thinner. In fact, stopping or skipping doses can increase your risk of a life-threatening clot by five times.
1. Levonorgestrel IUD (Mirena, Kyleena, etc.)
This is the most effective option for most women. A small T-shaped device inserted into the uterus releases a steady dose of progesterone directly into the uterine lining. Within three months, most women see a 70-90% drop in bleeding. Some stop getting periods altogether.
Studies show it works just as well whether you’re on apixaban, rivaroxaban, or warfarin. And because it’s local-no systemic hormones-it doesn’t interfere with your anticoagulant. One woman in the r/anticoag Reddit community said: "After the Mirena, my periods went from ER visits to nearly gone. I didn’t have to change my blood thinner."
2. Progestin-Only Pills (Norethisterone)
If you don’t want an IUD, high-dose progestin pills are a solid alternative. The American Society of Hematology recommends norethisterone 5 mg three times a day for 21 days during your period. It thickens the uterine lining and reduces flow by up to 60%.
It’s not a daily long-term fix like the IUD, but it’s safe to use alongside anticoagulants and can be repeated each cycle.
3. Tranexamic Acid
This is a non-hormonal pill taken only during your period-usually 1-2 tablets every 8 hours for up to 5 days. It helps your blood clot at the site of bleeding without affecting your overall clotting system.
Clinical trials show it cuts menstrual blood loss by 30-50%. It’s FDA-approved for heavy periods and works well with blood thinners. Just don’t take it every day-only when you’re bleeding. And avoid it if you have a history of blood clots.
4. Combined Hormonal Birth Control
Pills, patches, or rings that contain estrogen and progestin can also reduce bleeding. But they’re not always safe for women with a history of clots. If you’re on a blood thinner because of a past clot, your doctor will need to weigh the risks. For some, it’s a viable option. For others, it’s a no-go.
What Doesn’t Work (And Why)
Many women try NSAIDs like ibuprofen or aspirin thinking they’ll help. But here’s the catch: those drugs also thin the blood. Using them with anticoagulants can double your bleeding risk. A 2024 Cleveland Clinic update warns against combining them unless under strict medical supervision.
Endometrial ablation-a procedure that burns off the uterine lining-is often suggested for heavy periods. But if you’re on a blood thinner, it’s risky. Bleeding during or after the procedure can be dangerous. Most experts now consider it a last resort, only if you’re done having children and other treatments have failed.
Iron Deficiency Is Common-Get Checked
Heavy bleeding doesn’t just make life harder-it drains your iron. Symptoms like tiredness, shortness of breath, cold hands, or hair loss are often blamed on stress or lack of sleep. But if you’re on a blood thinner and experiencing these, ask for a ferritin test. Low iron is easy to fix with supplements or IV iron if needed.
The National Blood Clot Alliance recommends all menstruating women on anticoagulants get tested for anemia within six months of starting treatment. Don’t wait for symptoms. Get tested.
What to Ask Your Doctor
Most women don’t bring up heavy periods because they think it’s "just part of being a woman." But it’s not. It’s a medical issue that can be fixed.
Here’s what to say at your next appointment:
- "I’ve noticed my periods are much heavier since I started my blood thinner. Is this normal?"
- "Could my current blood thinner be making this worse? Are there alternatives?"
- "What are my options for reducing the bleeding without stopping my anticoagulant?"
- "Can you check my iron levels?"
- "Should I see a gynecologist who’s familiar with anticoagulated patients?"
Doctors aren’t always trained to ask about periods. But you are the expert on your body. If your hematologist doesn’t know the answer, ask for a referral to a gynecologist who specializes in bleeding disorders.
Real-Life Impact: More Than Just "Inconvenient"
Women on Reddit and in support groups describe:
- Carrying emergency changes in their purse, car, and work bag.
- Missing 3-5 days of work per month.
- Avoiding dates, travel, or social events because they’re afraid of leaking.
- Feeling like their body is betraying them.
This isn’t just a physical issue-it’s a mental one. Anxiety, shame, and isolation are common. And yet, treatment exists. And it works.
The Future: Better Guidelines Are Coming
In 2021, the International Society on Thrombosis and Haemostasis added menstrual bleeding to its official bleeding assessment tools. In 2024, ACOG updated its guidelines to include specific recommendations for anticoagulant-related HMB. And by mid-2025, the American Society of Hematology and ACOG plan to release joint guidelines-finally standardizing care.
But you don’t have to wait. Right now, you have options. You don’t have to accept heavy bleeding as your new normal. You don’t have to choose between preventing a clot and living your life.
Can I stop my blood thinner if my periods are too heavy?
No. Stopping or skipping doses of your blood thinner increases your risk of a life-threatening clot by up to five times. Never stop your medication without talking to your doctor. Instead, focus on treatments that reduce bleeding while keeping you protected-like the levonorgestrel IUD, progestin pills, or tranexamic acid.
Will the levonorgestrel IUD interfere with my blood thinner?
No. The levonorgestrel IUD releases hormones directly into the uterus, so very little enters your bloodstream. It doesn’t affect how your blood thinner works, and studies confirm it’s safe to use with all types of anticoagulants-including apixaban, rivaroxaban, and warfarin. Many women see a 70-90% drop in bleeding within three months.
Is tranexamic acid safe with blood thinners?
Yes, when used correctly. Tranexamic acid is taken only during your period-usually for up to five days-and helps your blood clot locally in the uterus. It doesn’t increase your overall clotting risk. Clinical trials show it reduces bleeding by 30-50% without interfering with anticoagulants. Just avoid it if you have a history of deep vein thrombosis or stroke.
Why don’t doctors ask about heavy periods?
Most hematologists focus on preventing clots, not managing menstrual bleeding. A 2023 survey found only 22% of hematology clinics routinely ask female patients under 50 about their periods. It’s a gap in training, not in need. If your doctor doesn’t bring it up, speak up. Heavy bleeding is a treatable side effect-not something you have to live with.
Can I use ibuprofen or aspirin to reduce bleeding?
Not without caution. NSAIDs like ibuprofen and aspirin also thin the blood. Using them with anticoagulants can increase your risk of bleeding, sometimes dangerously. While some women see a 20-40% reduction in flow, the added risk usually outweighs the benefit. Talk to your doctor before combining them.
What if I want to have children in the future?
The levonorgestrel IUD and progestin pills are fully reversible. Once removed, your fertility returns to normal. Tranexamic acid is taken only during your period and has no long-term effect on fertility. Endometrial ablation is not recommended if you plan to have children, as it can damage the uterine lining. All other treatments are safe for future pregnancy-just make sure your doctor knows your plans.




Comments
I started apixaban last year and my periods went from hellish to barely there after the Mirena. Seriously, it changed everything. I used to dread my cycle-leaking through clothes, panic-checking my bag every hour. Now? I forget I’m even on it. No more ER trips, no more anxiety. Just… peace.
Also, please tell your doctor to ask about periods. My hematologist never did. I had to bring it up myself. It’s not weird. It’s medical.
Wow. This is… a lot. Like, I appreciate the effort, but this reads like a textbook appendix. Did you copy-paste a journal article and call it a day? Honestly? Most people just want to know: what works? Not the 17-step clinical trial breakdown.
Also, tranexamic acid? I tried it. Didn’t work. And now I’m stuck with a $1,200 IUD because my insurance refused to cover the pill. So… thanks for the info, but real life is messier.
Thank you for writing this. I’ve been on warfarin for 5 years, and no one ever mentioned this side effect. I thought I was just ‘bad at periods.’ Turns out, I was just unlucky-and unheard.
I got the Kyleena last year. Three months later, I cried in the shower because I didn’t have to change a pad. That’s not an exaggeration. That’s real life.
You’re not alone. And you’re not broken. There’s help. Keep pushing.
Every human body is a universe of silent suffering, and yet we act as if bleeding is just ‘women’s stuff.’
When we reduce medical care to ‘clot prevention’ and ignore the visceral, daily reality of menstruation, we are not healing-we are erasing.
That 68% of women never asked about their periods? That’s not negligence. That’s systemic gendered blindness. The IUD, tranexamic acid, progestin-all of it is evidence. But evidence doesn’t change policy unless we scream loud enough.
So scream. Bring your pads. Bring your charts. Bring your rage. And don’t let them tell you it’s normal.
🫶
Let me tell you something about American healthcare. You think this is about bleeding? No. It’s about profit. Mirena? $1,200. Tranexamic acid? $40 a month. But insurance won’t cover it unless you’re ‘severely anemic’-which means you’re nearly unconscious before they’ll help.
And don’t get me started on doctors who think ‘just take ibuprofen’ is a solution. Ibuprofen is a blood thinner too! Do they even read the damn pharmacology textbooks?
Women in India don’t have this problem. We just… suffer. Quietly. Because we don’t have the luxury of ‘asking our doctor.’ So don’t act like this is some new revelation. It’s been happening for centuries. You’re just finally noticing.
And yes, I’m angry. You should be too.
Oh wow. Another ‘I’m a woman and I bleed’ post. How original.
Let me guess-you’re also mad that your period is heavier than your bank account? Newsflash: anticoagulants are life-saving. If you can’t handle a little extra flow, maybe you shouldn’t be on them in the first place.
Also, ‘levonorgestrel IUD’? That’s just a fancy word for ‘hormone implant.’ I’m surprised you didn’t mention yoga and crystal healing as ‘proven treatments.’
Grow up. Medicine isn’t a Pinterest board.
Just wanted to add: if you’re on rivaroxaban and your periods are brutal, switching to apixaban isn’t just an option-it’s a game-changer. My hematologist dismissed it at first. I came back with three studies. He switched me. Two months later, I was back to normal.
Also, tranexamic acid works better if you start it the *second* day of bleeding, not the first. And take it with food. My stomach hated it otherwise.
And yes, ferritin. Get it checked. Even if your hemoglobin’s fine. Iron stores are the silent killer here.
Ugh. More woke medical advice. Next you’ll tell me we need gender-neutral bathrooms for clotting disorders.
Look. I’m on warfarin. I’ve had two clots. I don’t care if your period’s heavy. You take the medicine. Period. (Pun intended.)
If you can’t handle it, maybe you shouldn’t be a woman. Just sayin’.