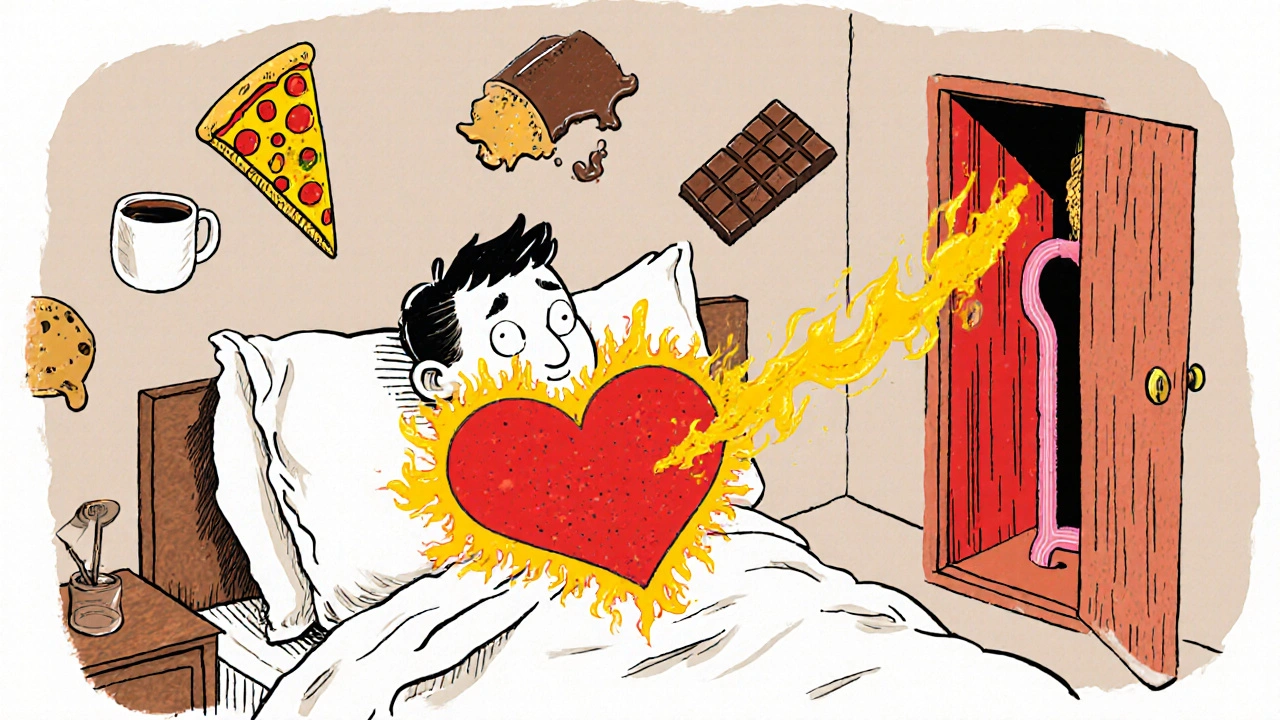
If you’ve ever woken up with a burning chest or a sour taste in your mouth, you’re not alone. About 20% of adults in the U.S. deal with GERD symptoms at least once a week. For many, it starts as occasional heartburn after spicy food or late-night pizza. But when it happens twice a week or more, it’s not just discomfort-it’s gastroesophageal reflux disease, or GERD. And while proton pump inhibitors (PPIs) like omeprazole and esomeprazole can bring quick relief, they’re not a long-term fix. The real key to managing GERD lies in combining medication with real, sustainable lifestyle changes.
What Actually Happens in GERD?
GERD isn’t just "too much stomach acid." It’s a broken valve. The lower esophageal sphincter (LES), a ring of muscle between your stomach and esophagus, should stay closed except when food passes through. In GERD, it relaxes too often or doesn’t close tightly enough. That lets stomach acid-strong enough to dissolve metal-creep up into your esophagus. Your stomach lining can handle it. Your esophagus can’t. That’s what causes the burn, the regurgitation, and the long-term damage.Common symptoms? Heartburn (felt by 90% of people with GERD), a sour or bitter taste, chronic cough, hoarseness, and even tooth erosion. Symptoms often get worse after eating, lying down, or bending over. Some people don’t even feel heartburn-they just have a persistent cough or sore throat, which doctors sometimes miss.
It’s not just about what you eat. Risk factors like obesity (BMI over 30 raises your risk 2.5 times), smoking, hiatal hernia, and certain medications (like calcium channel blockers for blood pressure) all play a role. Pregnancy triggers GERD in 30-50% of women. And if left untreated, GERD can lead to Barrett’s esophagus-a precancerous condition that develops in 10-15% of long-term sufferers.
How PPIs Work (and Why They’re Overused)
Proton pump inhibitors (PPIs) are the most powerful acid-reducing drugs available. They work by shutting down the acid-producing pumps in your stomach lining. Unlike antacids (which neutralize acid temporarily) or H2 blockers (which reduce acid by about 60-70%), PPIs cut production by 90-98%. That’s why they heal erosive esophagitis in 70-90% of cases-far better than H2 blockers.But here’s the catch: PPIs don’t fix the broken valve. They just mask the symptoms. And that’s led to massive overuse. About 70% of GERD patients are prescribed PPIs, and 15% take them for more than a year-even though guidelines say to reevaluate after 8 weeks. In Australia, where I live, PPI prescriptions have doubled since 2010. Many people take them "just in case," or because their doctor never asked if they still needed them.
Long-term use comes with real risks. Studies show prolonged PPI use (over a year) increases the chance of:
- Enteric infections like C. difficile by 20-50%
- Vitamin B12 deficiency (especially in older adults)
- Low magnesium levels, which can cause muscle cramps or irregular heartbeat
- Acute interstitial nephritis (a type of kidney inflammation)
- 35% higher risk of hip fractures in adults over 50 who take high doses for 3+ years
The FDA has issued warnings on all these. And when people stop PPIs cold turkey, up to 44% experience rebound acid hypersecretion-where the stomach overproduces acid for weeks, making symptoms worse than before. That’s why many think they "need" the drug forever.
Lifestyle Changes: The Real First-Line Treatment
The American College of Gastroenterology says lifestyle changes should come first-for everyone. Not as a backup. Not as a supplement. As the foundation.Here’s what actually works, backed by clinical data:
- Weight loss: Losing just 5-10% of your body weight cuts GERD symptoms by 50%. For someone weighing 200 lbs, that’s 10-20 lbs. It reduces pressure on the stomach and helps the LES close properly.
- No eating 2-3 hours before bed: Lying down lets acid flow easily into the esophagus. Avoiding late meals reduces nighttime acid exposure by 40-60%.
- Eliminate trigger foods: Coffee, tomatoes, alcohol, chocolate, fatty foods, and spicy meals worsen symptoms in 70-80% of people. Cutting coffee alone helps 73% of users. You don’t need to eliminate everything at once-track your triggers with a food diary for two weeks.
- Elevate the head of your bed: Raising the head by 6-8 inches (using blocks or a wedge pillow) uses gravity to keep acid down. One patient in Perth told me this single change ended his nighttime cough completely.
- Quit smoking: Smoking relaxes the LES and reduces saliva production (which helps neutralize acid). It doubles your GERD risk.
These aren’t "nice to haves." They’re medical interventions. A 2023 Johns Hopkins study found that a 12-week structured program of diet and lifestyle changes allowed 65% of patients to stop PPIs entirely-without symptom return. That’s more effective than most drugs.
Why Lifestyle Changes Are Hard (and How to Make Them Stick)
Let’s be honest: giving up pizza, wine, or late-night snacks is tough. Especially if you’re social, busy, or used to eating on the run. That’s why 41% of patients in a Cleveland Clinic survey couldn’t stick with lifestyle changes long-term.Here’s how to make it work:
- Start small: Pick one change-say, no food after 7 p.m.-and stick with it for two weeks. Then add another.
- Plan ahead: If you’re going out to dinner, eat a light lunch. Order grilled chicken instead of fried. Ask for sauces on the side.
- Use tech: Apps like RefluxMD (rated 4.7/5 by 8,500 users) help track meals, symptoms, and triggers. You’ll quickly see patterns-like how red wine triggers your cough but white wine doesn’t.
- Don’t go it alone: Talk to a dietitian who specializes in GI health. Many public hospitals in Australia offer free or low-cost nutrition counseling.
And remember: healing takes time. You might feel better in days on a PPI. But healing the esophagus? That takes 8-12 weeks of consistent lifestyle changes. Don’t mistake symptom relief for cure.
When to Use PPIs-and How to Use Them Right
PPIs have a place. If you have confirmed erosive esophagitis, severe symptoms, or complications like Barrett’s esophagus, they’re life-changing. But they should be used smartly.Here’s the right way:
- Take it 30-60 minutes before your first meal. That’s when acid pumps activate. Taking it after eating? It’s less effective.
- Use the lowest dose possible. Many people take 40 mg daily when 20 mg is enough. Ask your doctor if you can step down.
- Don’t stay on them longer than needed. After 4-8 weeks, try to taper off. Don’t quit cold turkey. Switch to an H2 blocker like famotidine for a week, then reduce frequency.
- Get checked if you’re on them long-term. Ask your doctor for a B12 and magnesium blood test yearly.
Newer drugs like vonoprazan (Voquezna), approved in 2023, offer faster, stronger acid control with potentially fewer side effects. But they’re not magic-they still don’t fix the valve. Lifestyle changes still matter.
What to Do If Your Symptoms Don’t Improve
If you’ve tried PPIs and lifestyle changes for 8-12 weeks and still have symptoms, it’s time to dig deeper. You might have:- A hiatal hernia (present in 94% of people with erosive esophagitis)
- Non-acid reflux (bile or gas, not acid)
- A different condition like eosinophilic esophagitis or gastroparesis
See a gastroenterologist if you have:
- Difficulty swallowing
- Unexplained weight loss
- Bloody or black stools
- Choking or vomiting
These aren’t "just GERD." They’re red flags.
Surgery is an option for those who don’t respond to meds. Fundoplication (wrapping the stomach around the esophagus) has a 90% success rate at 10 years. Newer options like the LINX® device (a magnetic ring around the LES) or TIF (transoral incisionless fundoplication) offer less invasive alternatives with 85%+ patient satisfaction.
Final Thought: It’s Not Either/Or
You don’t have to choose between PPIs and lifestyle changes. You need both-temporarily. Use PPIs to heal the damage. Use lifestyle changes to stop it from coming back. Most people can get off PPIs completely if they commit to the habits. But if you skip the lifestyle part, you’ll be back on them in six months.GERD isn’t a life sentence. It’s a signal. Your body is telling you something’s off. Fix the valve, not just the acid.
Can I stop PPIs cold turkey?
No. Stopping PPIs suddenly can cause rebound acid hypersecretion, making heartburn worse for weeks. Instead, work with your doctor to taper off slowly-usually over 4-8 weeks-while switching to an H2 blocker like famotidine or using on-demand antacids.
Are PPIs safe for long-term use?
PPIs are safe for short-term use (4-8 weeks), but long-term use (over a year) increases risks like kidney problems, vitamin B12 deficiency, low magnesium, and bone fractures. Regular check-ups and periodic reevaluation are essential. Never take them "just in case."
What foods should I avoid for GERD?
Common triggers include coffee, alcohol, tomatoes, chocolate, fatty or fried foods, spicy foods, citrus, and carbonated drinks. But triggers vary. Keep a food diary for two weeks to find your personal list. Many people find cutting out coffee alone makes a big difference.
Can weight loss really fix GERD?
Yes. Losing just 5-10% of your body weight reduces GERD symptoms by half. Excess belly fat puts pressure on the stomach, forcing acid upward. Weight loss helps the lower esophageal sphincter close properly again. It’s one of the most effective treatments available.
Is surgery worth considering?
Surgery is an option if medications and lifestyle changes don’t work, or if you want to avoid lifelong PPI use. Procedures like fundoplication or LINX® have high success rates (85-90%) and improve quality of life for most patients. But they’re not for everyone-discuss risks and benefits with a specialist.
Do I need an endoscopy for GERD?
Not always. If you have typical symptoms like heartburn and regurgitation without warning signs (weight loss, trouble swallowing, bleeding), doctors often use a "test-and-treat" approach with PPIs first. But if symptoms persist after 8 weeks, or if you’re over 50 with new-onset symptoms, an endoscopy is recommended to check for damage or Barrett’s esophagus.




Comments
Let’s be real-PPIs are the pharmaceutical equivalent of duct tape on a leaking pipe. They stop the drip for a while, but the pipe’s still busted. The real win? Losing 10% body weight. I dropped 22 lbs last year, stopped my omeprazole cold (after tapering, thank god), and haven’t had a single night cough since. No magic, just physics-less belly fat = less pressure on the LES. Simple as that.
Also, coffee isn’t the villain-it’s the *timing*. I still drink it, but never after 11 a.m. and never on an empty stomach. Game changer.
Yall are so gullible. PPIs are safe. The FDA? Big Pharma shills. They want you scared so you’ll buy their ‘lifestyle’ apps and $200 ‘GERD diet’ ebooks. I’ve been on Nexium for 8 years. My B12? Fine. My kidneys? Perfect. My doctor says I’m fine. You think some random blog post from a ‘gastroenterologist’ in Australia knows more than my MD? Lol. Wake up.
Also, ‘elevate your bed’? That’s what pillows are for. Why are we paying for wedge pillows now? Next they’ll tell us to sleep in a hammock.
Big shoutout to the OP-this is the most balanced, science-backed take on GERD I’ve ever read. Seriously. I was on PPIs for 5 years after my diagnosis. Tapered off using famotidine + the 2-hour no-eating rule + bed elevation. Took 10 weeks, but now I’m symptom-free and off everything. No more midnight coughing. No more ‘is this heartburn or a heart attack?’ panic.
Also-get a RefluxMD app. I tracked my triggers for 2 weeks and found out red wine = cough, white wine = fine. Mind blown. 🙌
just stop eatin late and u be fine. i did it. no pills. no fancy pillows. just no pizza at midnight. easy. 🤙
It’s alarming how many people treat GERD as a trivial inconvenience rather than a chronic, potentially precancerous condition. The fact that 70% of patients are prescribed PPIs without ever being counseled on lifestyle modification is a systemic failure of primary care. Furthermore, the normalization of self-medication with over-the-counter PPIs is a public health crisis. If you’re taking them ‘just in case,’ you’re not managing your health-you’re enabling pharmaceutical dependency. Please consult a gastroenterologist before self-prescribing.
PPIs are overprescribed because doctors are lazy. You give someone a script and they’re happy. You tell them to lose weight and quit smoking? That’s work. I’ve seen it a hundred times. Guy comes in with heartburn, gets 40mg omeprazole, never comes back. Meanwhile his BMI is 38 and he smokes 2 packs a day. The system rewards quick fixes. The patient pays in kidney damage.
Also-bed elevation works. I used books under my mattress. No cost. No gimmicks. Just gravity. Try it before you buy a $100 wedge.
My mom had GERD for 15 years. Tried everything. Then she started walking 20 mins after dinner and stopped eating after 7. That’s it. No meds. No surgery. Just… movement and timing. It’s wild how simple it can be when you stop looking for a pill to fix it.
Also-don’t stress. You don’t have to be perfect. One bad night won’t ruin you.
As someone who grew up in the South with fried chicken and sweet tea every Sunday, I get it. GERD feels like a betrayal of your culture. But here’s the thing-your grandma didn’t live to 90 because she ate fried food at midnight. She lived because she moved, slept early, and didn’t have 20 types of processed snacks in her kitchen.
Changing your habits isn’t giving up your roots-it’s honoring them by staying alive to pass them down. I swapped fried chicken for grilled. Kept the collards. Kept the tea. Just moved it to lunch. Still feel like me. Just without the burn.
I started tracking everything after my doctor said I had mild esophagitis. I thought I was eating ‘healthy’-quinoa salads, avocado toast, almond milk. Turns out tomatoes in my salad and almond milk were my triggers. Who knew? I thought I was doing everything right.
Now I eat oatmeal for breakfast, grilled fish for lunch, and a banana with peanut butter before bed. No caffeine after noon. I still have wine once a week-just not with dinner. And I sleep with my head up. It’s not perfect, but I haven’t needed PPIs in 9 months. Progress, not perfection.
Also-why is everyone so obsessed with ‘curing’ GERD? It’s a lifestyle adjustment, not a disease to be eradicated. I’m not ‘fixed.’ I’m just managing it like I manage my blood pressure. No shame.
They don’t want you to know the truth. PPIs are a trap. The real cause? Glyphosate in your food. It’s in the wheat, the soy, the corn syrup. It’s destroying your gut lining. The FDA knows. The WHO knows. But they’re paid off by Monsanto. That’s why they push PPIs instead of telling you to eat organic. Your ‘trigger foods’? They’re not the problem. The chemicals are. Go to a naturopath. Get your heavy metals tested. You’re being lied to.
Also-your bed elevation? That’s just a distraction. The real fix is a bentonite clay cleanse. I did it. My reflux vanished in 3 days. No one talks about this because Big Pharma doesn’t sell clay.
Wow. Another ‘lifestyle change’ article from someone who clearly never had to work a 60-hour week, raise kids, and still eat dinner after 9 p.m. Let me guess-you’re a wellness influencer with a $200 ‘GERD reset’ course. Real helpful. I don’t have time to track food diaries or buy wedge pillows. I have a toddler and a boss who emails at midnight. So I take my pill. And I’m fine. Stop shaming people for surviving.
Also, ‘65% can stop PPIs’? Cool. What about the other 35%? The ones with jobs? The ones with anxiety? The ones who just need to sleep? You’re not helping. You’re just flexing.
bro ppi’s are fine. i take them every day. i eat pizza every night. i smoke. i drink. i sleep on my stomach. i’m fine. everyone else is just weak. stop overthinking. your body’s fine. just take the pill. it’s not that hard. 🤡
I just wanted to say thank you to everyone sharing their stories here. This thread actually made me feel less alone. I’ve been scared to stop my PPIs because I thought I’d be back to square one. But reading how others tapered slowly, tracked triggers, and still had wine on weekends? That gave me hope.
I’m starting with no food after 8 p.m. and cutting out coffee on weekends. Baby steps. And if I slip? I’ll try again tomorrow. You’re all doing better than you think.