Every year, millions of people take generic drugs because they’re affordable and just as effective as brand-name versions. But behind that simplicity lies a hidden risk: contamination. Not all generic drugs are made the same. Some contain invisible impurities-chemical residues, bacteria, even metal particles-that can make you sick instead of helping you feel better. This isn’t rare. In 2022, generic drug contamination caused nearly 4 out of 10 drug recalls in the U.S., according to FDA data. And most of these problems come from overseas factories with weak oversight.
Where Does Contamination Come From?
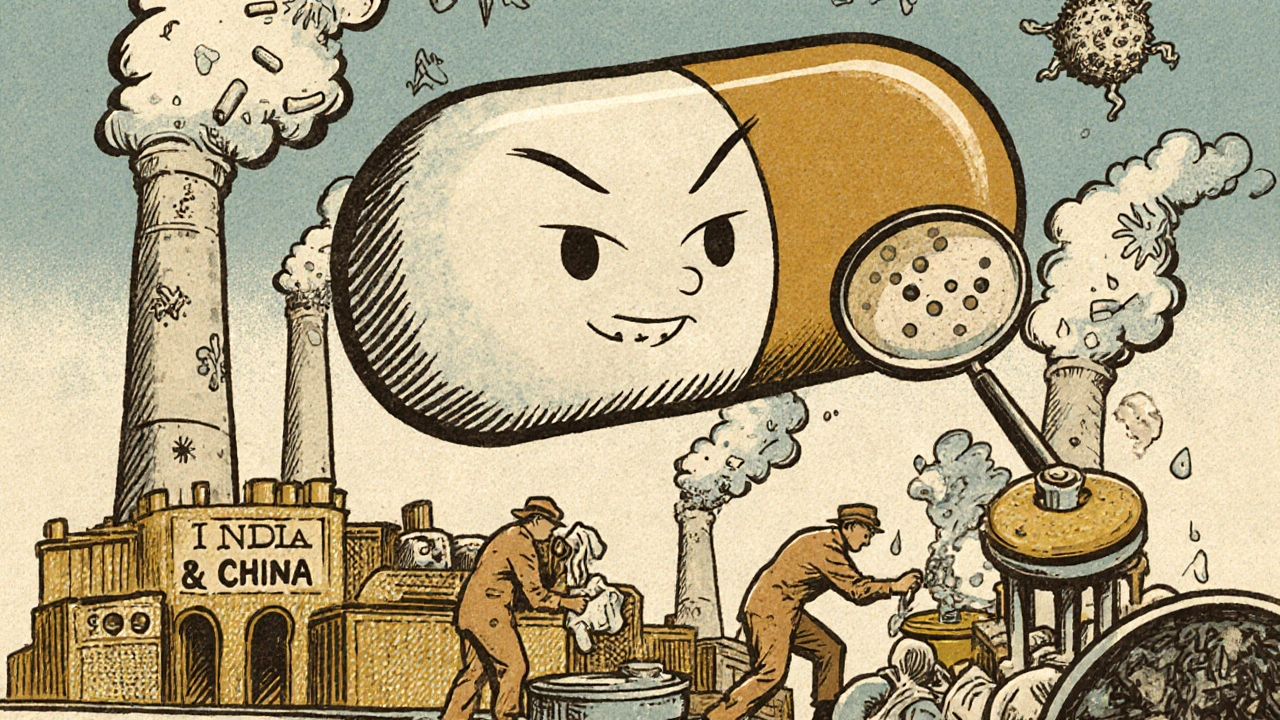
Contamination doesn’t happen by accident. It’s built into the system. About 80% of the active ingredients in U.S. generic drugs are made in just two countries: India and China. These factories often produce dozens of different drugs on the same equipment. One day it’s making blood pressure pills, the next day it’s making antibiotics. If cleaning between batches isn’t perfect, leftover chemicals stick around. That’s cross-contamination. The risk gets worse when workers handle drugs manually. People shed about 40,000 skin cells every minute. Each one carries particles that can land in a pill bottle. In cleanrooms, even small mistakes-like pulling a needle out of a vial or breaking an ampule-can introduce microbes. OSHA found that 62% of hazardous drug contamination incidents involve needle handling. Then there’s the environment. Older factories built before 2000 have 34% higher contamination rates. They weren’t designed for today’s strict standards. Some don’t even meet minimum ISO Class 8 air quality levels for non-sterile drugs. And cleaning? Many facilities only test for residue levels of 10 parts per million. But for powerful drugs like cancer treatments, that’s not enough. A tiny amount left behind can cause serious harm.Why Are Generics More at Risk?
Generic manufacturers don’t have the same resources as big pharma. Brand-name companies often spend 60-70% of their revenue on R&D and quality control. Generic makers operate on 20-25% margins. That means fewer staff, older equipment, and less money for advanced testing. FDA inspections show that 8.3% of generic drug facilities received violation notices for contamination control in 2022-nearly twice the rate of brand-name sites. Indian facilities had 12.7% of inspections flagged for contamination issues, compared to just 6.4% for U.S.-based plants. It’s not that all Indian factories are unsafe. Some, like Teva’s Bologna plant, cut cross-contamination by 78% using closed manufacturing systems. But the average factory? It’s playing catch-up. The problem isn’t just about money. It’s about oversight. The FDA inspects only 1% of imported drugs before they reach U.S. shelves. That means most contamination goes undetected until someone gets sick.What Happens When a Drug Is Contaminated?
Contamination doesn’t always show up right away. Sometimes it’s harmless. Other times, it’s deadly. In 2018-2019, a group of blood pressure meds called sartans were found to contain nitrosamines-cancer-causing impurities. Over 2,000 products were recalled across eight countries. The cost? More than $1.2 billion. Patients had to switch meds mid-treatment. Some saw their blood pressure spike. Others developed rashes, nausea, or liver damage. More recent cases are just as alarming. On Reddit’s r/pharmacy, a pharmacist posted in January 2022 about metronidazole tablets with blue specks. Lab tests confirmed copper contamination. Copper isn’t just a foreign substance-it’s toxic in high doses. That batch could have caused neurological damage. The FDA’s MedWatch database recorded over 1,200 contamination reports between 2020 and 2022. Nearly 400 of them involved actual patient harm. One case involved a generic hydrocortisone cream that caused severe skin burns because of microbial overgrowth. Another patient developed pneumonia after taking a contaminated oral antibiotic. And here’s the worst part: most patients never know. If your headache medicine tastes weird or looks discolored, you might think it’s just old. You don’t realize it’s contaminated. Pharmacists, too, often lack the tools to test. A 2022 survey found that 63% of independent pharmacies can’t verify if a generic drug is safe.
How Are Companies Trying to Fix This?
Some manufacturers are stepping up. Mylan’s facility in Morgantown reduced contamination incidents by 82% between 2019 and 2022 by installing real-time particle monitors. These sensors track airborne particles 24/7 and alert staff the moment levels rise. They also upgraded gowning procedures-changing how workers dress before entering cleanrooms. Other companies are switching to closed systems. Instead of open vials and manual transfers, drugs move through sealed tubes and robotic arms. This cuts human contact by over 90%. Rapid microbiological testing is another game-changer. Instead of waiting 7 days for lab results, some plants now get answers in 4 hours. That means contaminated batches are caught before they leave the facility. The FDA is also changing. In 2023, they made nitrosamine testing mandatory for all sartan drugs. Their new PREDICT system now flags 37% more risky shipments than before. And by 2024, they plan to roll out AI tools that analyze 15,000 data points per factory to predict contamination risks with 89% accuracy. But these fixes cost money. Upgrading a single production line with a closed isolator system can run $1-2 million. Most generic companies can’t afford that. So progress is slow.What Can You Do as a Patient?
You can’t test your pills at home. But you can stay alert. - Check for changes. If your generic pill looks different-new color, shape, size, or taste-ask your pharmacist. It might be a different manufacturer. That’s normal. But if it has specks, discoloration, or a strange odor, don’t take it. - Report anything suspicious. If you feel worse after starting a new generic, or notice unusual side effects, file a report with the FDA’s MedWatch system. Your report helps track patterns. In 2021, a single patient’s report led to the recall of a contaminated hydrocortisone cream. - Know your manufacturer. Ask your pharmacist which company made your drug. Some brands have better records. Teva, Sandoz, and Mylan have invested heavily in contamination controls. Smaller, unknown makers? They’re riskier. - Don’t assume “cheap” means “safe.” The cheapest option isn’t always the best. Sometimes paying a little more for a trusted generic saves you from hospital visits later.
What Should Pharmacies and Hospitals Do?
Pharmacists are on the front lines. They need better tools. - Use visual inspection. Hold pills up to the light. Look for discoloration, cracks, or foreign particles. If you see anything odd, set it aside. - Check lot numbers. When a recall happens, pharmacies can trace affected batches. If your drug’s lot number matches a recall, return it immediately. - Train staff regularly. OSHA found that 63% of compounding pharmacies lack proper engineering controls. Staff need annual training on contamination risks, especially when handling hazardous drugs like chemotherapy. - Push for better sourcing. Hospitals should prioritize suppliers with documented GMP compliance and third-party audit reports. If a supplier refuses to share inspection data, find another.Is There Hope for the Future?
Yes. But it won’t come from luck. It will come from pressure. Regulators are finally catching up. The FDA’s new AI tools, faster testing methods, and stricter import screening will reduce contamination over time. By 2027, experts predict a 40% drop in recalls thanks to these changes. But the real fix? Transparency. Patients deserve to know where their drugs come from. Pharmacies need access to real-time contamination data. Manufacturers must be held accountable-not just by regulators, but by the public. Until then, treat every generic drug like a product with hidden risks. Be informed. Be cautious. And never stop asking questions.Can generic drugs be as safe as brand-name drugs?
Yes, generic drugs are required by law to be identical in active ingredient, strength, dosage form, and route of administration to their brand-name counterparts. The FDA approves them based on the same quality standards. However, contamination risks can be higher in generics due to cost pressures, older facilities, and less oversight in global supply chains. While the drugs are therapeutically equivalent, their manufacturing environment may not always be.
How do I know if my generic drug is contaminated?
You won’t always know. Many contaminants are invisible. But signs include unusual color, odor, texture, or taste. If your pills have specks, look cloudy, or taste metallic, stop taking them. Check the lot number against FDA recall lists. If you feel worse after starting a new generic, report it to your doctor and the FDA’s MedWatch system.
Are all generic drugs made in India or China?
No, but the majority are. About 80% of active pharmaceutical ingredients (APIs) for U.S. drugs come from India and China. Some generic manufacturers in the U.S., Europe, and Canada produce drugs domestically, but they’re less common and often more expensive. Always ask your pharmacist where your drug’s ingredients are made.
What should I do if I suspect my medication is contaminated?
Stop taking the medication immediately. Contact your pharmacist to confirm the lot number and check for recalls. Report the issue to the FDA through MedWatch. If you’ve had symptoms like rash, nausea, dizziness, or fever after taking the drug, see your doctor. Keep the packaging and pills as evidence.
Why aren’t more generic drugs tested before they’re sold?
Testing every batch would make drugs too expensive. The FDA inspects only 1% of imported drugs before they enter the U.S. Instead, they rely on factory inspections and random sampling. Manufacturers are required to test their own products, but enforcement is inconsistent. This system works for most drugs-but fails when oversight is weak or corruption exists.
Can I trust my pharmacist to know if a drug is safe?
Most pharmacists do their best, but many lack the tools to test for contamination. A 2022 survey found that 63% of independent pharmacists can’t perform independent lab tests on generics. They rely on manufacturer certificates and FDA recalls. If you’re concerned, ask if they know the manufacturer and if they’ve seen issues with that batch before.



Comments
It’s wild how we just swallow these pills without a second thought. I never realized how much of our meds come from factories with outdated equipment and minimal oversight. The part about copper in metronidazole? That’s terrifying. I’ve taken that drug before and never thought to look at the tablets under light. I’m going to start doing that now.
India and China are being set up as the villains here, but let’s be real-Big Pharma outsourced everything to cut costs, then blames the factories. The FDA doesn’t inspect 1% of imports because they’re underfunded, not because they’re trying to protect us. This isn’t negligence-it’s policy. And now they want us to pay more for ‘trusted’ brands? Classic.
Let’s be honest-this is just fearmongering dressed up as public health. The odds of you being harmed by a contaminated generic are lower than getting struck by lightning. Most of these ‘cases’ are from decades-old batches or mislabeled products. The FDA’s recall rate is still under 0.001% of all prescriptions filled. Stop panicking and take your blood pressure meds.
lol so now im supposed to check my pills for specks? next u’ll tell me to test em with a stick or sumthin. i just want my zzzquil to work, not become a pharma detective. also why do u think they make generics cheaper if they’re all poison? 🤡
I appreciate the depth of this post. I’ve been a pharmacy tech for 12 years and I’ve seen a lot. The truth is, most generics are fine-but the ones that aren’t? They’re the ones that slip through. I always tell patients: if it looks weird, don’t take it. And if you’re unsure, call the pharmacy. We can check the lot number for you. Small steps matter.
What’s the data on contamination rates for generics made in the U.S. versus overseas? I know it’s a small percentage, but are there any studies comparing the actual impurity levels across manufacturing regions? I’m curious if the gap is as wide as the article suggests.
The FDA’s 1% inspection rate is not just inadequate-it’s criminal. If you imported 1% of your groceries without inspection, you’d be arrested for endangering public health. Yet we accept this for life-saving medication. The system is broken, and calling it ‘cost-effective’ is a euphemism for negligence. Someone needs to sue the FDA.
It’s important to recognize that the global pharmaceutical supply chain is a complex, interdependent system. While it’s easy to point fingers at foreign manufacturers, the demand for low-cost medications in the U.S. is what drives the entire structure. Consumers, insurers, and policymakers all share responsibility. Until we value safety over savings, these problems will persist. We need systemic reform-not just patient vigilance.
They’re hiding something. Always. Remember the Vioxx scandal? The opioid crisis? Now this. The FDA is in bed with Big Pharma. The same people who approved the contaminated sartans are still in charge. I bet you 100 bucks that the next big recall is already in the pipeline and they’re just waiting for the right moment to announce it. Don’t trust the system. Ever.
There is hope, and it’s in the hands of informed patients and responsible pharmacists. We must demand transparency from manufacturers and insist on third-party audits. Hospitals should refuse to stock generics without full disclosure of origin and testing protocols. This isn’t about fear-it’s about accountability. We deserve better than blind trust. Let’s use our collective voice to push for change.
I think about how much we rely on invisible things-air, water, medicine-and how little we know about where they come from. It’s humbling, and kind of scary. But maybe this is a wake-up call. Not to panic, but to pay attention. To ask questions. To care more. Maybe if enough of us start asking, the system will have to listen. We’re not just patients-we’re people who deserve to be safe.
check your lot #. if it’s bad, return it. that’s it. no need to overthink it.