When you’re on antibiotics and your stomach starts acting up, it’s tempting to grab an antacid. But if you take them together, you might be ruining your antibiotic’s effectiveness-without even knowing it. This isn’t a myth. It’s a well-documented, clinically significant interaction that affects millions of people every year. And the worst part? Most of these cases are completely preventable with simple timing adjustments.
Why Antacids and Antibiotics Don’t Mix
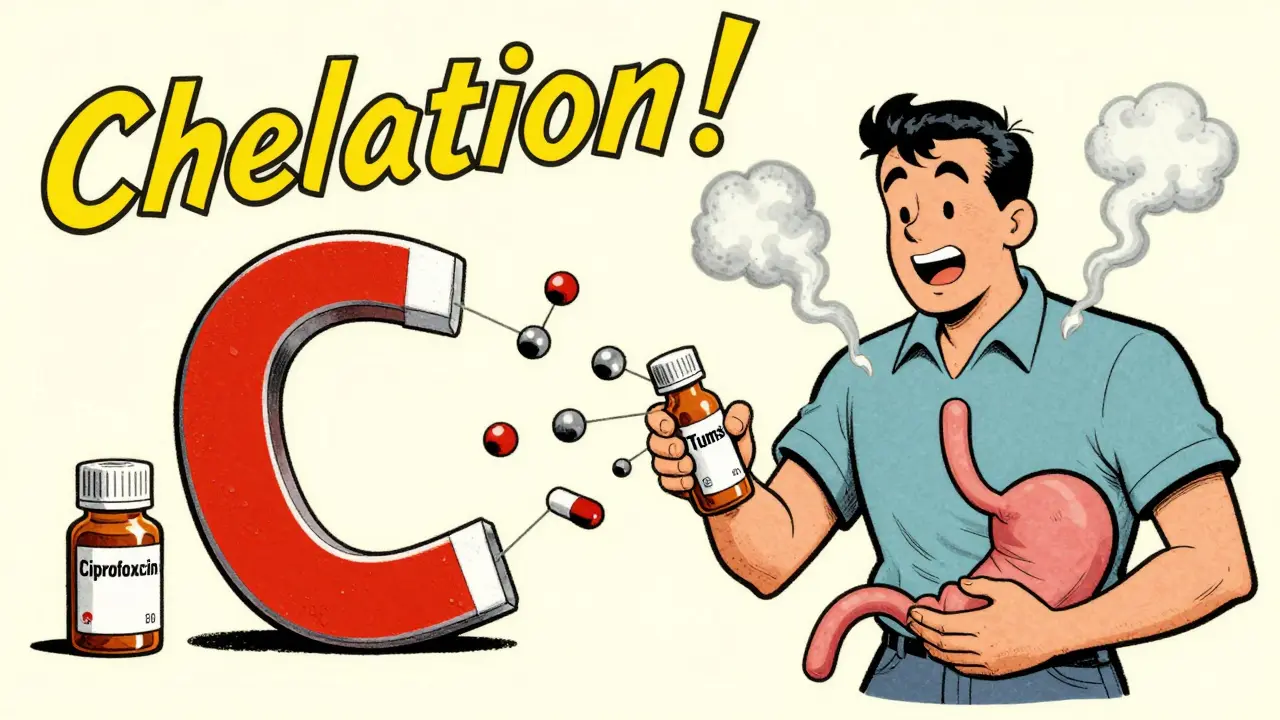
Antacids like Tums, Rolaids, or Maalox work by neutralizing stomach acid. That’s great for heartburn. But your antibiotics? They need that acid to dissolve and get absorbed properly. More importantly, antacids containing aluminum, magnesium, or calcium bind directly to certain antibiotics in your gut, forming a chemical compound your body can’t absorb. This is called chelation.Think of it like putting a magnet next to iron filings. The antibiotic molecules stick to the metal ions in the antacid, and suddenly, they’re stuck in your gut instead of entering your bloodstream. The result? Your antibiotic dose becomes useless. Studies show that taking ciprofloxacin with an antacid can cut its absorption by up to 90%. That’s not a small drop-it’s treatment failure waiting to happen.
Which Antibiotics Are Most Affected?
Not all antibiotics are equally vulnerable. Some are barely touched by antacids. Others? They’re extremely sensitive.High-risk antibiotics: Fluoroquinolones like ciprofloxacin and levofloxacin, and tetracyclines like doxycycline and tetracycline. These are the big ones. Ciprofloxacin, for example, can lose up to 90% of its effectiveness if taken within two hours of an antacid. Doxycycline isn’t far behind-its absorption drops by about 30% even with a single antacid pill.
Moderate-risk: Penicillins like amoxicillin and cephalosporins like cephalexin. These show a smaller reduction-around 15-20%-but it’s still enough to matter, especially if you’re treating something serious like pneumonia or a stubborn UTI.
Low-risk: Macrolides like azithromycin and clarithromycin. These are mostly safe, but experts still recommend spacing them out by two hours just to be safe. And then there’s metronidazole. It doesn’t interact at all. That’s good news if you’re prescribed it-you can take your antacid without worry.
How Long Should You Wait?
Timing isn’t guesswork. It’s science. And the numbers are clear:- For fluoroquinolones (ciprofloxacin, levofloxacin): Wait 4 hours after taking an antacid, or take the antibiotic 2 hours before the antacid.
- For tetracyclines (doxycycline, tetracycline): Separate by 2-3 hours.
- For penicillins and cephalosporins: A 1-2 hour gap is usually enough.
- For macrolides: Stick to a 2-hour gap as a precaution.
These aren’t suggestions-they’re evidence-based guidelines from the FDA, NHS, and Cleveland Clinic. And they’re backed by real-world data. One study tracked 15,000 patients with urinary tract infections. Those who took ciprofloxacin with antacids had a 22% higher rate of treatment failure. That’s not a small risk. That’s a medical mistake.

What About Other Acid Reducers?
You might be thinking, “What if I take something like Pepcid or Prilosec instead?” Those are H2 blockers and proton pump inhibitors (PPIs). They’re not antacids, but they still reduce stomach acid.Here’s the good news: They don’t cause chelation. That means no direct binding to antibiotics. But they can still slightly reduce absorption of some drugs by changing the stomach’s pH. For most antibiotics, this effect is minor. Still, if you’re on a high-risk antibiotic like ciprofloxacin, spacing it out by 2 hours from any acid-reducing medication is the safest move.
Here’s a practical tip: If you need acid control long-term-say, for chronic reflux-talk to your doctor about switching from antacids to an H2 blocker or PPI. A 2023 study found that switching cut treatment failure rates in half-from 27% down to 9%-for patients on antibiotics who needed ongoing acid suppression.
Real Stories: What Happens When People Don’t Time It Right
You don’t have to take our word for it. Look at what’s happening in real life.A woman in Ohio kept getting recurrent UTIs. Her doctor kept prescribing ciprofloxacin. Each time, she took it with her daily Tums for heartburn. After three failed treatments, her pharmacist noticed the pattern. She was told to take the antibiotic two hours before her antacid. The next infection cleared in five days.
On Reddit, a nurse shared that five of her patients in the past year had treatment failures-each one linked to taking antibiotics with antacids. Once they fixed the timing, the infections vanished.
And it’s not just patients. Doctors report that about 18% of apparent antibiotic failures in primary care are due to improper timing with antacids. That’s not resistance. That’s a simple scheduling error.
How to Actually Remember to Space Them Out
Let’s be honest: Remembering to wait two, three, or four hours between pills is hard. Especially if you’re on antibiotics twice a day, have other meds, and feel sick.Here’s what works:
- Use a pill organizer with time slots. Buy one with AM/PM and labeled times like “8 AM,” “10 AM,” “2 PM,” etc. Put your antibiotic in one slot, your antacid in another, with a clear gap.
- Set phone alarms. Name them clearly: “Ciprofloxacin NOW,” “Wait 4 hours,” “Tums NOW.”
- Ask your pharmacist. Most will give you a printed schedule. Some even offer free medication reviews.
- Use apps. MyMedSchedule and Medisafe have built-in alerts for antacid-antibiotic interactions. Over 1.2 million people use them.
One Mayo Clinic study found that giving patients a simple visual chart showing the safe timing windows reduced dosing errors by 37%. Sometimes, seeing it on paper makes all the difference.
The Bigger Picture: Why This Matters
This isn’t just about your next infection. It’s about antibiotic resistance.When antibiotics don’t reach effective levels in your body, bacteria don’t die-they adapt. Subtherapeutic doses are one of the biggest drivers of resistant strains. The CDC estimates that 15% of new fluoroquinolone resistance cases are linked to this exact issue.
And the cost? In the U.S. alone, unnecessary treatment failures from this interaction cost the healthcare system over $1.2 billion a year. More doctor visits. More tests. More antibiotics. More resistance.
Proper timing is one of the cheapest, simplest, and most effective ways to fight that.
What’s Changing in 2025?
The field is evolving. In 2023, the FDA approved a new extended-release form of ciprofloxacin called Cipro XR-24. In clinical trials, it showed only an 8% drop in absorption when taken with antacids-compared to 90% for the old version. This could be a game-changer for patients who need both acid control and antibiotics.Also, newer EHR systems like Epic now give specific timing instructions-not just a generic “interaction warning.” At Massachusetts General Hospital, that change cut timing errors by 41% in just six months.
Looking ahead, researchers are exploring personalized dosing based on genetics. Some people naturally empty their stomachs faster or slower. In the future, your dosing schedule might be tailored to your biology.
But for now? Stick to the basics. Time your doses. Talk to your pharmacist. Don’t assume it’s fine because you’ve done it before. Antibiotics are powerful. Antacids are simple. But together? They can mess things up-easily, quietly, and dangerously.
Can I take antacids and antibiotics at the same time if I really need to?
No. Taking them together can reduce antibiotic absorption by up to 90% for drugs like ciprofloxacin and doxycycline. This can lead to treatment failure, longer illness, and even antibiotic resistance. Always separate them by the recommended time window-usually 2 to 4 hours.
Which antacids are safest to use with antibiotics?
No antacid is completely safe with all antibiotics. Those with aluminum, magnesium, or calcium are the most problematic. If you must use one, choose a calcium-based antacid only if you’re on a low-risk antibiotic like amoxicillin, and wait at least 2 hours. For high-risk antibiotics, avoid them entirely and use H2 blockers like famotidine instead.
What if I forget and take them together? Should I take another dose?
Don’t double up. Taking an extra dose can cause side effects like nausea, dizziness, or even liver stress. Instead, take your next dose as scheduled, but make sure to space it properly from your antacid going forward. If you’re concerned about treatment effectiveness, contact your doctor-especially if you’re treating a serious infection.
Do all antibiotics interact with antacids?
No. Antibiotics like metronidazole, azithromycin, and penicillin have minimal or no interaction with antacids. But unless you’re sure, assume there’s a risk. Always check with your pharmacist or doctor before combining any new medication with an antacid.
Can I use natural remedies like baking soda instead of antacids?
Baking soda (sodium bicarbonate) is an antacid too. It contains sodium and can raise stomach pH, which may still interfere with some antibiotics. It doesn’t cause chelation like aluminum or magnesium antacids, but it’s not risk-free. Stick to medically approved options and avoid self-treating with home remedies while on antibiotics.


Comments
I took cipro with Tums once and thought I was fine until the UTI came back worse. Never again. Just space it out.
This is why I love pharmacists 😊 I asked mine before starting my antibiotics and she printed me a little chart with times. Game changer. 🙌
In India we just take antacid after food and antibiotic on empty stomach so no problem. Americans overcomplicate everything
The chelation mechanism is well-documented in pharmacokinetic literature-divalent cations like Ca²⁺, Mg²⁺, and Al³⁺ form insoluble complexes with fluoroquinolones via carboxyl and ketone groups, drastically reducing bioavailability. Also, gastric pH modulation affects ionization states. Bottom line: timing isn't optional.
This is exactly the kind of information patients need. Too many assume 'it's just an antacid' and don't realize they're sabotaging their treatment. Kudos to the author for laying it out clearly.
It’s wild how something so small-a two-hour gap-can change the entire trajectory of your health. We treat antibiotics like magic bullets, but they’re actually delicate tools. Respect the chemistry.
I’ve been telling my patients this for years. If they’re on doxycycline and have heartburn, I give them famotidine instead of Tums. Simple swap, huge difference. And no, baking soda isn’t safer-it’s just a different kind of mess.
My grandma used to take Tums with everything. She had a bad infection last year and it didn’t clear up. Turns out she was taking her amoxicillin right after her antacid. We switched her to a pill organizer and boom-problem solved. Sometimes the fix is just organization.
Why do you even need antacids? Eat less junk food. Stop being weak. This is why the West is collapsing.
The FDA guidelines are laughably vague. Real clinicians know you need a 4-hour window for fluoroquinolones regardless of 'usually'. This post is amateur hour.
Bro i just set 2 alarms one for my abx one for the tums and it works. no need to overthink. also i use medisafe app and it beeps like a boss. 🤘