Most people with chronic kidney disease (CKD) don’t know they have it-until it’s too late. By the time symptoms like fatigue, swelling, or trouble sleeping show up, the kidneys have already lost a lot of function. But here’s the truth: chronic kidney disease can be caught early, and when it is, progression can often be stopped-or at least slowed down significantly. This isn’t theory. It’s what happens in clinics where doctors use the right tests at the right time.
What Chronic Kidney Disease Really Means
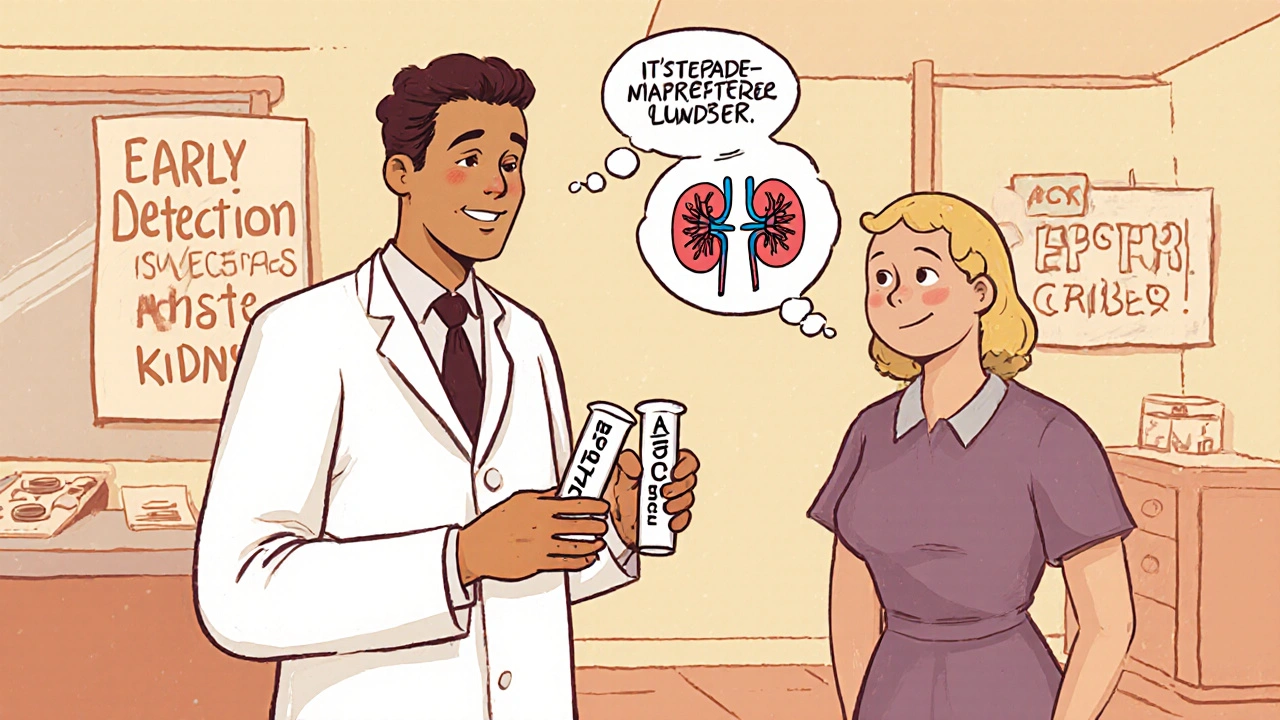
Chronic kidney disease isn’t just about high creatinine or a single blood test. It’s a long-term condition where the kidneys don’t work the way they should for at least three months. The damage might be from diabetes, high blood pressure, or something else entirely. But the key is this: it’s not sudden. It creeps in. And that’s why so many people miss it. The official definition from KDIGO and KDOQI guidelines is clear: CKD means either a reduced estimated glomerular filtration rate (eGFR) below 60 mL/min/1.73 m², or signs of kidney damage-like protein in the urine-lasting three months or longer. You need both pieces of evidence to confirm it. One test alone isn’t enough.The Two Tests That Change Everything
If your doctor only checks your serum creatinine, you’re not getting the full picture. Creatinine levels can look normal even when your kidneys are starting to fail-especially if you’re older, have low muscle mass, or are African American. That’s why relying on creatinine alone misses up to 40% of early cases. The real game-changer is combining two tests:- eGFR: This estimates how well your kidneys filter waste. It’s calculated using your creatinine level, age, sex, and race. The CKD-EPI equation is the current standard, but even this has limits.
- uACR: This measures albumin (a type of protein) in your urine. A value of 30 mg/g or higher means your kidneys are leaking protein-a clear red flag. The best sample is the first morning urine.
Staging: Knowing Where You Stand
CKD is broken into five stages. But stages 1 and 2 are where the fight begins:- Stage 1: eGFR ≥90, but uACR ≥30. Kidneys are still working well, but damage is present.
- Stage 2: eGFR 60-89, uACR ≥30. Slight decline, but still early.
- Stage 3a: eGFR 45-59. Mild to moderate loss.
- Stage 3b: eGFR 30-44. Moderate to severe.
- Stage 4: eGFR 15-29. Severe damage.
- Stage 5: eGFR under 15. Kidney failure. Dialysis or transplant needed.
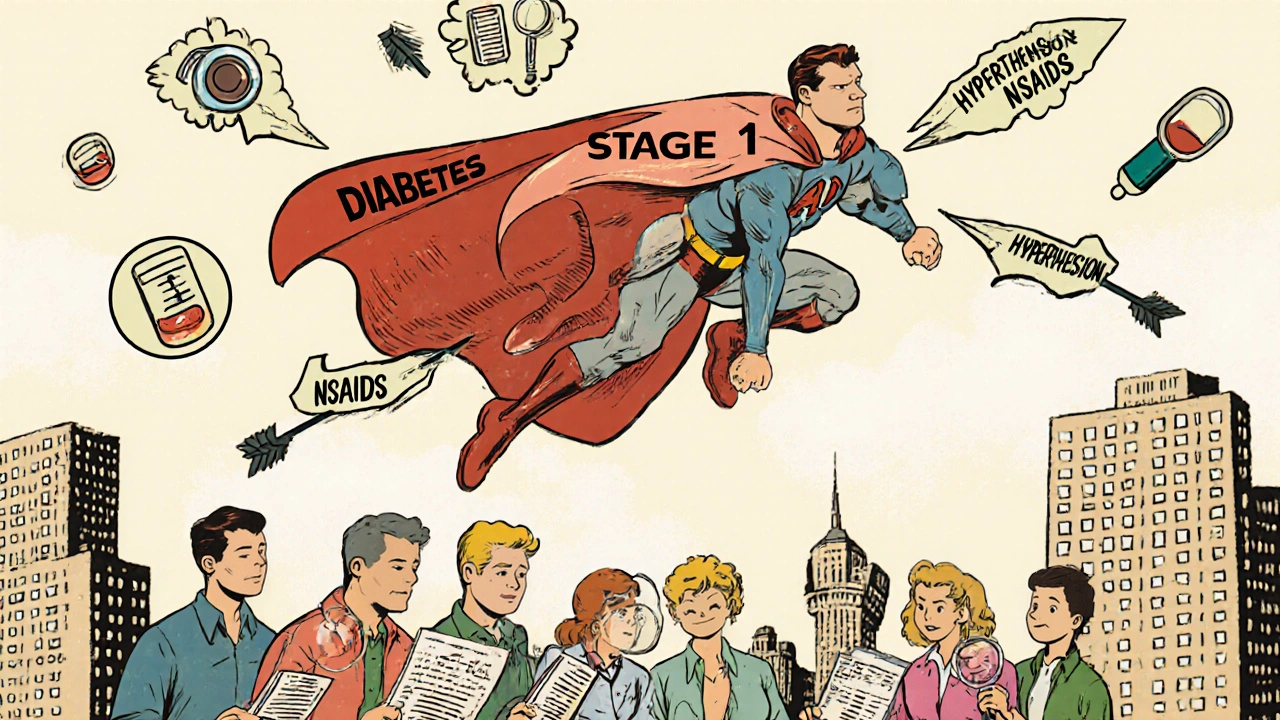
Who Should Be Tested-and How Often
Not everyone needs annual screening. But if you fall into one of these groups, you’re at risk:- People with type 1 or type 2 diabetes (screen annually after diagnosis)
- People with high blood pressure (screen at every visit, full test yearly)
- Those with a family history of kidney failure
- African Americans, Native Americans, and Hispanic individuals (3.7x higher risk for African Americans)
- People on long-term NSAIDs, certain antibiotics, or other kidney-toxic drugs
- Anyone over 60
What Happens When You Catch It Early
This isn’t just about avoiding dialysis. It’s about living longer, healthier, and with fewer heart problems-because CKD isn’t just a kidney issue. It’s a cardiovascular risk factor. Studies show that when CKD is caught in stages 1 or 2 and managed properly:- Blood pressure control below 130/80 mmHg reduces progression risk by 27% (SPRINT trial data).
- SGLT2 inhibitors (like dapagliflozin or empagliflozin) cut the risk of kidney failure by 32% in people with albuminuria (CREDENCE trial).
- Comprehensive care-including diet, medication, and education-slows eGFR decline from 3.5 mL/year to just 1.2 mL/year.
Why So Many Cases Are Still Missed
Despite the guidelines, most primary care providers don’t order both tests. A 2022 study found only 52.7% of doctors consistently order eGFR and uACR together. In rural clinics, that number drops to under 32%. Why?- Electronic health records don’t prompt for both tests.
- Doctors think “normal creatinine” means normal kidneys.
- Patients don’t ask for the test because they don’t know it exists.
What’s Changing Right Now
The tide is turning. In 2023, the FDA cleared the first AI tool-NephroSight by Renalytix-that analyzes 32 clinical factors to predict CKD risk before eGFR drops. It’s already being used in some VA hospitals. The Biden administration’s 2023 Executive Order on Kidney Health is funding $150 million to roll out dual-testing in Federally Qualified Health Centers by 2026. That’s 1.2 million more people who could be diagnosed early. And soon, point-of-care uACR tests-devices that give results in minutes instead of days-could be available in doctor’s offices. The Kidney Health Initiative predicts this could boost screening rates by 40%.What You Can Do Today
If you’re at risk, here’s your action plan:- Ask your doctor for an eGFR and uACR test-don’t accept just creatinine.
- If you have diabetes or high blood pressure, make sure you’re getting both tests every year.
- Request your results. Know your numbers. Don’t let them just say “everything’s fine.”
- If your uACR is over 30, ask about SGLT2 inhibitors or ACE inhibitors-they’re proven to protect your kidneys.
- Reduce salt, avoid NSAIDs like ibuprofen long-term, and control your blood sugar and blood pressure.
Why This Matters Beyond the Kidneys
CKD doesn’t just affect your kidneys. It increases your risk of heart attack, stroke, and early death. The annual cost of kidney disease in the U.S. is $120 billion-mostly from treating late-stage disease. But studies show early detection saves $1,850 per patient per year by preventing complications. That’s not just money. That’s time. That’s mobility. That’s avoiding dialysis. That’s staying alive longer, healthier, and on your own terms. The science is clear. The tools exist. The guidelines are in place. What’s missing is action-from doctors, from patients, from the system. You can’t fix what you don’t know. But if you know, you can stop it. Before it’s too late.Can chronic kidney disease be reversed?
Early-stage CKD (stages 1 and 2) can often be stabilized or even improved with proper treatment. While damaged kidney tissue doesn’t regenerate, stopping further damage is possible. Controlling blood pressure, managing diabetes, using kidney-protective medications like SGLT2 inhibitors, and following a low-sodium diet can halt or significantly slow progression. Many people live for decades with stage 1 or 2 CKD without advancing.
If my creatinine is normal, do I still need to be tested for CKD?
Yes. Serum creatinine can be normal even when kidney damage is present-especially in older adults, people with low muscle mass, or those with early-stage disease. The urine albumin-to-creatinine ratio (uACR) detects damage that creatinine misses. Up to 40% of early CKD cases are missed if only creatinine is checked. Always ask for both tests if you’re at risk.
What does a uACR result of 30 mg/g mean?
A uACR of 30 mg/g or higher means you have albuminuria-protein leaking into your urine. This is a sign of kidney damage. It’s classified as A2 (moderate) under KDIGO guidelines. Even if your eGFR is normal, this alone qualifies you for a CKD diagnosis if it persists for three months or longer. This is a key warning sign that needs medical attention.
Are there medications that can protect my kidneys if I have early CKD?
Yes. Two classes of drugs have strong evidence: SGLT2 inhibitors (like dapagliflozin, empagliflozin) and ACE inhibitors or ARBs. SGLT2 inhibitors reduce the risk of kidney failure by 32% in people with albuminuria, according to the CREDENCE trial. ACE/ARBs lower blood pressure and reduce protein leakage. These aren’t just for diabetes-they’re now standard for early CKD with proteinuria, even without diabetes.
Why is race used in eGFR calculations?
Race was historically included because Black patients tend to have higher muscle mass, which can lead to higher creatinine levels-even with normal kidney function. This adjustment was meant to avoid overdiagnosis. But recent research shows it can delay diagnosis in Black patients by masking early kidney damage. New eGFR equations (like the 2021 CKD-EPI creatinine-cystatin C equation) no longer include race. Many labs are switching to race-neutral formulas, which may improve early detection in high-risk populations.
Can I check for CKD at home?
Currently, no FDA-approved home test can replace the clinical eGFR and uACR. Some over-the-counter urine strips detect protein, but they’re not accurate enough for diagnosis. They can give false positives or negatives. The only reliable way is a lab test ordered by your doctor. However, point-of-care uACR devices are expected to be available in clinics by 2025, making testing faster and more accessible.
What lifestyle changes help slow CKD progression?
Four key changes make a difference: (1) Keep blood pressure under 130/80 mmHg; (2) Control blood sugar if you have diabetes; (3) Reduce sodium to under 2,300 mg per day (avoid processed foods); (4) Avoid long-term use of NSAIDs like ibuprofen or naproxen. Quitting smoking and maintaining a healthy weight also help. A diet rich in vegetables, whole grains, and lean proteins-not a low-protein diet unless advised-is recommended for early CKD.
How often should I get tested if I’m at risk?
If you have diabetes, get both eGFR and uACR tested annually. If you have high blood pressure, get tested at least once a year-more often if your numbers are unstable. If you’re over 60 with no risk factors, discuss testing with your doctor. Anyone with a family history of kidney failure should be tested every year starting at age 40. Don’t wait for symptoms. Early detection is silent but powerful.




Comments
eGFR + uACR is non-negotiable if you're at risk. Creatinine alone is a lie. Period.
man i just had my doc check creatinine for 5 years straight until i asked for the uACR. turned out i was stage 2 with 85 albumin. he looked at me like i spoke greek. now i'm on dapagliflozin and my numbers are stable. if you're diabetic or hypertensive and your doc doesn't order both tests, find a new one. this ain't rocket science, it's basic care. the system is broken but you can fight it.
Just had my first uACR test last month. 42 mg/g. eGFR was 70. Docs said 'nothing to worry about' but I knew better. Followed up with a nephrologist. They confirmed stage 2 CKD. Started on an ACE inhibitor and cut salt like my life depended on it (it does). Two months later, uACR down to 28. This stuff works. Don't wait for symptoms. Get tested. You owe yourself that.
uACR is the silent alarm. Creatinine is the snooze button. If you're over 60 or have diabetes, demand both. No excuses. Your kidneys don't yell. They whisper. And if you ignore the whisper, they stop talking forever.
so let me get this straight… we have AI tools that can predict kidney failure before eGFR drops, but most primary care docs still think 'normal creatinine' = 'healthy kidneys'? and we're surprised people end up on dialysis? i mean… wow. just wow. 🤦♂️
i used to think kidney stuff was for old people or diabetics but then my mom got diagnosed at 58 with no symptoms. turns out she had a family history and never got tested. now i'm 34 and i get both tests every year. its like a car checkup but for your insides. and honestly? it’s the only thing keeping me from being one of those stats. you don’t need to be scared. just informed.
Early detection saves lives. 🙏
My brother went from stage 2 to stable for 8 years after catching it early. He’s still working, hiking, playing with his kids. No dialysis. No transplant. Just consistent care.
Don’t wait. Ask. Know your numbers. You’ve got this.
Don't accept 'normal creatinine' as a diagnosis. It's not a diagnosis. It's an omission. Request eGFR and uACR. Always. If your doctor resists, get a second opinion. Your kidneys can't argue back. You have to.
just got my results back: uACR 35, eGFR 68. doc said 'eh, keep an eye on it'... i said 'nah, i want a plan'. now i'm on an SGLT2i and seeing a dietitian. also deleted my ibuprofen app 😅. this isn't scary if you act early. it's empowering. 🌱💪
They're not testing because they're lazy. Or because the EHR doesn't prompt. Or because they don't get paid for it. But here's the truth: if you're at risk and you don't get both tests, you're not being cared for-you're being neglected. Demand better. Your life isn't a billing code.
Isn't it tragic? We live in a world where we can map the human genome, yet we still allow people to drift into kidney failure because we refuse to run two simple tests? The system doesn't care about you. It cares about cost centers and metrics. And yet… you're expected to be your own advocate? That's not healthcare. That's survival theater. And the worst part? The people who suffer the most are the ones who can't fight back. I weep for them.
Per KDIGO 2023, uACR ≥30 mg/g is A2 albuminuria, which independently predicts CKD progression and CVD events-even when eGFR is preserved. The 2021 CKD-EPI cystatin C equation eliminates race bias and improves sensitivity in early-stage disease. SGLT2i reduces ESKD risk by 32% in A2/A3 populations per CREDENCE. This isn't opinion. It's evidence-based medicine. If your provider isn't aligned, seek one who is.