Personalized Dosing Guide
This tool helps you understand how factors like age, weight, kidney function, and other medications might influence your dose. It does NOT replace medical advice. Always consult your doctor before changing any medication.
Dosing Factors Calculator
Results
Getting the right dose of medication isn’t just about following the label. It’s about finding the sweet spot where the drug works without hurting you. Too little, and it does nothing. Too much, and you risk serious side effects-or worse. For some drugs, the line between healing and harm is razor-thin. This is especially true for medication dose adjustment, where small changes can make a big difference in how you feel-and how safe you are.
Why One Size Doesn’t Fit All
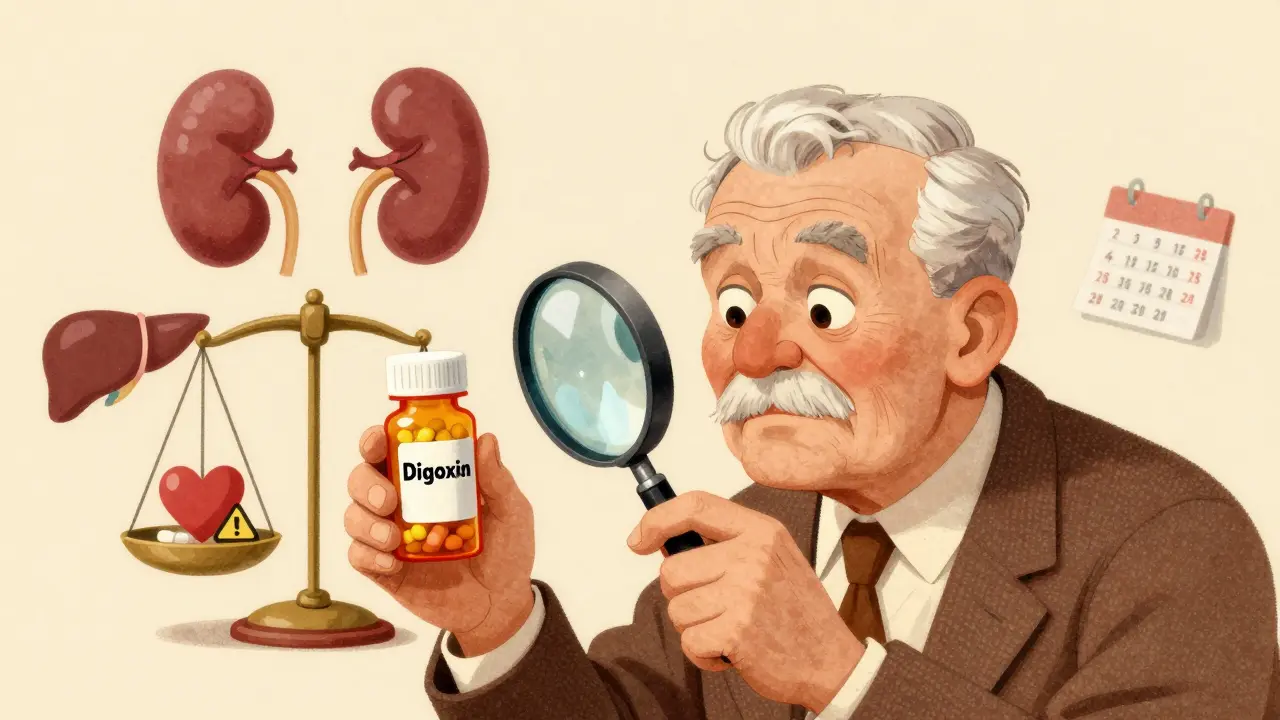
Doctors don’t just pick a dose because it’s on the bottle. That standard dose? It’s based on studies done mostly on healthy adults between 18 and 65. But what if you’re 78? Or weigh 300 pounds? Or have kidney trouble? Or take five other pills a day? That standard dose might be too high-or too low-for you. Take digoxin, a heart medication. Just two and a half times the normal dose can kill half the people who take it. That’s not a guess. That’s science. The reason? Digoxin has a narrow therapeutic index-meaning the difference between a helpful dose and a deadly one is tiny. The same goes for warfarin, phenytoin, and lithium. These aren’t rare drugs. Millions take them. And for each one, getting the dose wrong can land you in the hospital-or worse.The Therapeutic Index: Your Safety Margin
Every drug has a therapeutic index. It’s a number that tells you how wide the safety margin is. If the index is above 10, you’re usually safe with the standard dose. Penicillin? Index is 100+. You can take a little extra and nothing bad happens. But if the index is 2 or 3? You’re walking a tightrope. That’s what’s called a narrow therapeutic index (NTI) drug. These need careful tuning. For NTI drugs, doctors don’t just prescribe and hope. They monitor. Blood tests. Regular check-ins. Adjustments. A single missed dose or a new antibiotic can throw your levels off. That’s why warfarin users get their INR checked every few weeks. It’s not bureaucracy-it’s survival.What Changes Your Dose (Without You Realizing It)
Your body doesn’t process drugs the same way everyone else’s does. Here’s what shifts the balance:- Age: After 65, your kidneys and liver slow down. Many seniors need 20-30% less of certain meds.
- Weight: If you’re obese, standard dosing can be dangerously low. Doctors use ideal body weight plus 40% of extra weight to calculate the right amount.
- Kidney function: Creatinine clearance matters. If your kidneys aren’t filtering well, drugs build up. A simple blood test can tell you if your dose needs to drop.
- Liver health: The liver breaks down most drugs. If it’s damaged (from alcohol, hepatitis, fatty liver), drugs stick around too long. Child-Pugh or MELD scores help guide this.
- Other drugs: Taking five or more medications? That’s polypharmacy. One drug can block another from being broken down, causing toxic buildup. Statins with certain antibiotics? Risk of muscle damage. Antidepressants with painkillers? Seizure risk.
- Genes: About 25% of common drugs are affected by your DNA. Some people metabolize them too fast-drug doesn’t work. Others too slow-drug builds up. Genetic tests for CYP450 enzymes are becoming more common.
Real-World Problems Nobody Talks About
You might think, “My doctor knows what they’re doing.” But here’s the truth: clinical trials rarely include older adults, pregnant women, or people with multiple chronic conditions. So the dose you’re given? It’s based on data from people who aren’t you. That’s why so many elderly patients end up in the ER. A 72-year-old on digoxin eats a banana-potassium goes up, digoxin levels spike. No one warned her. A 68-year-old on warfarin starts taking a new OTC painkiller. His INR skyrockets. He bleeds internally. He didn’t know to tell his doctor. Even worse? Many doctors don’t have time to adjust doses properly. They rely on guidelines that say “start at 5 mg” and “increase if needed.” But what if “needed” means “you’re already at risk”? That’s guesswork-and it’s dangerous.How to Take Control
You don’t have to wait for your doctor to catch up. Here’s what you can do:- Know your meds. Write down every pill, supplement, and OTC drug you take. Include dosages and times. Bring it to every appointment.
- Ask about your therapeutic index. If you’re on warfarin, lithium, or phenytoin, ask: “Is this a narrow therapeutic index drug? What are the signs it’s too high or too low?”
- Request monitoring. If you’re on an NTI drug, insist on regular blood tests. Don’t wait for your doctor to suggest it.
- Ask about alternatives. Sometimes, switching to a drug with a wider safety margin makes more sense than tweaking the dose.
- Use a pharmacist. Pharmacists are trained in drug interactions and dosing. Ask for a free med review. Many pharmacies offer this. Studies show pharmacist-led programs cut hospital visits by 22%.
- Track side effects. Keep a simple log: “Day 3: dizzy after 10 a.m. pill.” “Day 7: bruising easily.” These details help your doctor adjust faster.
What’s Changing-And Why It Matters
The old way of dosing is fading. The FDA held a major meeting in 2019 about precision dosing. That’s the future: using real-world data, genetics, weight, age, kidney function, and even gut microbiome info to predict your perfect dose. Companies like DoseMe and InsightRX are building AI tools that crunch all this data and spit out a personalized dose recommendation. In transplant centers, this is already standard. In primary care? Still rare. But it’s coming. And it’s not just tech. Guidelines are changing too. Instead of “maximum tolerated dose” in cancer trials, researchers now test multiple doses to find the best balance of benefit and risk-before approving the drug. That’s a huge shift.The Bottom Line: Your Dose Is Yours to Manage
Medication isn’t a one-time fix. It’s a living adjustment. What works today might not work next month. Your body changes. Your other meds change. Your diet changes. Your stress levels change. Don’t assume your dose is perfect because it was prescribed. Ask questions. Track your symptoms. Push for monitoring if you’re on a high-risk drug. Talk to your pharmacist. Use your own observations as data. The goal isn’t just to take a pill. It’s to take the right pill, at the right dose, at the right time-so you feel better, not worse.Frequently Asked Questions
What does it mean if a drug has a narrow therapeutic index?
A narrow therapeutic index means the difference between a safe, effective dose and a dangerous or toxic dose is very small. Drugs like warfarin, digoxin, and lithium fall into this category. Even small changes in dose or how your body processes the drug can lead to serious side effects or reduced effectiveness. These drugs require close monitoring, often through regular blood tests.
Can I adjust my own medication dose if I feel it’s not working?
No. Never change your dose without talking to your doctor or pharmacist. Even if you think you know what’s going on, self-adjusting can be dangerous-especially with narrow therapeutic index drugs. Too much can cause toxicity. Too little can let your condition worsen. Always report how you’re feeling, then let your provider decide whether a change is needed.
How often should I get blood tests if I’m on a high-risk medication?
It depends on the drug and your health. For warfarin, most people need an INR test every 2-4 weeks when starting or adjusting the dose, then maybe every 4-6 weeks once stable. For lithium, testing every 3-6 months is typical, but more often if you’re elderly or have kidney issues. Always follow your provider’s schedule, and don’t skip tests just because you feel fine.
Why do some medications need dose adjustments for weight?
Many drugs are distributed in body water or fat. If you’re overweight or obese, standard doses may not reach effective levels in your tissues. For some drugs, doctors use ideal body weight plus 40% of excess weight to calculate the right dose. This ensures you get enough of the drug without overloading your system.
Can genetic testing help me find the right dose?
Yes-for some drugs. Genetic tests can show how your body breaks down medications, especially those processed by the CYP450 enzyme system. This affects drugs like antidepressants, blood thinners, and certain pain meds. If you’ve had bad reactions to meds before, or if standard doses never seem to work, ask your doctor about pharmacogenomic testing. It’s becoming more common and can prevent trial-and-error dosing.
What should I do if I miss a dose?
It depends on the drug. For some, like antibiotics, you can take it as soon as you remember. For others, like warfarin or seizure meds, missing a dose can be risky. Never double up unless your provider says to. Check the medication guide, call your pharmacist, or look up the drug’s official dosing instructions. When in doubt, skip the missed dose and go back to your regular schedule.
Are there tools or apps that help track medication doses?
Yes. Many free apps let you log doses, set reminders, and track side effects. Some, like Medisafe and MyTherapy, even alert you to potential interactions. For high-risk drugs, use one that lets you record lab values (like INR or lithium levels) so you can share trends with your doctor. These tools improve adherence and give your provider better data to adjust your dose safely.


Comments
This post is a godsend. I’ve been on warfarin for five years and never knew how much my liver was playing puppet master with my INR. Finally, someone explained why my doctor keeps nagging me about spinach and antibiotics. It’s not paranoia-it’s pharmacology.
Been there. Took lithium for bipolar and missed one blood test. Ended up in the ER with tremors and confusion. Turns out my thyroid meds were slowing down my clearance. Docs don’t always connect the dots. You gotta be your own advocate.
As a pharmacist, I see this every day. People think ‘prescribed = safe’-but polypharmacy is a silent killer. I run free med reviews at my clinic. One guy was on 11 meds. Turned out 4 were redundant, 2 were interacting, and one was causing his dizziness. He cried when he realized he didn’t have to feel like a zombie. You’re not being difficult-you’re being smart.
While I appreciate the attempt at elucidating pharmacokinetic principles, one must question the epistemological foundations of this piece. The reliance on ‘standard doses’ is a colonial remnant of evidence-based medicine’s hegemony. Where are the voices of indigenous populations whose metabolic pathways differ radically? Where is the critique of Big Pharma’s role in suppressing pharmacogenomic data? The narrow therapeutic index is not a scientific truth-it is a capitalist construct designed to perpetuate dependency.
Furthermore, the suggestion to ‘ask your pharmacist’ is a bourgeois distraction. Pharmacists are corporate agents. True autonomy lies in herbalism, fasting, and ancestral knowledge. I’ve cured my hypertension with turmeric and moon-phase alignment. Why are we still using 19th-century chemistry to treat 21st-century souls?
Bro. I’m on citalopram and my doc just gave me 20mg ‘cause that’s the default. I felt like a robot for 3 months. Got my CYP2C19 tested-turns out I’m a poor metabolizer. Switched to 10mg. Now I’m human again. 🧬💊 #PharmacogenomicsIsReal #DontGuessJustTest
They don’t want you to know this. They don’t want you to know that your dose is being calculated by a spreadsheet that never met you. That your kidney function is just a number on a chart while your body screams for help. They profit from your confusion. They profit from your silence. They profit from your ER visits. And now you’re supposed to be grateful for a blog post that tells you to ‘ask questions’? Wake up. This isn’t about dosing-it’s about control. Who owns your biology? And why do you still trust them?
I stopped taking all my meds. Started juicing. Did a 21-day cleanse. My INR normalized. My anxiety vanished. No blood tests. No doctors. Just me, my body, and the truth they buried under layers of white coats and FDA forms.
It is regrettable that the author fails to acknowledge the systemic inefficiencies in the Indian public healthcare system, wherein pharmacogenomic testing is inaccessible to 98% of the population. The suggestion to ‘consult a pharmacist’ is a Western luxury. In rural India, patients receive prescriptions from unlicensed practitioners who prescribe based on commission. The concept of ‘therapeutic index’ is unknown to 90% of prescribers. This article, while technically accurate, is irrelevant to the majority of global patients. The real issue is not dosing-it is access.
OMG YES. My grandma was on digoxin and her cardiologist didn’t even check her potassium. She got dizzy and fell-broke her hip. Turns out she was eating a ton of oranges and bananas after hearing they’re ‘heart healthy.’ No one told her that’s like pouring gasoline on a fire with digoxin. I printed out this whole article and gave it to her doc. He actually apologized. We’re all just one missed lab away from disaster.
In India, we call this ‘dose ka khel’-the game of dosage. My uncle was on phenytoin for seizures. Took the same dose for 10 years. Then he started drinking herbal tea with neem. Seizures came back. Doctor said ‘maybe your liver is tired.’ We didn’t test. We just changed the tea. He’s fine now. Sometimes, it’s not science-it’s culture.
I didn't know what to say until I read this. I've been on lithium for 8 years. Every time I feel off, I think it's me. Not the drug. Not the dose. Just me being weak. But this… this made me realize it's not me. It's the system. I started tracking my moods and my meals. I asked for my lithium level. It was high. They lowered it. I cried. Not because I was sad. Because I finally felt seen. Thank you.
It is illogical to suggest that patients should ‘track side effects’ when most are illiterate or lack digital access. The entire premise assumes a level of health literacy that does not exist in 70% of the world. This is not empowerment-it is victim-blaming disguised as education. The solution is not individual responsibility-it is universal healthcare with mandatory pharmacist oversight. Until then, this article is a luxury for the privileged.