Epigastric Pain Symptom Checker
Answer the following questions to help determine potential causes of your epigastric pain.
Potential Cause of Your Pain
Key Takeaways
- Epigastric pain can be an early sign of IBD, but it also appears in many non‑IBD conditions.
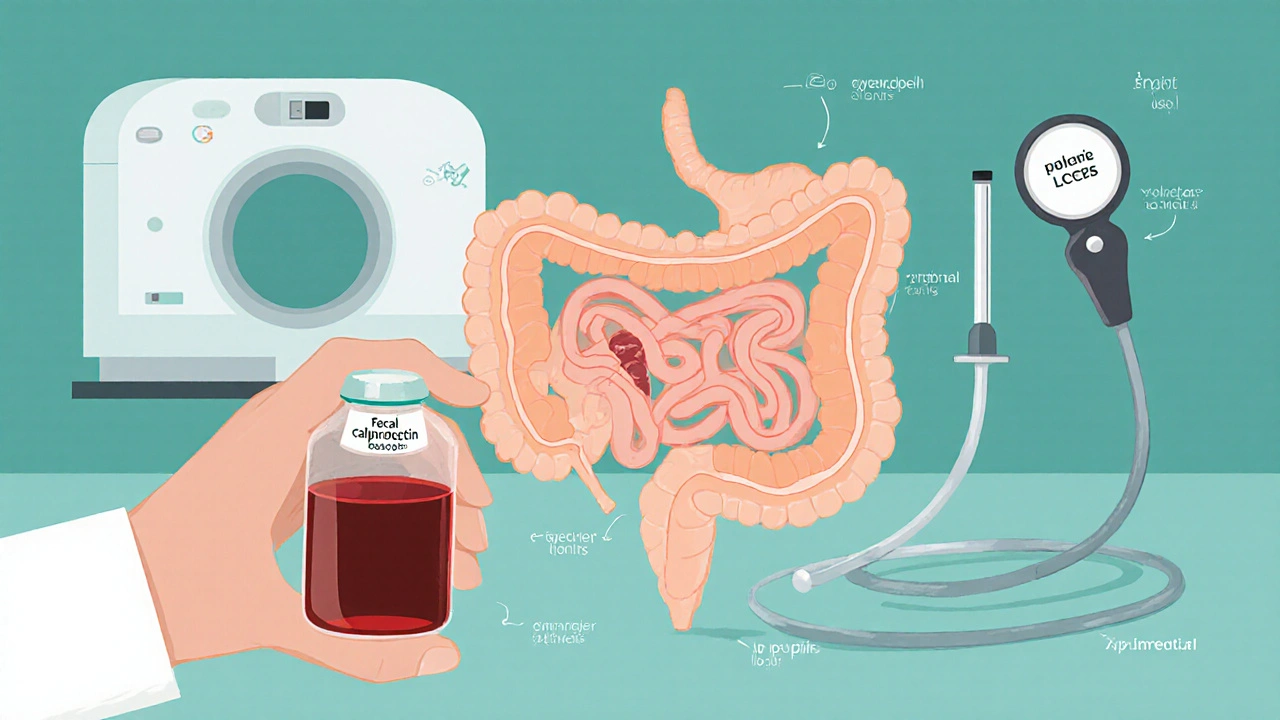
- Distinguishing IBD‑related pain relies on symptom patterns, lab markers like fecal calprotectin, and visual confirmation via endoscopy.
- Treatment blends medication, diet, and regular monitoring to keep flare‑ups under control.
- Prompt medical evaluation is crucial whenever pain is persistent, worsening, or accompanied by weight loss, blood in stool, or fever.
Most people think of epigastric pain as a stomach‑ache caused by heartburn or an ulcer. Yet for a sizable group, that discomfort is actually a red flag of a deeper gut problem - inflammatory bowel disease (IBD). If you’ve ever felt a burning or gnawing sensation just below your breastbone and wondered whether it might be linked to Crohn’s or ulcerative colitis, this guide breaks down the why, how, and what‑next in plain language.
Understanding Epigastric Pain
Epigastric Pain is a discomfort located in the upper central region of the abdomen, just above the stomach and below the ribs. It often feels like a burning, pressure, or dull ache and can be triggered by food, stress, or underlying disease. While it’s most famously linked to acid reflux, the pain’s location makes it a common symptom in a range of gastrointestinal disorders.
What Is Inflammatory Bowel Disease?
Inflammatory Bowel Disease (IBD) is an umbrella term for chronic, immune‑mediated inflammation of the gastrointestinal tract. The two major forms are Crohn’s disease and ulcerative colitis. IBD affects roughly 3 million people in the United States and an increasing number worldwide, with a noticeable rise in younger adults.
How IBD Can Trigger Epigastric Pain
Both Crohn's disease and ulcerative colitis primarily target the intestines, but the inflammation can extend upward, irritating the upper gut and causing epigastric discomfort. In Crohn’s disease, the inflammation is often patchy and can involve the duodenum (the first part of the small intestine), directly beneath the epigastric zone. Ulcerative colitis usually starts in the colon, but severe cases can produce systemic inflammation that sensitizes nerves in the upper abdomen.
Other IBD‑related mechanisms include:
- Secondary acid hypersecretion due to altered gut motility.
- Strictures or fistulas near the upper small bowel that produce obstructive pain.
- Medication side‑effects - for example, non‑steroidal anti‑inflammatory drugs (NSAIDs) used for joint pain can worsen both IBD and upper‑gut irritation.
Separating IBD‑Related Pain from Other Upper‑Abdomen Issues
Because epigastric pain is a symptom shared by many ailments, clinicians use a combination of history, labs, and imaging to pinpoint the cause. Below is a quick comparison of the most common culprits.
| Condition | Typical Triggers | Associated Signs | Key Diagnostic Test |
|---|---|---|---|
| Inflammatory Bowel Disease | Food, stress, medication withdrawal | Weight loss, night sweats, blood in stool, extra‑intestinal symptoms | Colonoscopy with biopsies; fecal calprotectin |
| Gastroesophageal reflux disease | Large meals, lying down, caffeine, alcohol | Heartburn, regurgitation, sour taste | Upper endoscopy or pH monitoring |
| Peptic ulcer disease | NSAID use, H. pylori infection | Melena, anemia, pain improves with food | Upper endoscopy, H. pylori testing |
| Functional dyspepsia | Stress, irregular meals | Bloating, early satiety, no alarm features | Diagnosis of exclusion; Rome IV criteria |
Diagnostic Pathway for Suspected IBD‑Related Epigastric Pain
- Detailed medical history - note duration, relation to meals, presence of diarrhea, blood, or extra‑intestinal symptoms.
- Blood work - complete blood count, C‑reactive protein (CRP), and erythrocyte sedimentation rate (ESR) to gauge inflammation.
- Stool testing - fecal calprotectin is a non‑invasive marker that rises sharply in IBD compared with functional disorders.
- Imaging - abdominal ultrasound or MRI enterography can reveal thickened bowel loops, strictures, or fistulas in the upper gut.
- Endoscopic evaluation - a colonoscopy (often combined with an upper endoscopy) provides visual confirmation and tissue samples for histology.
When the work‑up points toward IBD, the gastroenterologist will classify the disease subtype, assess severity, and design a personalized treatment plan.

Managing Epigastric Pain in the Context of IBD
Effective control hinges on two fronts: reducing gut inflammation and addressing the pain itself.
- Anti‑inflammatory meds: 5‑ASA agents (e.g., mesalamine) for mild ulcerative colitis; biologics such as anti‑TNFα (infliximab) or anti‑integrin (vedolizumab) for moderate‑to‑severe Crohn’s.
- Nutritional strategies: Small, frequent meals; low‑residue diet during flares; probiotic supplementation shown to improve dysbiosis in some studies.
- Acid‑suppressive therapy: Proton pump inhibitors (PPIs) can relieve overlapping GERD‑type pain, but long‑term use should be balanced against infection risk.
- Pain relief: Acetaminophen is preferred; NSAIDs are generally avoided because they can trigger IBD exacerbations.
- Monitoring: Regular fecal calprotectin checks and periodic colonoscopy help catch silent inflammation before it spikes.
Quick Checklist for Patients Experiencing Upper‑Abdominal Discomfort
- Track pain intensity, timing, and food triggers in a diary. \n
- Note any accompanying symptoms: diarrhea, blood, weight loss, fever.
- Check recent medication use - especially NSAIDs or steroids.
- Schedule blood and stool tests if pain persists more than two weeks.
- Ask your doctor about a colonoscopy or upper endoscopy if alarm signs appear.
Frequently Asked Questions
Can epigastric pain be the first sign of IBD?
Yes. In about 15‑20% of newly diagnosed IBD patients, upper‑abdominal pain precedes classic lower‑gut symptoms like diarrhea. Early recognition allows faster treatment and reduces complication risk.
How reliable is fecal calprotectin for distinguishing IBD from functional disorders?
Fecal calprotectin levels above 250µg/g are strongly predictive of intestinal inflammation. While not 100% specific, it’s far more accurate than symptom checklists alone and helps decide whether endoscopy is warranted.
Should I take antacids for epigastric pain if I have IBD?
Occasionally, antacids can relieve overlapping acid‑related discomfort, but they don’t treat the underlying inflammation. Consult your gastroenterologist before adding any over‑the‑counter acid reducers.
When is it an emergency?
Seek immediate care if the pain is sudden and severe, if you notice vomiting blood, black stools, high fever, or if you feel faint. These signs may indicate a perforation, severe bleed, or toxic megacolon - conditions that need urgent treatment.
Can lifestyle changes reduce epigastric pain in IBD?
Adopting a low‑fat, low‑spice diet, managing stress through mindfulness, and avoiding smoking can lower overall gut inflammation and may ease upper‑abdominal discomfort over time.
Next Steps: When to See a Doctor
If you’ve logged persistent epigastric pain for more than two weeks, or if it’s coupled with any of the alarm features listed above, book an appointment with a gastroenterologist. Bring your symptom diary, recent lab results, and a list of medications. Early evaluation can differentiate IBD from other causes and set you on the right treatment path.



Comments
In the realm of gut health we often forget that the body is a covenant of responsibility.
If you swallow the excuse that pain is merely "stress", you betray the trust your intestine places in you.
The epigastric ache described in the article is not a trivial inconvenience; it is a siren calling for introspection.
We must ask ourselves why we continue to drown in processed foods while ignoring the subtle cries of inflammation.
Philosophically, every symptom is a message, a dialectic between our choices and our biology.
To dismiss it as "just heartburn" is to deny the moral agency we possess over our own well‑being.
Moreover, the data on fecal calprotectin is a crystal clear beacon that separates genuine inflammation from imagined discomfort.
When the test lights up, it is not a random number but evidence that our gut demands attention.
Ignoring such evidence equates to willful negligence, a neglect of the self we are obligated to nurture.
It also reflects a broader societal trend of valuing immediacy over diligent care.
The article wisely suggests colonoscopy, yet many shy away from it out of fear.
Fear, however, should be confronted, for it is the only barrier between you and proper diagnosis.
In practical terms, keep a symptom diary, avoid NSAIDs, and seek a gastroenterologist before the pain escalates.
Remember, the gut does not forgive chronic insult, and the price of procrastination can be far higher than a brief inconvenience.
So, honor your body, act with humility, and let the science guide your next steps.
The choice, ultimately, remains yours, but the consequences will echo in every future meal you enjoy.
Consider tracking your meals and symptoms to share with your doctor.
Our nation has produced world‑class doctors, yet we still watch people suffer from gut pain without seeking proper care.
It is unacceptable that so many rely on over‑the‑counter fixes while ignoring the real threat of IBD.
The statistics show a rising incidence, and that is a direct result of ignoring lifestyle and dietary discipline.
If you think NSAIDs are harmless, think again; they are a silent killer for our digestive system.
The article mentions fecal calprotectin, but people treat it like a myth rather than a vital diagnostic tool.
This complacency is a betrayal of our cultural heritage that once prized natural healing.
Wake up, prioritize real medical evaluation, and stop feeding the pharmaceutical lobby with your ignorance.
Your gut will thank you, and the nation will be healthier when individuals take responsibility.
I hear the frustration and want to add a gentle reminder that seeking help is a sign of strength, not weakness.
A step‑by‑step plan-starting with a symptom log, then a blood work panel-can make the process feel manageable.
When you share this information with your doctor, they can pinpoint whether a colonoscopy or a simple stool test is appropriate.
Remember, many patients find relief once the correct treatment pathway is identified.
Take it one day at a time, and don’t hesitate to lean on support groups for encouragement.
Hey! dont let that tummy ache bring you down, u got this!
Keep track of what you eat and hit up a doc soon, ur gut will thank u.
From a broader perspective, epigastric pain serves as a reminder of the mind‑body continuum.
The interplay between inflammation and stress underscores the need for holistic approaches.
Incorporating mindfulness, balanced nutrition, and evidence‑based medication often yields the best outcomes.
Ultimately, knowledge empowers patients to collaborate effectively with their clinicians.
It's plain that ignoring warning signs is irresponsible.
We all share a duty to listen to our bodies.
Take the recommended tests before the problem worsens.
Oh, the drama of a simple ache turning into an existential crisis!
People swear by coffee, pizza, and midnight snacks as if they were holy sacraments.
Then they gasp when the stomach rebels with a burning flare.
The article tries to be scientific, but forgets the human element of fear and denial.
I mean, who wants to think about colonoscopies while binge‑watching series?
Yet the reality is that without proper screening, the disease can stealthily progress.
Your gut is not a joke; it's a battlefield where microbes and immunity clash.
If you keep popping ibuprofen like candy, you're basically handing ammunition to the enemy.
So, listen to that gnawing feeling and schedule that appointment before regret knocks.
Trust me, the peace of mind after a clean bill of health is worth the brief inconvenience.
It is evident that the dissemination of medical information is often manipulated by unseen interests.
The emphasis on endoscopic procedures may serve ulterior commercial agendas rather than patient welfare.
Consequently, one must remain vigilant and critically assess the purported benefits presented.
A thorough independent review of the data is indispensable before committing to invasive diagnostics.
Honestly, most of this sounds like recycled fluff.
While everyone nods to the standard workup, the overreliance on fecal calprotectin is questionable.
Studies show a significant false‑positive rate in patients with minor infections.
Thus, sweeping it as a definitive marker for IBD can lead to unnecessary anxiety.
A more nuanced approach, integrating clinical context, would serve patients better.
In the end, medicine thrives on skepticism, not blind acceptance of protocols.