Every year, over 51 million dispensing errors happen in community pharmacies across the U.S. Most of them never reach the patient-not because of barcodes or double-checks, but because a pharmacist asked one simple question: "What is this medication for?"
Why Patient Counseling Is the Last Line of Defense
Automated systems catch about half of all dispensing mistakes. Pharmacists double-checking each other catch two-thirds. But when a pharmacist sits down with a patient and actually talks to them? That’s when 83% of errors get caught. That’s not a guess. That’s data from Pharmacy Times, backed by decades of real-world use. This isn’t just about giving advice. It’s about verification. The patient is the final quality check. No machine can tell if a patient thinks they’re getting a blood pressure pill when they’re holding a diabetes drug. No scanner can detect if someone says, "I’ve never seen this blue pill before," when it’s supposed to be white. That’s where counseling works. The law has known this since 1990. OBRA ’90 made counseling mandatory for Medicare patients. Today, it’s standard practice everywhere-not because of regulation, but because it works.The Four Critical Checks in Every Counseling Session
Effective counseling isn’t random. It follows a proven structure. The UConn School of Pharmacy and the American Pharmacists Association agree: there are four things you must verify every time.- Confirm the purpose. Don’t ask, "Is this for your blood pressure?" That’s a yes-or-no trap. Ask, "What condition are you taking this medication for?" Open-ended questions catch 3.2 times more errors. If a patient says, "I think it’s for my knees," but the script is for atrial fibrillation-you’ve found a mistake.
- Check how they’ll take it. Have them show you. Can they open the bottle? Do they know if it’s once daily or four times a day? Do they think they should crush it? The "teach-back" method-where the patient repeats instructions in their own words-boosts error detection by 68%. One woman told her pharmacist she was supposed to take her insulin "after meals," but the label said "before." That’s a dangerous mix. She caught it because she was asked to explain it.
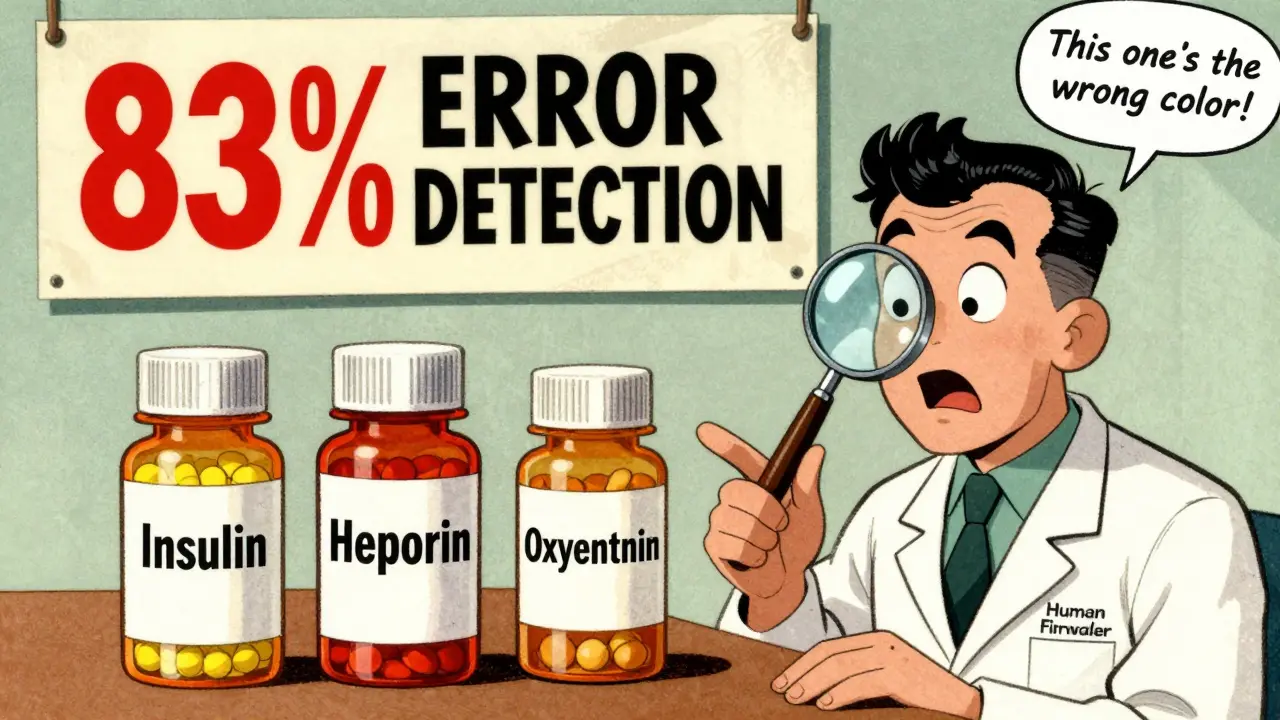
- Verify what it looks like. Show the patient the medication. Ask, "Does this look like what you’ve taken before?" Walgreens found this single question caught 29% of look-alike errors. That’s insulin vs. heparin. Oxycontin vs. oxycodone. Pills that look almost identical but act completely differently. Patients notice changes. They just need to be asked.
- Review interactions and allergies. Cross-check the new med against their current list. Did they start a new blood thinner? Are they on a statin? Are they allergic to sulfa? This isn’t just about safety-it’s about catching the wrong drug. A patient once said, "I’m allergic to this color pill," and it turned out the pharmacist had dispensed the wrong brand. The active ingredient was the same, but the patient had a reaction to the dye. That’s a mistake only a person could catch.
Altogether, this takes about 2 minutes and 40 seconds. That’s the gold standard. Shorter than that? You’re skipping steps. Longer? You’re overdoing it. Stick to the checklist.
Why Counseling Beats Technology Every Time
Barcodes? They catch 53% of errors. Pharmacist double-checks? 67%. But counseling? 83%. Why the gap? Because technology checks the pill. Counseling checks the person. A barcode can’t know if the patient is confused. It can’t hear hesitation in their voice. It can’t notice they’re holding the bottle sideways, unsure how to open it. It doesn’t know if the patient is taking their grandchild’s asthma inhaler because they thought it was their own. The Institute for Safe Medication Practices calls this a "human firewall." Automated systems are great. But they’re blind to context. Patients aren’t. And when you give them the chance to speak, they’ll tell you when something’s wrong.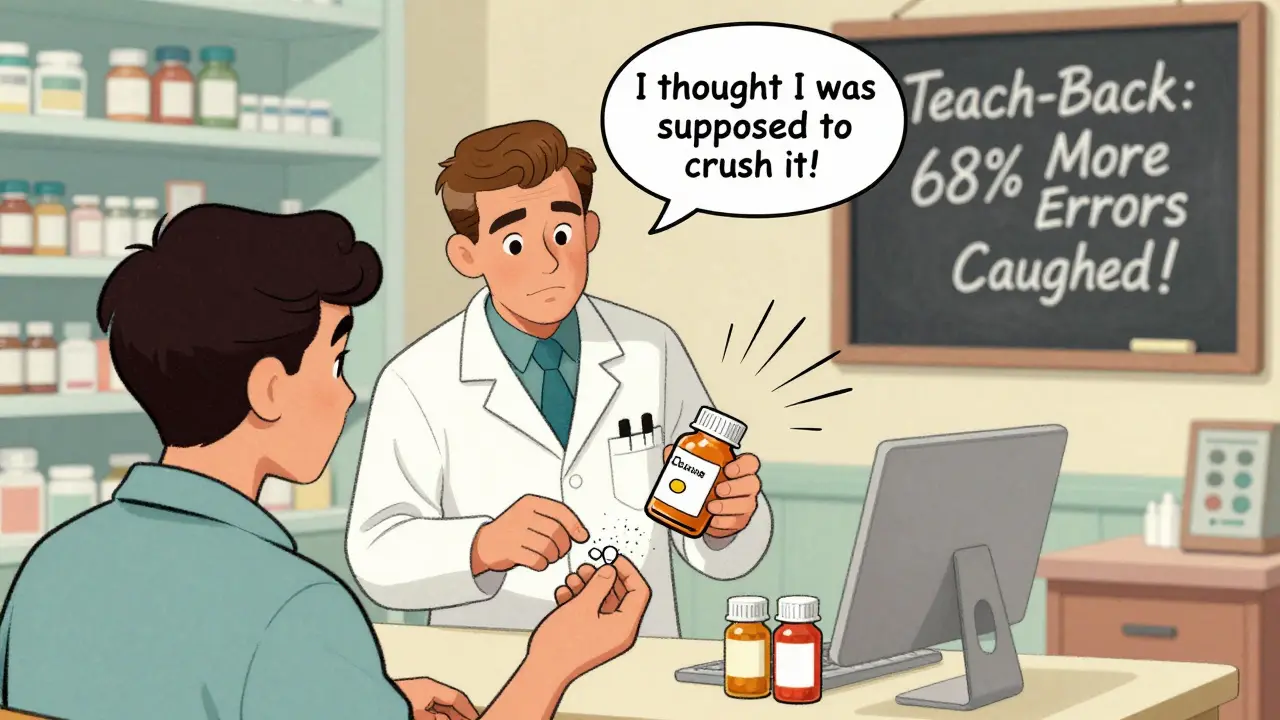
When Counseling Falls Short
It’s not perfect. And it’s not always done right. In CVS pilot stores, pharmacists asked, "Does this look familiar?" and caught over 1,200 errors in three months. But in other pharmacies, counselors spend just 1.2 minutes per patient-far below the 2.3-minute minimum needed. Why? Pressure to move faster. Corporate productivity targets. Staff shortages. One Reddit user wrote: "I asked my pharmacist if she could explain my new med. She said, ‘We’re backed up. Just read the label.’ I left scared." And that’s the problem. Counseling isn’t optional. It’s the last safety net. Skip it, and you’re gambling with lives. Even worse: 18.7% of patients refuse counseling. That’s a gap. You can’t force them. But you can make it worth their time. Explain why it matters. Say, "This is how we make sure you don’t get the wrong pill." People respond to safety, not speed.Who Needs It Most
Not everyone needs the same level of attention. But some patients are at much higher risk.- Patients over 65. They’re 3.7 times more likely to suffer harm from a dosing error.
- People with low health literacy. 42% of undetected errors happen here. They don’t know what "take with food" means. Or why they need two different pills for the same thing.
- Those on high-alert meds. Insulin, opioids, blood thinners-1 in 5 errors involve these. One wrong dose can kill.
- New prescriptions. 91% of errors on new meds are caught during counseling. Refills? Only 33%. Why? People assume it’s the same. It’s not always.
Focus your time where it matters most. Don’t rush through the elderly patient. Don’t skip the one on five meds. They’re the ones who need you most.
How to Make It Work in Real Life
You know it’s important. But how do you do it when you’re swamped? The University of Michigan study gives a real answer: use a structured 4-step framework and train your team.- Identity verification (27 seconds): "Can you confirm your name and date of birth?"
- Purpose confirmation (43 seconds): "What are you taking this for?"
- Appearance and administration (52 seconds): "Show me how you’ll take this. Does it look right?"
- Interactions and allergies (38 seconds): "Any new meds or allergies since your last visit?"
That’s 2 minutes 40 seconds. Total.
Use pharmacy technicians for the first two steps. In 42 states, they’re allowed to do preliminary counseling under supervision. That frees you up to focus on the complex cases. Document everything. NABP’s 2022 standards require notes on what was discussed. Pharmacies that do this cut liability claims by 44%. That’s not just safety-it’s savings.The Bigger Picture: Safety Pays
Counseling costs about $0.87 per prescription. Barcode systems? $1.35. Pharmacist double-checks? $2.10. Independent pharmacies that use structured counseling report 19% lower malpractice insurance premiums. Why? Fewer errors. Fewer lawsuits. CMS now ties 8.5% of Medicare Part D payments to counseling quality. The FDA says it’s the most effective way to catch errors technology misses. And by 2027, Evaluate Pharma predicts pharmacies with strong counseling will gain 12-15% more market share. Patients notice. A Healthgrades review from June 2023 says: "The pharmacist caught that my new blood thinner was the wrong strength when I said it looked smaller than before." That’s trust. That’s loyalty.Final Thought: You’re Not Just Dispensing. You’re Protecting.
Your job isn’t to fill prescriptions. It’s to make sure they’re right. Every time you skip counseling, you’re betting a patient’s life on a barcode, a checklist, or a tired pharmacist’s memory. But when you sit down, ask the right questions, and listen? You’re not just preventing an error. You’re saving a life.How long should a patient counseling session last to catch dispensing errors?
A minimum of 2.3 minutes is needed to properly verify all safety elements, according to NCBI’s StatPearls. The most effective protocol, used by leading pharmacies, takes 2 minutes and 40 seconds and includes verifying patient identity, medication purpose, dosage instructions, physical appearance, and drug interactions. Sessions shorter than 2 minutes miss critical checks.
Can pharmacy technicians help with patient counseling?
Yes. In 42 U.S. states, pharmacy technicians are permitted to conduct preliminary counseling under pharmacist supervision. They can verify patient identity, confirm medication purpose, and check basic instructions. The pharmacist then reviews high-risk items like drug interactions and appearance. This approach increases effective counseling time by 37% without compromising safety.
What types of errors does patient counseling catch that technology misses?
Counseling catches errors related to patient understanding and expectations-things machines can’t detect. This includes wrong medication purpose (e.g., a patient thinks they’re getting a blood pressure pill but received a diabetes drug), incorrect administration (e.g., crushing a pill that shouldn’t be crushed), mismatched appearance (e.g., a patient recognizes the wrong color or shape), and unrecognized allergies or interactions. These are human-level errors that automated systems aren’t designed to identify.
Why are open-ended questions better than yes/no questions in counseling?
Open-ended questions like "What is this medication for?" require the patient to explain in their own words, revealing misunderstandings. Closed questions like "Is this for your blood pressure?" can be answered with a yes even if the patient is wrong. Studies show open-ended questions catch 3.2 times more errors because they expose gaps in knowledge rather than just confirming assumptions.
Is patient counseling required by law?
Yes, for Medicare Part B beneficiaries under OBRA ’90. While not federally mandated for all patients, 34 states require documented counseling for new opioid prescriptions. The Joint Commission and NABP treat it as a standard of care. CMS now includes counseling effectiveness in Medicare Part D reimbursement metrics, making it a de facto requirement for financial compliance.
What’s the biggest barrier to effective patient counseling?
Time pressure. When pharmacists handle more than 14 prescriptions per hour, counseling effectiveness drops from 83% to 41%. Corporate productivity targets often discourage thorough sessions. The solution is staffing adjustments, technician support, and leadership that prioritizes safety over speed.




Comments
Bro, I work at a CVS and they make us do counseling in 90 seconds. I just say 'Take it with food' and hand them the bag. If they die, it’s on them. 😅
I’ve seen pharmacists skip the ‘what’s this for?’ question because they’re ‘in a rush’-and then patients end up on the wrong meds. It’s not just negligence-it’s negligence with a paycheck. And yes, I’ve been that patient. I asked. They rolled their eyes. I left. I Googled it later. Turned out I was right to be scared.
Of course counseling works-because humans are fallible and machines aren’t. But here’s the real problem: pharmacies treat patients like inventory. They don’t want to listen. They want to scan, bag, and move on. This isn’t healthcare-it’s a conveyor belt with a white coat.
83% error detection? That’s statistically impossible. You’re conflating correlation with causation. The real reason counseling catches errors is because it’s the last step before the patient leaves-so any mistake that slipped through earlier gets caught by chance, not because of the question format. Also, barcodes catch more than 53%. You’re cherry-picking data.
The notion that counseling is a ‘human firewall’ is a romanticized myth. In reality, most patients are either too confused to articulate their concerns or too intimidated to question authority. The data may show 83%, but that’s likely inflated by selection bias-those who refuse counseling are excluded from the metrics. The real solution is standardized electronic alerts and AI-driven reconciliation, not asking people to paraphrase their medication regimen.
My grandmother was given metformin instead of metoprolol. She didn’t say anything because she didn’t want to ‘be a bother.’ That’s the real issue-not the pharmacist’s technique, but the patient’s fear of being dismissed. You can ask all the open-ended questions you want, but if the patient doesn’t feel safe speaking up, it’s all theater.
It is profoundly encouraging to observe that, in an era increasingly dominated by algorithmic efficiency and automation, the fundamental humanity of direct patient interaction remains the most reliable safeguard against medical error. The act of sitting, listening, and asking open-ended questions is not merely a procedural formality-it is an ethical imperative, a quiet act of dignity extended to the vulnerable. One may argue that time constraints are systemic, but one cannot reasonably justify the erosion of care under the banner of productivity. The patient is not a transaction; they are a person with lived experience, with intuition, with memory-and that intuition, when honored, often reveals what no barcode ever could. The data is clear, the ethics are unambiguous, and the cost of inaction is measured not in dollars, but in lives. Let us not mistake convenience for compassion.
Bro, this is beautiful 🙏❤️. In India, we don’t always have pharmacists who take time-but I’ve seen grandmas who remember every pill they’ve ever taken. They’re the real safety net. Let’s train techs, give pharmacists breaks, and stop treating humans like machines. We’re not just filling scripts-we’re holding hands with fear. 🌿💊
Yeah, sure. Counseling works. But let’s be real-this is just another way for the AMA and pharmacy boards to inflate their own importance. You think the average person cares if their pill is blue or white? Most people take whatever’s in the bottle and hope for the best. And don’t get me started on ‘open-ended questions.’ You think some 70-year-old with dementia is gonna tell you they’re taking their neighbor’s blood thinner because ‘it looked familiar’? This whole thing is performative healthcare for people who think talking is the same as fixing.