Every year, millions of people take dietary supplements-vitamins, herbs, minerals, amino acids-thinking they’re harmless, even healthy. But what if those pills you’re swallowing with your morning coffee could make your blood thinner less effective, or cause your blood pressure medication to stop working? The truth is, dietary supplement-drug interactions are more common-and more dangerous-than most people realize.
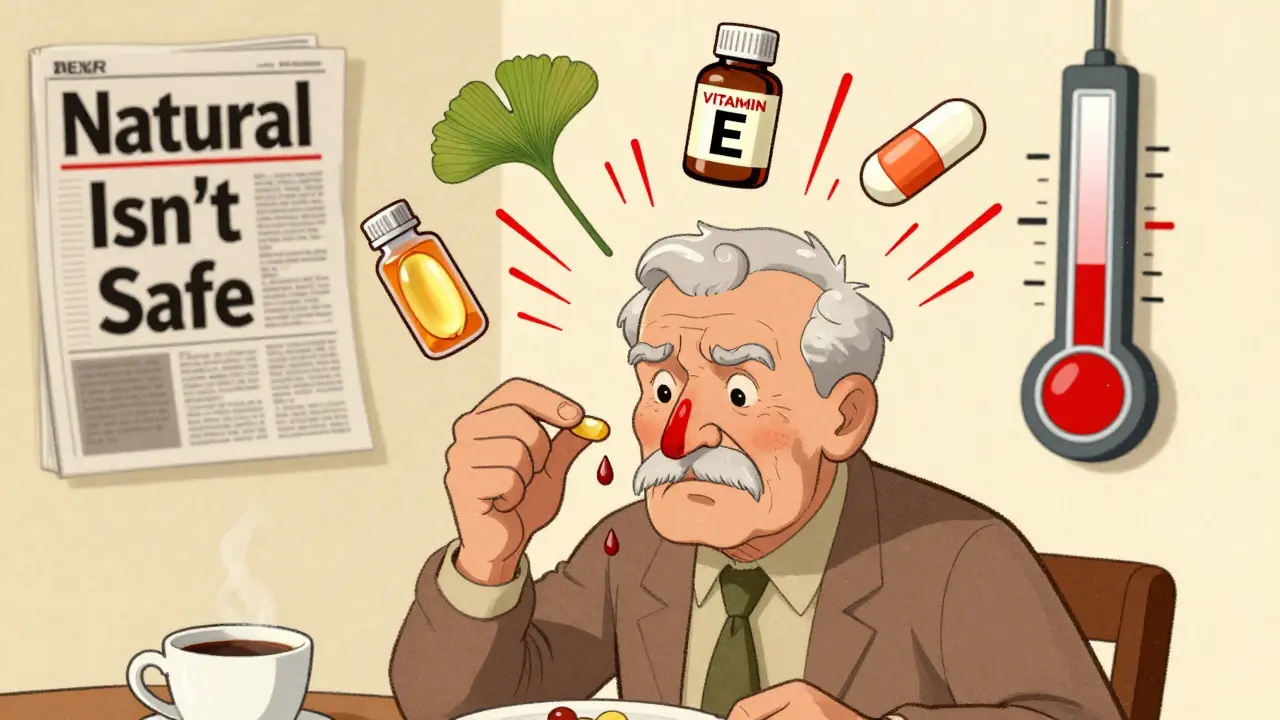
You might not think of fish oil or turmeric as drugs, but they act like them in your body. And when they mix with prescription meds, the results can be serious. Take warfarin, a common blood thinner. If you start taking ginkgo biloba or even high-dose vitamin E, your INR can spike into dangerous territory. One case in Pharmacotherapy showed a patient’s INR jumping from 3.1 to 6.8 after adding ginkgo. That’s not a typo. That’s a bleeding risk.
How Supplements and Drugs Actually Interact
These aren’t random accidents. They happen because of how your body processes chemicals. There are two main ways supplements interfere with medications:
- Pharmacokinetic interactions change how much of the drug gets into your bloodstream. This means your body might absorb less of the drug, or break it down too fast.
- Pharmacodynamic interactions change how the drug works once it’s in your system. The effect might get stronger, weaker, or even opposite.
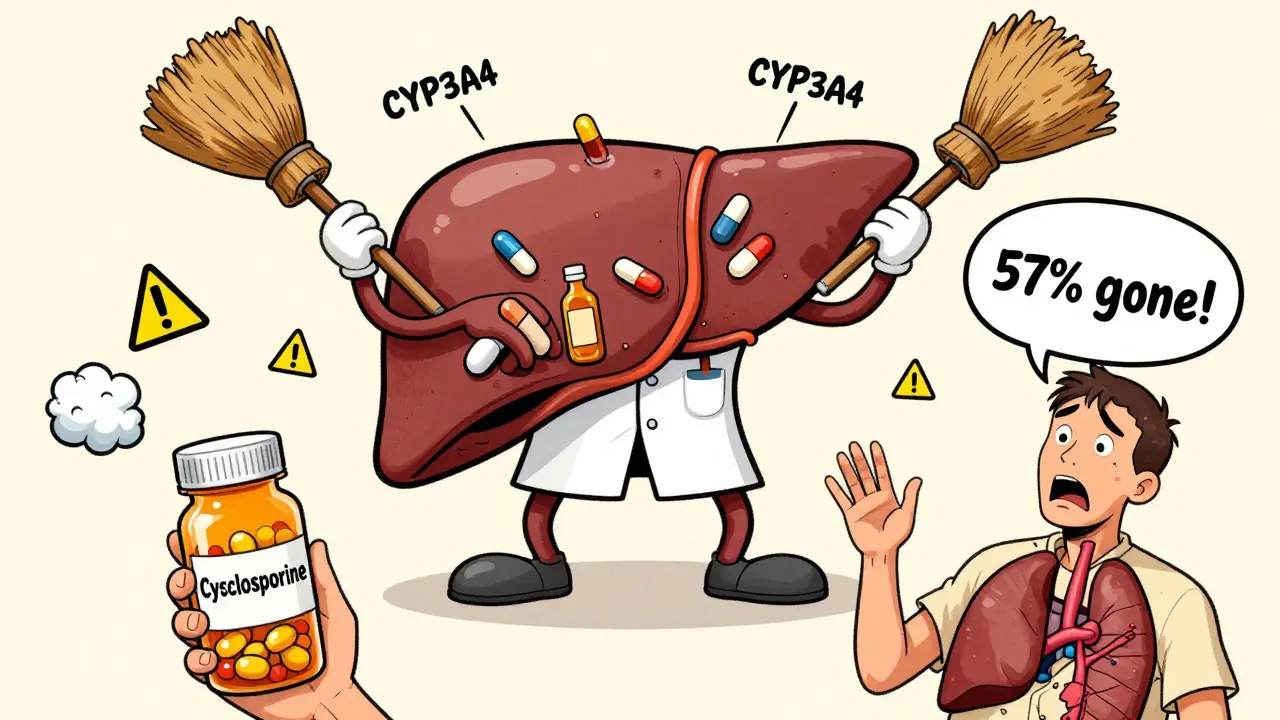
One of the biggest culprits? St. John’s wort. This popular herb for mood support triggers enzymes in your liver-specifically CYP3A4 and P-glycoprotein-that flush drugs out of your system before they can do their job. Studies show it can slash cyclosporine levels by 57%, making organ transplant patients vulnerable to rejection. It can drop indinavir (an HIV drug) by 54%. In one documented case, a woman on carbamazepine for seizures had her drug levels drop by more than half after starting St. John’s wort-and had a breakthrough seizure.
Then there’s vitamin K. If you’re on warfarin, your doctor carefully balances your dose based on how much vitamin K you eat. But if you start taking a daily vitamin K supplement-even one labeled “natural”-it can directly counteract the drug’s effect. Your blood won’t thin enough. Clots can form. Stroke risk goes up.
High-Risk Supplements and the Drugs They Clash With
Not all supplements are equal when it comes to danger. Some are quietly risky. Others are outright hazardous when mixed with common meds.
St. John’s wort - Interacts with over 80 medications. Includes antidepressants (SSRIs, SNRIs), birth control pills, statins, and immunosuppressants like cyclosporine. The Natural Medicines Database lists it as responsible for 30% of all clinically significant supplement-drug interactions.
Ginkgo biloba - Increases bleeding risk when taken with warfarin, aspirin, or NSAIDs like ibuprofen. Case reports show INR levels rising above 6.5, far beyond the safe range of 2-3.
Calcium supplements - Can reduce absorption of levothyroxine (thyroid medication) by 25-50%. One study showed patients needed a 30% higher dose of thyroid meds just to stay stable after starting calcium.
Magnesium antacids - Bind to antibiotics like ciprofloxacin and levofloxacin in the gut. One study found absorption dropped by up to 90%. Take them two hours apart-or skip the antacid altogether.
Cranberry - Often thought to be safe, but it can amplify the effect of warfarin. The mechanism isn’t fully understood, but enough cases have been reported that the FDA issued a warning in 2010.
CBD oil - A newer player, but a big one. CBD inhibits liver enzymes that break down many drugs. In epilepsy patients, it can raise clobazam levels by up to 500%. That’s not a minor tweak-it’s a potential overdose.
Why Doctors Don’t Always Know
You’d think your doctor would ask. But they rarely do. A 2018 study in Patient Education and Counseling found that 43-69% of patients never mention supplements during medical visits. Why? Many assume supplements are “natural,” so they’re safe. Others think doctors don’t care-or don’t know anything about them.
One Reddit user wrote: “My doctor doesn’t know anything about supplements anyway.” That’s the mindset that gets people hurt. Meanwhile, the FDA’s Bad Ad program received over 1,800 reports of supplement-drug interactions between 2019 and 2022. Of those, 32% involved warfarin, 24% involved antidepressants, and 18% involved immunosuppressants.
Even worse? Supplement labels rarely warn you. Dr. Paul Kemper of the NCCIH said in 2022 that 78% of supplement labels contain no interaction warnings-even though the risks are well-documented. You’re left guessing.
Who’s at the Highest Risk?
If you’re over 60, you’re in the danger zone. About 85% of older adults take supplements, and most are also on 4-5 prescription drugs. That’s a perfect storm for interactions.
People with chronic conditions are especially vulnerable:
- Heart disease patients on blood thinners
- Transplant recipients on immunosuppressants
- People with epilepsy on seizure meds
- Those with thyroid disorders on levothyroxine
- Patients with depression on SSRIs or SNRIs
And it’s not just about quantity-it’s about what’s in the bottle. A 2019 JAMA Internal Medicine study found that 20% of supplements contain unlisted ingredients. One supplement sold as “red yeast rice” was found to contain lovastatin-a prescription cholesterol drug. When taken with gemfibrozil, it caused rhabdomyolysis, a life-threatening muscle breakdown.
What You Can Do to Stay Safe
You don’t have to give up supplements. But you need to take control.
- Make a full list-Write down every pill, powder, capsule, or tea you take daily. Include brand names and doses. Don’t forget the “just in case” ones you only take occasionally.
- Bring it to every appointment-Show it to your doctor, pharmacist, or nurse. Don’t say “I take vitamins.” Say: “I take Nature Made Vitamin D 5000 IU, Ginkgo Biloba 120 mg, and Fish Oil 1000 mg.” Specificity matters.
- Ask directly-Say: “Could any of these interfere with my prescription meds?” Don’t wait for them to ask.
- Use trusted resources-Check the Natural Medicines Database or NIH’s LiverTox. These aren’t blogs-they’re clinical tools used by hospitals.
- Watch for warning signs-Unusual bruising, dizziness, fatigue, confusion, or sudden changes in how you feel could signal an interaction.
One study showed that when doctors routinely asked about supplements, 73% of them prevented potential harm. It’s that simple.
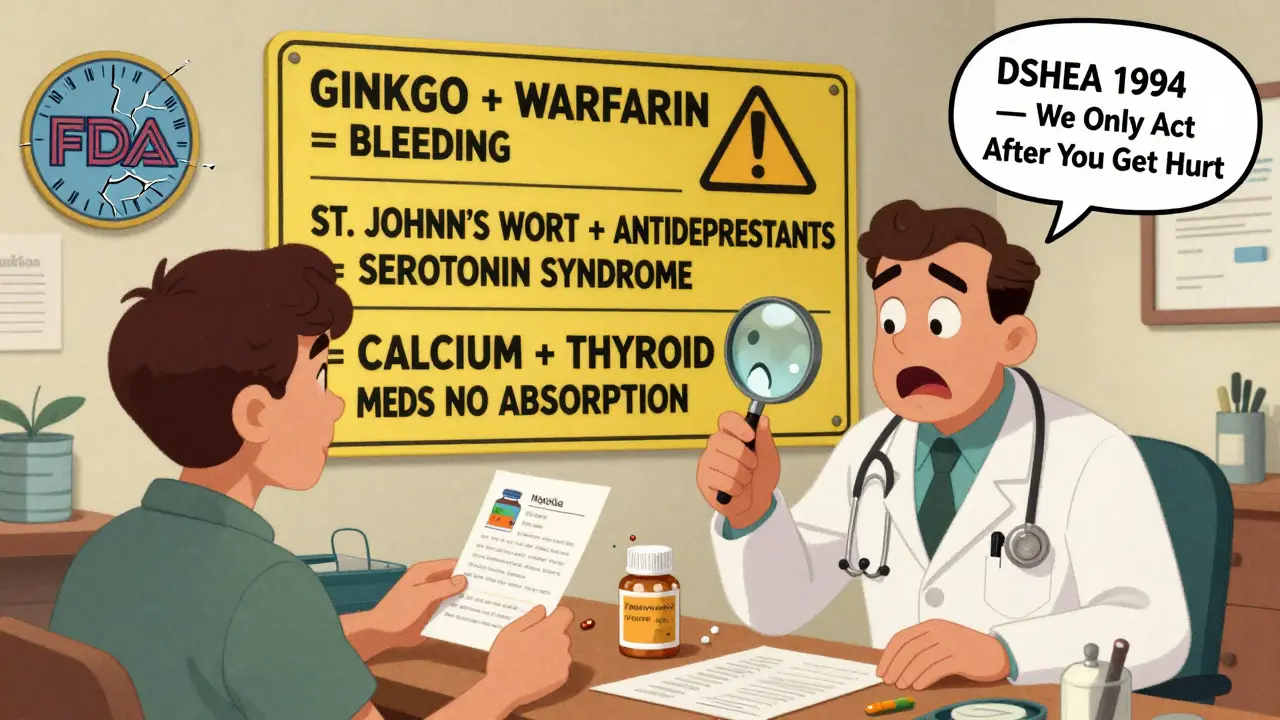
The Bigger Picture: Why Regulation Falls Short
The Dietary Supplement Health and Education Act (DSHEA) of 1994 lets companies sell supplements without proving they’re safe or effective. The FDA can only act after someone gets hurt. That’s backward. Prescription drugs go through years of testing. Supplements? They go straight to shelves.
The result? The U.S. supplement market hit $52 billion in 2022 and is projected to hit $82 billion by 2028. But only 0.5% of supplements have formal interaction studies published in peer-reviewed journals. Meanwhile, herbal supplements-just 15% of sales volume-account for 65% of serious adverse events reported to the FDA.
Proposals like the 2023 Dietary Supplement Labeling Act aim to fix this by requiring interaction warnings on high-risk products. But until then, the burden is on you.
Final Thought: Natural Doesn’t Mean Safe
Just because something comes from a plant doesn’t mean it’s harmless. Willow bark contains salicin-the same compound as aspirin. Foxglove contains digitalis-a powerful heart drug. Nature didn’t design these plants to be safe for humans. They evolved to defend against insects and animals.
Supplements aren’t candy. They’re bioactive compounds with real, measurable effects on your body. And when you mix them with prescription drugs, you’re playing with fire.
Don’t assume your doctor knows. Don’t assume the label tells you everything. Don’t assume “natural” means safe. Take charge. Talk. List. Ask. Protect yourself.
Can I take vitamin D with my blood pressure medication?
Yes, vitamin D generally doesn’t interfere with common blood pressure medications like ACE inhibitors, beta-blockers, or calcium channel blockers. However, if you’re taking thiazide diuretics, high doses of vitamin D could raise calcium levels too much, increasing the risk of kidney stones. Always check with your doctor before starting high-dose supplements, especially if you have kidney issues.
Is it safe to take turmeric with aspirin?
It’s risky. Turmeric contains curcumin, which has mild blood-thinning properties. When combined with aspirin, the risk of bleeding increases. There’s no clear safe dose, and studies are limited. If you’re on daily aspirin for heart protection, avoid high-dose turmeric supplements. A small amount in food is usually fine, but don’t take capsules or extracts without talking to your doctor.
Why doesn’t my pharmacist warn me about supplement interactions?
Many pharmacies don’t have access to reliable, updated interaction databases for supplements. Unlike prescription drugs, supplements aren’t tracked in standard pharmacy systems. Even when they are, the data is incomplete. Pharmacists often don’t know what’s in your supplement bottle, especially if it’s a lesser-known brand. That’s why you need to bring your list and ask.
Can herbal supplements affect my antidepressants?
Yes, and it can be life-threatening. St. John’s wort is the most dangerous-it can cause serotonin syndrome when mixed with SSRIs or SNRIs. Symptoms include agitation, rapid heart rate, high blood pressure, confusion, and seizures. Even 5-HTP, a supplement marketed for mood support, can increase serotonin levels. Never combine these without medical supervision.
Are there any supplements that are generally safe with most medications?
Some have low interaction risk when taken at standard doses: vitamin C, vitamin B12, magnesium (unless you have kidney disease), and zinc (in moderation). But “low risk” doesn’t mean “no risk.” Always disclose everything to your provider. Even safe supplements can become problematic at high doses or if you have underlying conditions.
What should I do if I think a supplement is interacting with my drug?
Stop taking the supplement immediately and contact your doctor or pharmacist. Don’t wait for symptoms to get worse. If you’re having chest pain, unusual bleeding, confusion, or severe dizziness, go to the emergency room. Report the incident to the FDA’s MedWatch program-it helps track these problems and protect others.




Comments
Bro, I took ginkgo with my blood thinner and thought I was being ‘natural’-turns out I almost bled out in the shower. My wife found me pale as a ghost. Don’t be me. Stop being dumb with supplements.
The epistemological failure of DSHEA is not merely regulatory-it is ontological. We have surrendered the integrity of pharmacological discourse to the mythos of ‘naturalness,’ a semiotic construct that obfuscates biochemical reality. The body does not distinguish between ‘drug’ and ‘supplement’; it responds to molecular structure, not marketing copy.
Willow bark is aspirin. Foxglove is digoxin. To call them ‘herbs’ is to veil toxicity in the language of innocence. We are not stewards of health-we are participants in a grand, unregulated pharmacopeia of ignorance.
Umm hello?? This is why I don’t trust doctors. They don’t even know what’s in my vitamin bottle but they wanna tell me what to take? Plus, all this ‘danger’ stuff is just Big Pharma scare tactics to keep you buying their expensive pills. Natural stuff has been used for centuries. You think ancient Egyptians were dumb?
And why is CBD such a big deal? It’s just plant juice. People are losing their minds over nothing.
My grandma takes turmeric for her knees and warfarin for her AFib. She’s 82. Never had a problem. Maybe it’s just about dose? I’d just ask my pharmacist before I freak out.
Interesting breakdown. I’d be curious to see the pharmacokinetic data on calcium and levothyroxine-specifically, what’s the half-life difference between taking them together vs. 4 hours apart? The 25-50% absorption drop sounds dramatic, but is it linear? Are there studies with TSH tracking over 12 weeks?
Also, is the 20% unlisted ingredient stat from the JAMA study corrected for adulteration in low-quality brands vs. high-end ones? That could skew the risk profile.
Let’s be clear: this is a textbook case of confirmation bias masquerading as public health guidance. The FDA’s Bad Ad program? 1,800 reports over three years? That’s 0.0005% of supplement users. Meanwhile, 40% of Americans take statins, and we don’t hear about the 20,000+ rhabdomyolysis cases annually from those. Why is the supplement industry the villain here?
Also, ‘natural doesn’t mean safe’? Then why are we still recommending ‘natural’ diets? Why is ‘natural childbirth’ a thing? You’re cherry-picking your scare tactics.
As someone who studied pharmacology at Oxford and now runs a clinical research lab, I must say: this article is dangerously oversimplified. The CYP3A4 inhibition by St. John’s wort is well-documented, yes-but the clinical significance varies by genotype. Poor metabolizers may not experience the same drop in cyclosporine levels. Also, most supplement studies are underpowered, observational, and funded by anti-supplement NGOs.
Furthermore, the FDA doesn’t ‘only act after someone gets hurt’-they issue warning letters, seize products, and initiate recalls. But you won’t hear about that because it doesn’t fit the narrative.
And let’s not forget: 80% of pharmaceuticals are derived from natural sources. Penicillin. Morphine. Taxol. Are you suggesting we ban trees?
They're watching us. The FDA, the pharmaceutical companies, the doctors-they all want you to stay sick so you keep buying their pills. Supplements are the only thing keeping people alive without being hooked on poison. They don't want you to know about the real dangers. The real danger is the system. They don't want you to be healthy. They want you dependent. I stopped taking all my meds and now I'm fine. They can't control me anymore.
Finally, someone who understands that ‘natural’ is a marketing term, not a scientific one. The FDA’s inability to regulate supplements is a catastrophic failure of governance. But this article misses the bigger point: the problem isn’t just supplement-drug interactions-it’s the complete absence of standardized labeling, batch testing, and bioavailability reporting.
Until supplements are held to the same standards as pharmaceuticals-active ingredient concentration, third-party verification, interaction disclosures-we’re all just gambling with our biology.
I’m a pharmacist in rural Tennessee, and I see this every day. An elderly woman comes in with 14 supplements-some in unlabeled jars-and says, ‘My cousin said this one helps her arthritis.’ I don’t judge. I just ask: ‘Can I see the bottle?’ Then we sit down, look at the ingredients, and cross-reference them with her meds.
One time, a man was taking St. John’s wort with his SSRI and didn’t realize he was on the edge of serotonin syndrome. We caught it before he ended up in the ER. He cried and said, ‘No one ever asked.’
That’s the real takeaway: it’s not about fear. It’s about conversation. Bring your list. Show your bottles. Ask the question. We’re here to help-not to shame you for wanting to feel better.
Let’s not forget-this is all part of the globalist agenda to control your health. Supplements are freedom. Big Pharma is a cartel. The FDA? A puppet. They ban turmeric in Europe because it competes with their blood thinners. They silence research on CBD because it kills profits. And now they want you to trust a doctor who went to medical school funded by pharmaceutical grants? Please.
Also, vitamin D doesn’t interact with anything-unless you’re one of those weak, pill-popping zombies who can’t handle sunlight. Go outside. Eat real food. Stop trusting the system.