Pancreatitis Risk Calculator for GLP-1 Agonists
This calculator estimates your relative risk of pancreatitis while taking GLP-1 agonist medications (such as Ozempic or Wegovy) based on key health factors identified in medical research. Your risk is calculated relative to the general population taking these medications.
Note: Absolute risk remains low (0.1% to 0.4% lifetime risk). This tool helps identify who may benefit from closer monitoring.
When you start taking a GLP-1 agonist like Ozempic or Wegovy for diabetes or weight loss, you’re not just chasing better numbers on the scale or blood sugar chart. You’re making a decision that affects your whole body - including your pancreas. And while these drugs have transformed how we treat obesity and type 2 diabetes, there’s one concern that keeps popping up in doctor’s offices and online forums: pancreatitis.
What Exactly Are GLP-1 Agonists?
GLP-1 agonists are synthetic versions of a natural hormone your body makes after eating. This hormone, called glucagon-like peptide-1, tells your pancreas to release insulin when blood sugar rises. It also slows down how fast your stomach empties, so you feel full longer. That’s why people lose weight on these drugs - they eat less because they’re not hungry as often.
First approved in 2005, drugs like exenatide (Byetta), liraglutide (Victoza, Saxenda), semaglutide (Ozempic, Wegovy), and tirzepatide (Mounjaro, Zepbound) have become some of the most prescribed medications in the U.S. By late 2024, nearly 40% of all diabetes prescriptions were for GLP-1 agonists. In 2023 alone, semaglutide generated nearly $20 billion in global sales. But with that rise in use came a rise in questions - especially about the pancreas.
Why the Concern About Pancreatitis?
Pancreatitis is inflammation of the pancreas. It can be sudden and painful (acute) or long-lasting (chronic). Symptoms include severe upper belly pain that radiates to your back, nausea, vomiting, and fever. It’s not rare - about 1 in 1,000 people with type 2 diabetes will develop it each year, even without any medication.
Since 2007, the FDA has required a warning on GLP-1 agonist labels about pancreatitis risk. The concern came from early case reports and animal studies showing that these drugs might increase pressure in the pancreatic ducts or trigger enzyme activation. But here’s the twist: the science hasn’t been clear since.
The Evidence Is Mixed - And It Matters
In May 2025, a massive study of nearly a million diabetic patients found GLP-1 agonists raised the risk of acute pancreatitis by 34% and chronic pancreatitis by 45% over five years. That sounds alarming. But just a few months earlier, another study of nearly a million people found no increased risk - in fact, the group on GLP-1 drugs had a slightly lower lifetime chance of pancreatitis than those not taking them.
Then there’s the JAMA study from 2023 that compared GLP-1 agonists to bupropion-naltrexone (Contrave). It found a nine-fold higher risk of pancreatitis with GLP-1 drugs. But that study only included about 5,000 people total - too small to be definitive. Meanwhile, a 2024 study of 127 million patients across 15 countries suggested GLP-1 agonists might actually reduce the chance of pancreatitis coming back compared to SGLT2 inhibitors.
So what’s going on? The truth is, we don’t have one clear answer. The data is messy because pancreatitis is often linked to other things: obesity, high triglycerides, alcohol use, smoking, and diabetes itself. When you’re trying to isolate the effect of a drug, those factors muddy the waters.
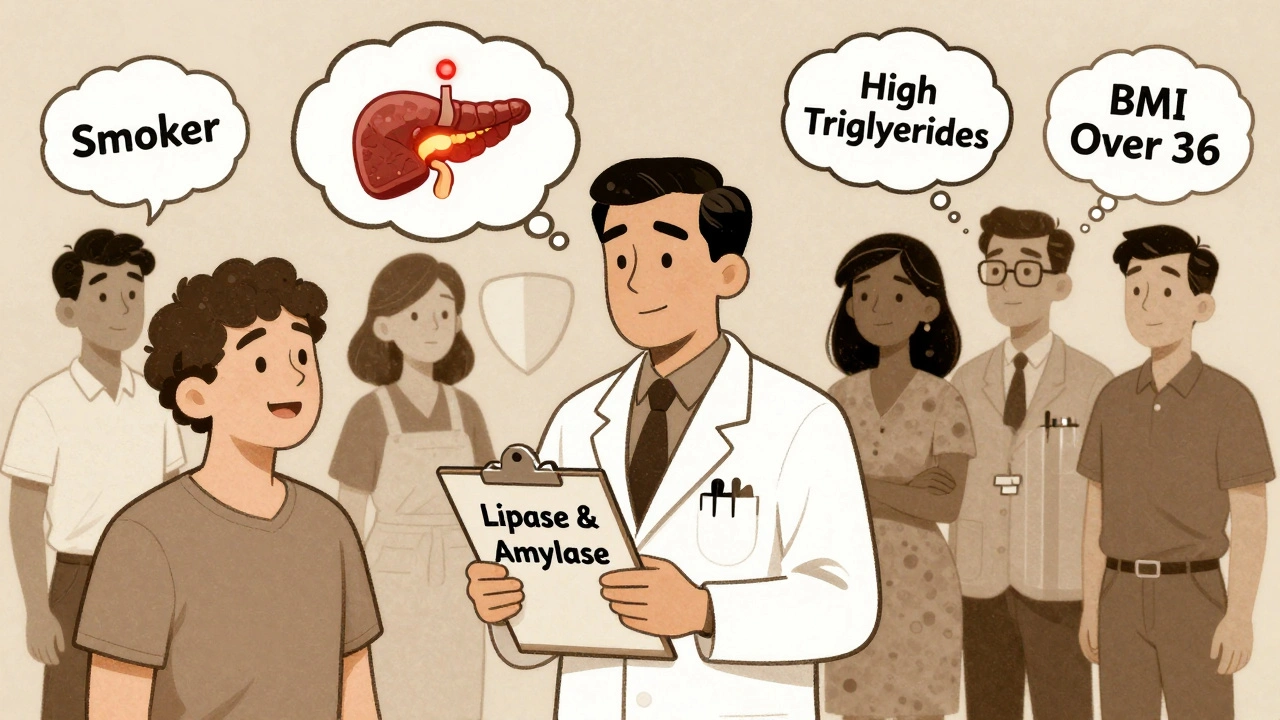
Who’s Really at Risk?
Not everyone needs to worry. Research from the American College of Gastroenterology shows that certain people have a higher chance of developing pancreatitis on these drugs:
- People with a history of high triglycerides (above 500 mg/dL)
- Current or former smokers
- Those with advanced chronic kidney disease
- Patients with a prior history of pancreatitis - but here’s the surprise: newer data says that even if you’ve had it before, starting a GLP-1 agonist doesn’t automatically mean it will come back.
And here’s another counterintuitive finding: people with a BMI over 36 might actually be protected. That’s likely because the drug’s weight-loss effect reduces fat around the pancreas and lowers inflammation overall.
One thing we do know for sure: the absolute risk is still very low. Even in the highest-risk studies, lifetime pancreatitis rates for GLP-1 users range from 0.1% to 0.4%. That’s less than 1 in 250 people.
How to Monitor for Pancreatitis
There’s no need to panic. But you should know the signs and how to respond.
The American Diabetes Association recommends checking blood levels of lipase and amylase - two enzymes released by the pancreas - before you start a GLP-1 agonist if you’ve had pancreatitis before. But many doctors skip this step unless you’re high-risk.
What’s more important is knowing your symptoms:
- Sudden, severe pain in the upper abdomen - often described as a “boring” or “stabbing” feeling
- Pain that spreads to your back
- Nausea or vomiting that doesn’t go away
- Fever or rapid heartbeat
If you feel any of these, stop the medication and call your doctor right away. Don’t wait. Acute pancreatitis can become serious fast.
For high-risk patients (smokers, high triglycerides, kidney disease), doctors often check lipase every 3 months during the first year. For low-risk people, testing is only needed if symptoms appear.
The label for Wegovy (semaglutide) says: “Advise patients to seek medical attention if they experience symptoms of pancreatitis.” That’s not a scare tactic - it’s a practical safety step.
What Are the Alternatives?
If you’re worried about pancreatitis, you have options. But each comes with trade-offs.
SGLT2 Inhibitors (e.g., Jardiance, Farxiga, Invokana)
These drugs make your kidneys flush out extra sugar through urine. They help with weight loss, lower blood pressure, and protect your heart and kidneys. Studies show they don’t raise pancreatitis risk - and may even lower the chance of recurrence compared to GLP-1 drugs. Side effects include yeast infections and dehydration, so you need to drink plenty of water.
Metformin
This is the oldest, cheapest, and most studied diabetes drug. It’s been around since the 1950s. Pancreatitis risk? About 0.15 per 1,000 patient-years - lower than most other options. It doesn’t cause weight loss like GLP-1 drugs, but it’s safe, effective, and widely used as a first-line treatment.
DPP-4 Inhibitors (e.g., Januvia, Onglyza)
These work by boosting your body’s own GLP-1. Sitagliptin (Januvia) shows no increased pancreatitis risk. But saxagliptin (Onglyza) carries a black box warning because of higher risk in one large trial. If you’re considering one of these, ask which one your doctor recommends.
Bupropion-Naltrexone (Contrave)
This combo drug is approved for weight loss. The JAMA study found it had far lower pancreatitis risk than GLP-1 agonists - about 1 case per 1,000 person-years versus 4.6 to 11.7 for GLP-1 drugs. But it’s not for everyone. It can cause anxiety, insomnia, or seizures in people with a history of eating disorders or seizures.
Orlistat (Xenical)
This drug blocks fat absorption in your gut. It’s safe for the pancreas, but it causes oily stools, gas, and frequent bowel movements. About 30-40% of people quit using it within a year because of the side effects.
Emerging Options
Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 agonist. It’s even more effective for weight loss than semaglutide. But since it still acts on GLP-1 receptors, experts assume it carries similar pancreatitis risks - though long-term data isn’t available yet. The FDA is requiring a post-marketing study to track its safety through 2027.
Should You Stop Taking Your GLP-1 Agonist?
No - unless you have symptoms or your doctor advises it.
These drugs don’t just help you lose weight. They reduce your risk of heart attack, stroke, and kidney failure. For people with type 2 diabetes, the cardiovascular benefits alone often outweigh the tiny pancreatitis risk. A 2024 study showed GLP-1 agonists cut heart disease deaths by 26% over five years.
What’s changing isn’t the drug - it’s how we think about risk. Instead of treating pancreatitis as a class-wide danger, doctors are learning to identify who’s truly at risk. If you’re a smoker with high triglycerides and kidney disease, you need closer monitoring. If you’re a healthy person with obesity and no prior pancreatitis, your risk is minimal.
Final Thoughts
GLP-1 agonists are powerful tools. But like all powerful tools, they need respect. Don’t ignore the warnings - but don’t let fear stop you from getting the help you need.
Know your symptoms. Talk to your doctor about your personal risk factors. Get baseline labs if you’re high-risk. And if you’re unsure about your current medication, ask about alternatives. There’s no one-size-fits-all answer - but there is a smart, personalized approach.
The goal isn’t to avoid all risk. It’s to manage it - so you can live longer, healthier, and with fewer complications.



Comments
I've been on Ozempic for 8 months and my pancreas is fine 🤷♂️ but my dog started crying every time I eat now. He's jealous. Also, my pants are falling off. Win win.
So let me get this straight - you're telling me the same drugs that are making people lose 50 lbs are also quietly murdering their pancreases? 🤡 And we're still prescribing these like they're vitamin gummies? I'm not scared - I'm just done trusting Big Pharma's fairy tales. Wake up, people.
I just read this whole thing and now I'm crying. Not because of the science - because I spent $1200 on Wegovy and now I'm terrified I'm gonna die from a pancreas that looks like a burnt marshmallow. My doctor said it's fine. But what does she know? She's got a Starbucks loyalty card and a LinkedIn profile.
Hey everyone - I just want to say you're all doing amazing. Whether you're on GLP-1s, metformin, or just trying to drink more water, you're showing up for yourself. That's huge. And if you're scared? That's okay. Talk to your doc. Ask questions. You're not alone in this. We're all just trying to be healthier, one step at a time. 💪❤️
The meta-analysis from JAMA in 2023 had a sample size of 5,000 - underpowered for pancreatitis outcomes, which occur at a rate of ~0.3% per year. The 9-fold increase is statistically insignificant given the low baseline incidence. The 1M-patient studies are far more reliable. Also, amylase/lipase monitoring is not clinically useful unless symptoms are present - false positives are common. Don't get lab-happy.
I’m a nurse practitioner who’s prescribed these for years. I’ve seen maybe two cases of pancreatitis in total - both in patients with heavy alcohol use and triglycerides over 800. The real danger isn’t the drug - it’s ignoring the lifestyle factors. If you’re smoking, drinking, and eating pizza every night while on Ozempic, yes, your pancreas is going to hate you. But the drug? It’s doing its job. Focus on the whole picture.
so i took semaglutide for 6 months and lost 38 lbs and my blood sugar is now normal but i also had this weird pain in my side once and i thought i was dying but it went away after 2 days and my dr said its probably just gas?? idk man i just wanna live long enough to see my nephew graduate high school
Ah yes, the classic 'the science is messy' cop-out. What that really means is: we have no idea what's happening, but we're making billions so let's just tell people to 'monitor' and hope they don't die before their next insurance renewal. I'm starting a cult. Worship the pancreas. It's the only organ that didn't ask for this.
The risk is low. The benefits are high. The data is complex. The choice is personal. Consult your physician. Monitor symptoms. Do not discontinue without medical advice.
Actually, the FDA warning was lifted in 2022 for most GLP-1s - but nobody tells you that because the media loves fear. Also, I read the original 2007 case reports - three of the four patients were alcoholics who had never been diagnosed with diabetes. Coincidence? I think not. This whole thing is a scam to sell more tests.
I'm from India and we don't have Ozempic here yet - but my cousin in Canada took it and lost weight like crazy. His doctor said he's low risk because he doesn't drink and his triglycerides are normal. He's doing great. I think it's about knowing your body, not fearing the medicine. We've been using natural herbs for pancreas health for centuries - maybe we should mix old wisdom with new science?