Acute interstitial nephritis isn’t something most people hear about until their kidneys start acting up. It’s not a common diagnosis, but when it happens, it can turn a routine medication into a serious threat. This condition isn’t caused by infection or trauma-it’s your immune system turning on your kidneys because of a drug you took. And the worst part? It often flies under the radar. No fever. No rash. Just a slow drop in kidney function that gets mistaken for dehydration or a urinary tract infection.
What Exactly Is Acute Interstitial Nephritis?
Acute interstitial nephritis (AIN) means inflammation in the spaces between the kidney’s filtering units-the tubules and interstitium. Think of your kidneys as a network of tiny filters. When the tissue around those filters swells up, they can’t work properly. The result? Waste builds up, fluid gets stuck, and your creatinine levels rise. You might feel tired, nauseous, or notice you’re peeing less. Sometimes you won’t feel anything at all until a blood test shows your kidney function has dropped.
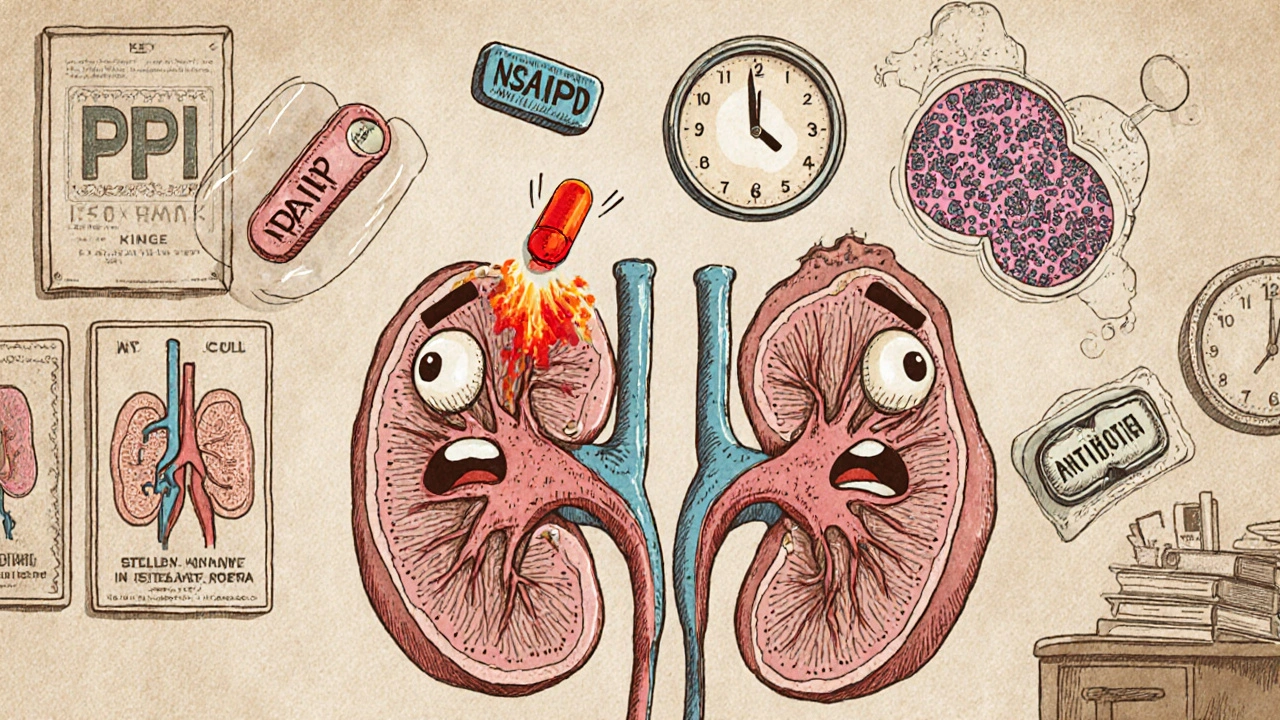
It’s not one disease. It’s a reaction. And the biggest trigger? Medications. About 60 to 70% of all cases come from drugs. Over 250 different medications have been linked to AIN. That’s more than most doctors realize. Some are obvious-antibiotics, NSAIDs. Others are everyday pills you never think twice about, like heartburn meds.
The Top Culprits: Which Drugs Cause the Most Damage?
Not all drugs are equal when it comes to triggering AIN. The most common offenders today aren’t what they were 20 years ago.
- Proton pump inhibitors (PPIs) like omeprazole, pantoprazole, and esomeprazole are now the second most common cause. Once rare, they now account for nearly 4 in 10 cases. People take them for months or years for heartburn, acid reflux, or ulcers. Then, out of nowhere, their kidneys start failing. It’s not immediate-it can take 6 months to 2 years. That’s why so many cases are missed.
- Antibiotics like penicillin, cephalosporins, and ciprofloxacin still make up about 30% of cases. These tend to hit faster-often within 10 days. You might get a rash, fever, or feel generally unwell. But even then, doctors often blame it on a viral infection.
- NSAIDs like ibuprofen, naproxen, and celecoxib cause 44% of drug-induced AIN cases. These are especially dangerous for older adults or people with existing kidney issues. Unlike antibiotics, NSAID-induced AIN rarely causes a rash or fever. Instead, you get heavy protein in your urine-sometimes enough to look like nephrotic syndrome. Recovery is slower, and damage is more likely to stick around.
What’s surprising? PPIs cause less dramatic symptoms than antibiotics, but they’re more likely to leave lasting damage. Only 50-60% of people fully recover from PPI-induced AIN. With antibiotics, it’s 70-80%. That’s a big difference-and it’s why stopping the drug early is so critical.
Why Diagnosis Is So Hard (And Why It’s Often Too Late)
There’s no blood test that confirms AIN. No quick scan. No simple urine dipstick. The only way to be sure is a kidney biopsy. That’s invasive. That’s scary. So doctors often wait-until kidney function is dangerously low.
Patients typically wait 2 to 4 weeks before getting the right diagnosis. Why? Because the symptoms are vague. Fatigue? Common. Nausea? Everyone gets that. Reduced urine output? Maybe you’re just not drinking enough. Many are misdiagnosed with a UTI, especially if they have cloudy urine or mild pain.
Even the classic signs-rash, fever, eosinophilia-are rare. Less than 10% of cases show the full triad. But here’s what’s more common: eosinophils in the urine (eosinophiluria). It’s a clue, but most labs don’t test for it routinely. And 67-gallium scans? They’re outdated and unreliable.
Dr. David Jayne from the University of Cambridge says it plainly: “Early recognition is crucial because patients can ultimately develop chronic kidney disease if AIN is not diagnosed promptly.” That’s not hyperbole. If you wait more than 14 days after symptoms start, your chance of full recovery drops by 35%.
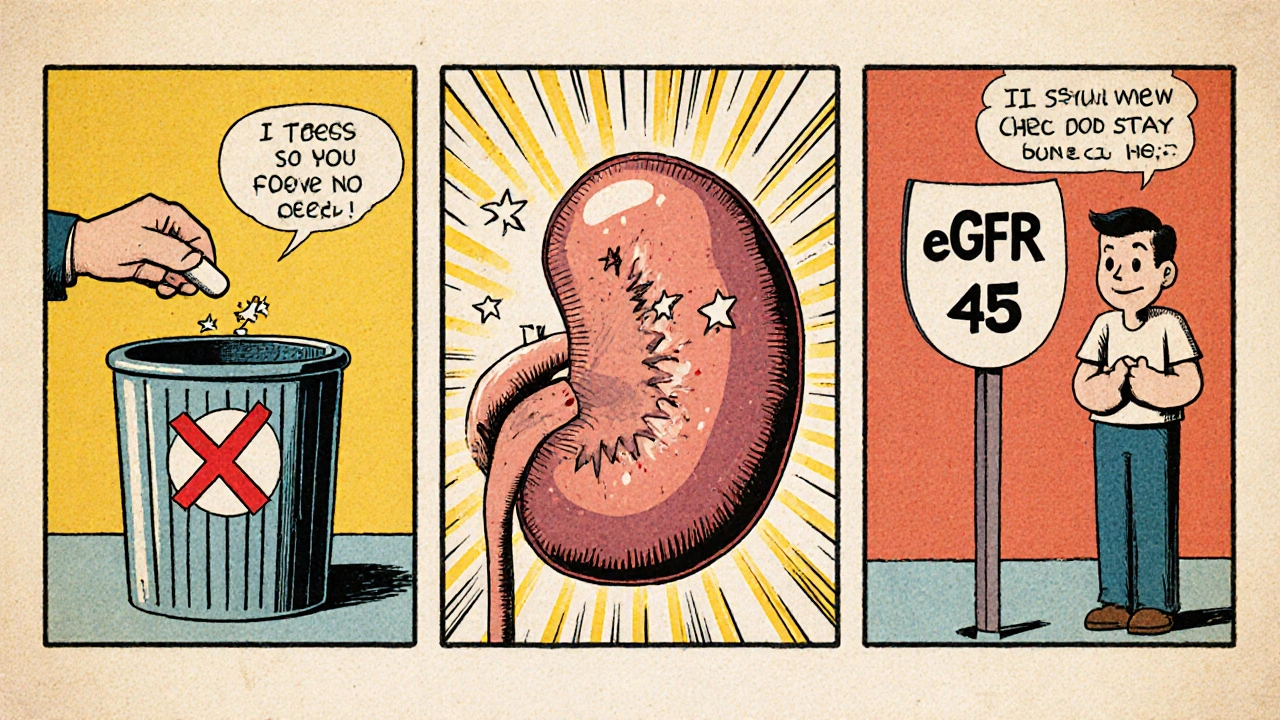
What Happens After You Stop the Drug?
The single most important step? Stop the drug. Immediately. No waiting. No “let’s monitor for a week.” If your doctor suspects AIN, the medication must go within 24 to 48 hours.
Most people start feeling better within 72 hours after stopping the trigger. One Medscape survey of 120 patients found 65% improved noticeably in just three days. But improvement doesn’t mean recovery. Kidney healing takes time.
- Antibiotic-induced AIN: Median recovery time is 14 days.
- NSAID-induced AIN: Takes about 28 days.
- PPI-induced AIN: Takes 35 days on average.
But here’s the hard truth: 42% of patients in that same survey still had reduced kidney function (eGFR below 60) six months later. That’s chronic kidney disease stage 3 or worse. And NSAID users? They’re the most likely to end up there-42% progress to lasting damage.
One case from the American Kidney Fund tells the story: a 63-year-old woman took omeprazole for 18 months. When she developed AIN, her kidneys were so damaged she needed dialysis for three weeks. Even after recovery, her eGFR stayed at 45-down from a normal 90. She’ll live with reduced kidney function for the rest of her life.
Do Steroids Help? The Controversy Explained
This is where things get messy. Should you take steroids? The answer isn’t clear-cut.
No large randomized trials prove corticosteroids work for AIN. But real-world data says they might. Dr. Ronald J. Falk from UNC Kidney Center says: “Although benefits remain unproven in randomized controlled trials, corticosteroids appear to improve outcomes when initiated early, particularly in severe cases.”
So when do doctors use them? Usually if:
- Your eGFR is below 30 (severe kidney impairment)
- Your kidney function keeps dropping after 72 hours of stopping the drug
- You have signs of heavy inflammation on biopsy
The typical dose? Methylprednisolone (IV) at 0.5-1 mg/kg per day for 2-4 weeks, then switched to oral prednisone and slowly tapered over 6-8 weeks. It’s not a cure. But for severe cases, it can mean the difference between dialysis and recovery.
Who’s at Highest Risk?
AIN doesn’t care about your fitness level or diet. It cares about your age, your meds, and how long you’ve been taking them.
- Age 65+: Risk jumps from 5 cases per 100,000 in people under 45 to 22 cases per 100,000 in those over 65.
- Taking 5 or more medications: Your risk triples. Polypharmacy is a silent killer here.
- Chronic kidney disease already: Even small insults can push you over the edge.
- Long-term PPI use: The longer you’re on them, the higher the risk-even if you feel fine.
And here’s a growing concern: immune checkpoint inhibitors-cancer drugs like pembrolizumab-are emerging as new triggers. These are powerful drugs that turn the immune system against tumors. But sometimes, they turn it against the kidneys too. These cases are rarer, but harder to treat.
What Does Recovery Really Look Like?
Let’s be honest: recovery isn’t guaranteed. Even if your creatinine drops back to normal, your kidneys may never fully heal.
Studies show:
- 70-80% of patients regain partial kidney function
- Only 50-60% recover completely
- 30% develop chronic kidney disease within a year
- NSAID-induced cases have the highest rate of permanent damage
And the damage isn’t just physical. It’s emotional. People on Reddit’s r/kidneydisease talk about the fear of never knowing if their kidneys will bounce back. They worry about future meds, about needing dialysis, about becoming a burden.
The best outcome? Catch it early. Stop the drug fast. Get a biopsy if needed. Don’t wait for the classic signs. Don’t assume it’s just a UTI. If you’ve been on a PPI for over a year and your creatinine is creeping up-ask your doctor about AIN.
What You Can Do Now
You don’t need to panic. But you do need to be aware.
- If you’re on a PPI for more than 6 months, ask your doctor if you still need it. Many people take them long after they’re necessary.
- Track your kidney function. If you’re on multiple medications, get a basic blood test (creatinine, eGFR) at least once a year.
- Don’t ignore fatigue, nausea, or reduced urine output-especially if you’ve started a new drug recently.
- Keep a list of all your meds-including OTCs and supplements. Bring it to every appointment.
- If you’re diagnosed with AIN, don’t just stop the drug. Ask for a biopsy to confirm. And ask about steroids if your kidney function is low.
AIN isn’t a death sentence. But it’s a warning. A signal that your body is reacting to something you thought was harmless. The sooner you act, the better your kidneys will be in five years. And that’s worth paying attention to.
Can you get acute interstitial nephritis from over-the-counter painkillers?
Yes. NSAIDs like ibuprofen, naproxen, and aspirin are among the top causes of drug-induced AIN. They account for 44% of cases. The risk is higher in older adults, people with existing kidney problems, or those taking them long-term. Even short-term use can trigger it in sensitive individuals.
How long does it take for kidneys to recover after stopping the drug?
Recovery time depends on the drug. Antibiotic-induced AIN usually improves in about 14 days. NSAID-induced cases take around 28 days. PPI-induced AIN takes the longest-often 35 days or more. But improvement doesn’t mean full recovery. Some people never regain their original kidney function, especially if diagnosis was delayed.
Do I need a kidney biopsy to diagnose AIN?
Yes. While blood and urine tests can suggest AIN, only a kidney biopsy can confirm it. Other tests like eosinophiluria or gallium scans are unreliable. A biopsy shows the inflammation, immune cells, and tissue damage that define AIN. It’s the only way to rule out other kidney diseases and guide treatment.
Are proton pump inhibitors safe for long-term use?
Long-term PPI use carries risks, including AIN, bone fractures, and nutrient deficiencies. The FDA has warned about AIN risk since 2021, with over 1,200 reported cases between 2011 and 2020. If you’ve been on a PPI for more than a year, ask your doctor if you still need it. Many people take them far longer than necessary.
Can acute interstitial nephritis come back after recovery?
Yes-if you take the same drug again. Once your immune system has reacted to a medication, it’s more likely to react again. Avoid all drugs that triggered AIN in the past. Even similar drugs in the same class (like switching from omeprazole to lansoprazole) can cause a relapse. Always inform new doctors about your history of AIN.


Comments
Bro, I was on omeprazole for 3 years thinking it was harmless. Then my creatinine jumped from 1.1 to 2.4 overnight. No fever, no rash, just pure exhaustion. Docs called it 'dehydration' for 6 weeks. Finally, a nephrologist said 'stop the PPI' - and boom, biopsy confirmed AIN. I'm lucky I didn't end up on dialysis. PPIs are not vitamins. They're stealth killers.
Typical American overmedication. People take PPIs like candy. In India, we only use them for 2 weeks max. No one thinks they're 'safe'.
I just want to say - this is so important, and I'm so glad someone took the time to lay this out clearly. I've seen friends go through this, and it's terrifying how easily it's missed. I mean, think about it: we’re told to take heartburn meds 'as needed' - but then we end up on them for years because it's just easier than changing diet or lifestyle. And the kidneys? They don't scream. They whisper. Until it's too late. And then you're stuck with a 45 eGFR and a lifetime of caution. It's not just medical negligence - it's systemic. We're trained to treat symptoms, not root causes. And that's why so many of us are walking around with silent organ damage.
When I was in medical school in Mumbai, we were taught: 'If you don't know what it is, stop the drug.' But here in the West, it's like everyone's on 12 pills a day. I had a cousin in Texas - took ibuprofen daily for back pain, didn't know it could wreck kidneys. Now he's on meds for CKD. It's not the medicine that's bad - it's the culture of 'pop it and forget it.' We've lost the art of listening to our bodies.
You’re not alone. I had AIN from naproxen after a sports injury. Thought it was just soreness. Turns out my kidneys were crying for help. Stopped the drug, got steroids, and slowly came back. It took 6 months, but I’m at 80% now. Don’t ignore fatigue. Don’t assume it’s stress. Your kidneys are working 24/7 - show them some respect.
omg i took pantoprazole for 5 years and now i have kidney issues?? i thought it was just aging lol
It's funny how we fear cancer drugs but trust a $2 bottle of antacids. The body doesn't care if it's 'prescription' or 'OTC.' It reacts to chemistry. And we're just now realizing how many of these drugs are slow-motion poison. The real tragedy? The people who die from this never even knew they were at risk. We need warning labels that scream, not whisper.
While I appreciate the anecdotal evidence presented, it is imperative to note that the absence of randomized controlled trials validating corticosteroid efficacy in AIN renders clinical recommendations speculative at best. Furthermore, the conflation of correlation with causation in the context of PPI usage and renal decline is a well-documented epidemiological pitfall. One must exercise extreme caution before attributing renal dysfunction solely to pharmaceutical agents without ruling out confounding variables such as age-related decline, comorbid hypertension, or undiagnosed glomerulonephritis.
Man, this hit hard. My uncle died because they didn’t catch AIN in time. He was on ibuprofen for arthritis - thought it was fine. Then one day he just... stopped waking up. Autopsy showed massive interstitial damage. I started asking every doctor I meet: 'Have you checked for AIN?' Now I tell everyone I know: if you're on meds longer than 6 months, get your kidneys checked. Don't wait for the crash. Your kidneys don't text you. They just... stop.
I’ve been reading this whole thing and I just… I don’t know what to feel. I’ve been on omeprazole since 2019. I thought it was keeping me healthy. Now I’m scared. But also… I feel so stupid for not asking sooner. I’m going to the doctor tomorrow. I’m going to get a creatinine test. And I’m going to stop the PPI. Not because I’m scared - because I owe it to my body to try. Thank you for writing this. I needed to hear it.
Of course this is happening. America’s addicted to quick fixes. We don’t want to change our diet, we don’t want to sleep better, we don’t want to walk more - so we pop a pill. And then we blame the medicine when it breaks our kidneys. It’s not the drug. It’s the laziness. The entitlement. The refusal to live like a human being.
Let’s not forget: NSAIDs are also linked to GI bleeds, heart attacks, and liver damage. PPIs? Linked to C. diff, pneumonia, dementia, and now AIN. We’re in an era of polypharmacy where every drug is a band-aid on a bullet wound. The real question isn’t ‘which drug caused it?’ - it’s ‘why are we prescribing so many drugs to fix problems we created with our lifestyles?’
And yes - if you’ve had AIN once, never touch that class of drugs again. Even if it’s ‘different.’ Your immune system remembers. And it doesn’t forgive.