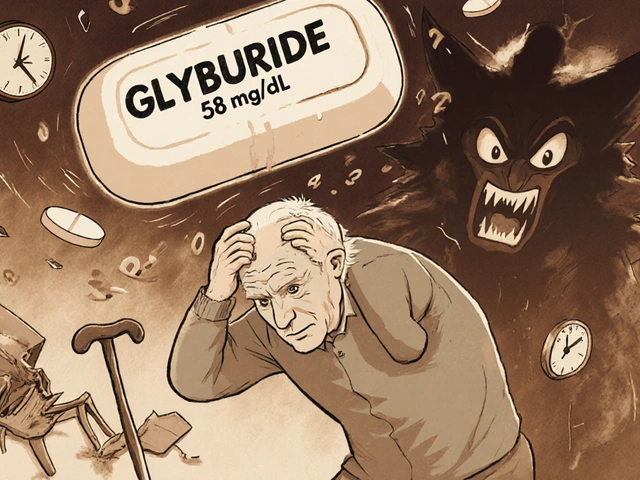
When your blood sugar stays high for years, it doesn’t just wear out your kidneys or nerves-it slowly damages the tiny blood vessels in your eyes. This is diabetic retinopathy, and it’s the number one reason people with diabetes lose their vision. The scary part? You might not notice anything wrong until it’s too late.
What Happens Inside Your Eye
Your retina is the light-sensitive layer at the back of your eye. It’s packed with millions of cells that turn light into signals your brain turns into images. These cells need a steady flow of oxygen and nutrients, delivered by a network of tiny blood vessels. In diabetes, those vessels get damaged by high glucose levels. At first, they weaken and bulge out, forming microaneurysms-tiny balloon-like swellings. Then, they start leaking fluid or blood. Sometimes, they get completely blocked. When that happens, parts of the retina don’t get enough oxygen. Your eye tries to fix this by growing new blood vessels. But these aren’t normal. They’re fragile, messy, and prone to bleeding. They can pull on the retina, causing it to detach. They can also block fluid drainage in your eye, leading to pressure buildup and glaucoma. All of this can happen without you feeling a thing.The Three Stages of Retinal Damage
Diabetic retinopathy doesn’t show up overnight. It creeps in over years, and it has clear stages:- Mild nonproliferative: Small bulges in blood vessels. No symptoms yet.
- Moderate to severe nonproliferative: More vessels are blocked. Fluid leaks into the retina, causing swelling-especially in the macula, the center of your vision. This is called diabetic macular edema, and it makes things look blurry or wavy.
- Proliferative: New, abnormal blood vessels grow on the retina’s surface. They bleed into the vitreous (the gel inside your eye), causing floaters, dark spots, or sudden vision loss. Scar tissue can form and pull the retina away from the back of your eye.
Diabetic macular edema can happen at any stage, even before the retina starts growing new vessels. About 1 in 15 people with diabetes will develop it. And once the macula swells, your sharp, detailed vision-reading, driving, recognizing faces-starts to go.
Why You Might Not Know You Have It
This is the biggest trap. Most people don’t feel pain. Their vision stays normal. That’s why routine eye exams are non-negotiable. A study from the Texas Diabetes Institute found that 68% of patients didn’t notice symptoms until their retinopathy was already moderate or worse. By then, damage is done. When symptoms do show up, they’re not subtle:- Blurred or wavy vision
- Floaters or dark spots floating across your sight
- Difficulty seeing at night or in low light
- Fading or washed-out colors
- Loss of side vision
- Sudden vision loss from bleeding inside the eye
If you’ve had diabetes for more than 10 years, your risk jumps. But even people with well-controlled diabetes aren’t safe. The damage builds slowly. It’s not about how bad your sugar is today-it’s about how long it’s been high.
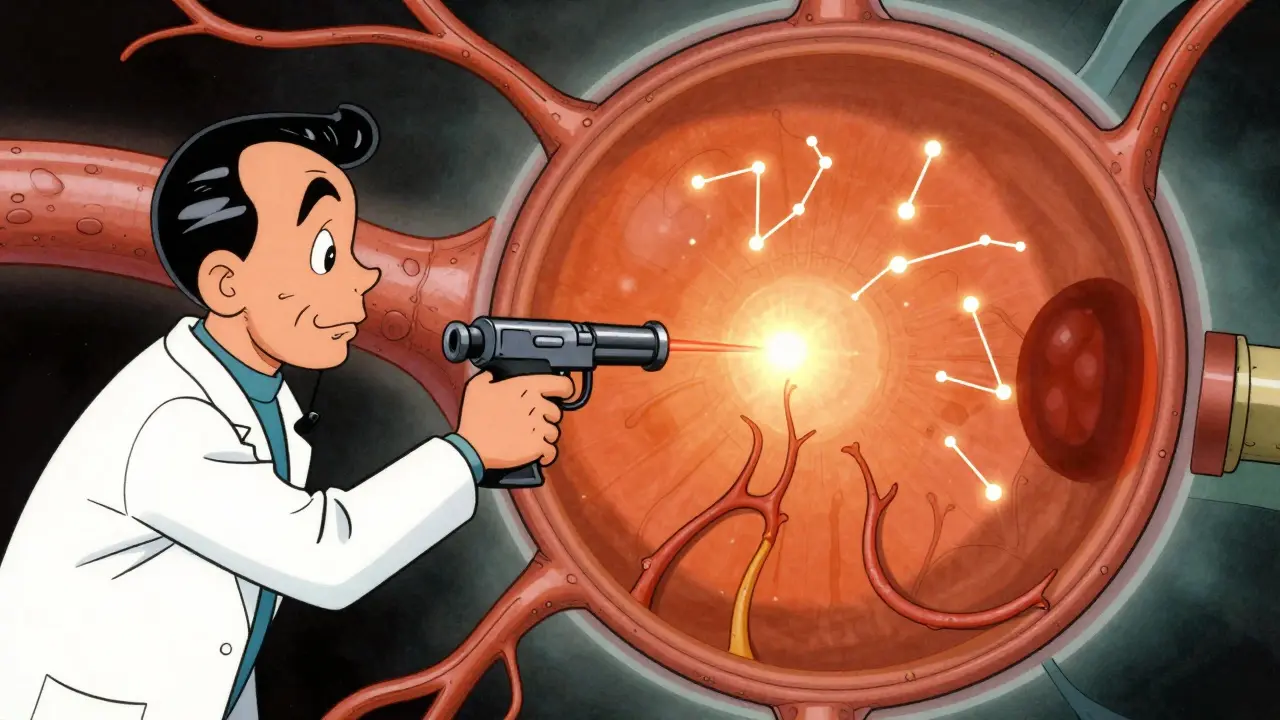
Laser Treatment: How It Stops the Damage
Laser treatment has been the backbone of diabetic retinopathy care for decades. It’s not glamorous. It’s not a cure. But it works. There are two main types:- Focal or grid laser: Used for diabetic macular edema. The doctor targets specific leaking vessels in the macula. The laser seals them off, reducing swelling. It doesn’t restore lost vision, but it stops it from getting worse.
- Scatter (panretinal) laser: Used for proliferative retinopathy. Instead of targeting one spot, the laser makes hundreds of tiny burns across the peripheral retina. This reduces the retina’s demand for oxygen, which tells the body to stop growing those dangerous new blood vessels.
Both procedures are done in an outpatient clinic. You’re awake, but your eye is numbed. You might feel a brief pinch or bright flash with each laser pulse. It takes about 15 to 30 minutes per eye. Most people go home the same day.
Success rates? Studies show that if you get laser treatment before vision is severely damaged, you have a 95% chance of keeping your sight. That’s not a guarantee you’ll see better-but it’s a strong guarantee you won’t lose what you have.
It’s Not Just About the Laser
Laser treatment doesn’t fix diabetes. It just protects your eyes from its effects. If your blood sugar stays high, the damage will keep coming. That’s why managing your diabetes is just as important as the laser.- Keep your HbA1c below 7% if your doctor says it’s safe for you.
- Control your blood pressure. High pressure makes leaking vessels worse.
- Lower your cholesterol. Fatty deposits can clog small eye vessels.
- Quit smoking. Smoking speeds up blood vessel damage.
- Get checked every year-even if your vision feels fine.
Some people think once they’ve had laser treatment, they’re done. They’re wrong. Retinopathy can come back. New vessels can grow. Swelling can return. That’s why lifelong monitoring is part of the deal.
What’s New in Treatment
Laser isn’t the only tool anymore. Anti-VEGF injections-medicines like ranibizumab or aflibercept-are now used often, especially for macular edema. These are injected directly into the eye and work by blocking the signal that tells the body to grow abnormal blood vessels. They can reduce swelling faster than laser alone. Many doctors now use a combo approach: injections to shrink swelling quickly, then laser to prevent it from coming back. It’s not about choosing one or the other-it’s about using the right tool at the right time. Research is also looking at ways to repair damaged retinal cells, not just stop the damage. But those are still years away. For now, the proven path is: control your diabetes, get screened yearly, and treat early.
What Happens If You Wait
Waiting isn’t an option. Once the retina detaches or the vitreous fills with blood, vision loss can be permanent. Even with surgery, you might only get partial recovery. And if glaucoma develops from blocked drainage, pressure can destroy your optic nerve. The good news? Almost all vision loss from diabetic retinopathy is preventable-if you act early. The National Eye Institute says that regular eye exams and timely treatment can reduce severe vision loss by up to 95%.What You Need to Do Now
If you have diabetes:- Get a dilated eye exam at least once a year. If you have retinopathy, your doctor may want to see you every 3 to 6 months.
- Don’t wait for blurry vision. By then, it’s often too late.
- Keep your blood sugar, blood pressure, and cholesterol numbers in your target range.
- Ask your eye doctor if you’re a candidate for anti-VEGF injections.
- If you’ve had laser treatment, don’t skip follow-ups.
If you’re a caregiver or family member, help remind your loved one about eye appointments. Many people with diabetes forget. Vision loss doesn’t just affect them-it affects everyone around them.
Can diabetic retinopathy be reversed?
Early damage can be stabilized, but once photoreceptor cells die or the retina detaches, the damage is permanent. Laser and injections can prevent further loss, but they don’t restore vision that’s already gone. That’s why catching it early is everything.
Is laser treatment painful?
Most people feel a slight pressure or brief sting with each laser pulse, but not pain. Numbing drops are used, and the whole process is quick. Some people see spots or have blurry vision for a few hours afterward, but it clears up.
Do I still need laser if I’m on insulin?
Yes. Insulin helps control blood sugar, but it doesn’t undo damage already done to your retina. You still need regular eye exams and treatment if retinopathy is detected. Medication and eye care work together.
Can I drive after laser treatment?
Not right away. Your pupils will be dilated, and your vision may be blurry or sensitive to light. Most people wait until the next day to drive. Always follow your doctor’s advice.
How often should I get screened if I have type 2 diabetes?
Once a year, starting when you’re diagnosed. If your eyes are healthy, you might stretch it to every two years-but only if your doctor says so. If you have any signs of retinopathy, you’ll need exams every 3 to 6 months.
Does pregnancy affect diabetic retinopathy?
Yes. Pregnancy can speed up retinopathy, especially if blood sugar isn’t tightly controlled. Women with diabetes should have an eye exam before getting pregnant and again during the first trimester. More frequent checks may be needed throughout pregnancy.





Comments
This is why we need to stop coddling diabetics who think insulin makes them invincible. Your eyes don't care if you're on meds. If your sugar's up, your retina's dying. Period.
Get checked or go blind. Simple.
Laser treatment? That's just Big Pharma's way of keeping you hooked. What about the real solution? Fasting. Ketosis. Cutting carbs. No one talks about that because the eye doctors get paid per procedure. You're being played.
It is, without a shadow of a doubt, an ethical imperative for individuals diagnosed with diabetes to undergo annual ophthalmological evaluations, as the pathophysiological cascade leading to retinal vascular compromise is both insidious and irreversible once advanced stages are reached. The notion that asymptomatic progression negates the necessity of intervention is not only medically unsound but morally indefensible.
The real tragedy isn't the laser-it's the epistemological failure of a system that treats symptoms instead of root causes. We've turned the body into a machine to be patched, not a system to be understood. Anti-VEGF injections? Band-aids on a leaking dam. The real question: why are we still letting glucose run wild in the first place?
Laser treatment is a scam. The FDA knows this. The real cause is glyphosate in your food. It destroys your capillaries. That’s why organic people never get retinopathy. I’ve seen it. My cousin’s friend’s neighbor went keto, stopped eating corn syrup, and her vision cleared in 3 months. No laser. No injections. Just clean food. They’re hiding this.
Thank you for this comprehensive and clinically accurate overview. It is imperative that patients with diabetes understand that early detection and consistent management are the cornerstones of vision preservation. I encourage all readers to prioritize their annual dilated eye exams as non-negotiable components of their health regimen.
You say 'control your sugar' like it's that easy. Try living on a fixed income with no access to fresh food. Try being a single mom working two jobs. This isn't a moral failure. It's a system failure. And now you want me to get laser surgery? For what? To keep seeing my kids while I die of kidney failure?
Oh sweetie, you really think the doctor's gonna care about your 'laser treatment' after you've spent 15 years eating Pop-Tarts and calling it 'moderation'? Your retina's not a Netflix show-you can't just pause it and come back later. You knew the rules. You broke them. Now you get the consequences. And no, I won't feel bad for you.
laser hurt? i got mine done last year and it felt like someone was poking me with a hot toothpick. not fun but worth it. my vision still sucks tho. guess i shoulda started earlier
I’ve lived with type 2 for 22 years. No laser. No injections. Just walking 5 miles a day, sleeping 8 hours, and avoiding processed stuff. My eyes are better than my 30-year-old nephew’s. It’s not magic. It’s discipline. And yes, it’s harder than the system wants you to believe.
They want you to think laser is the answer. But let me tell you what they don’t say: after the laser, your peripheral vision ghosts out. You’re left seeing in a tunnel. That’s not saving your sight-that’s trading one hell for another. I’d rather be blind than live like a robot with a spotlight for a view.
I’ve been a nurse for 18 years, and I’ve seen too many people ignore this until it’s too late. The real hero here isn’t the laser-it’s the person who shows up for their yearly eye exam even when they feel fine. That’s the quiet act of courage that keeps people seeing their grandkids, reading bedtime stories, watching sunsets. Don’t wait for the warning signs. Be the one who shows up before they appear.