Why Medication Safety Matters More Than You Think
Getting a new prescription can feel overwhelming. You’re handed a bottle, told when to take it, and sent on your way. But what happens if you take it wrong? Or mix it with something else? Or forget to check the expiration date? These aren’t just small mistakes-they’re real risks. In the U.S. alone, over 1.3 million people end up in the emergency room every year because of bad reactions to medicines. About 350,000 of those cases need hospital stays. And here’s the scary part: nearly half of these errors could be avoided with simple, clear steps.
Medication safety isn’t just for hospitals or nurses. It’s for you. Whether you’re taking a pill for high blood pressure, an antibiotic for an infection, or even a daily vitamin, getting it right saves your health-and possibly your life.
The Six Rights of Taking Medicine (And How to Remember Them)
Healthcare professionals use a simple checklist called the "Six Rights" to avoid mistakes. As a patient, you should use it too. Here’s what each one means and how to apply it:
- Right patient: Make sure the name on the bottle matches yours. If you’re picking up medicine at the pharmacy, confirm your full name and date of birth. Never assume it’s yours just because the label looks familiar.
- Right medication: Double-check the drug name. Generic versions look different from brand names. For example, metoprolol is the generic version of Lopressor. Ask your pharmacist: "Is this the same as what my doctor ordered?"
- Right indication: Know why you’re taking it. Don’t just take it because "the doctor said so." Ask: "What condition is this for?" If you’re unsure, call your doctor. Taking the wrong medicine for the wrong reason can make things worse.
- Right dose: Use the measuring device that comes with the medicine. Never use a kitchen spoon. A tablespoon from your drawer can be 25% more or less than it should be. Liquid medicines need precise drops or milliliters. If the cap has a built-in dropper or cup, use that.
- Right route: Is it meant to be swallowed, applied to the skin, or inhaled? Taking a cream orally or a pill as a suppository can be dangerous. Read the instructions carefully.
- Right time: Some medicines work best on an empty stomach. Others need food. Some need to be taken at the same time every day. Set a phone alarm if you need to. Missing doses or taking them too close together can cause side effects or make the medicine useless.
Keep a Medication List-No Exceptions
Most people don’t realize they’re taking more than they think. Prescription drugs, over-the-counter pain relievers, herbal supplements, vitamins-even daily aspirin-can interact. The CDC says patients who keep a full, updated list of everything they take have 27% fewer medication errors.
Make a simple list. Include:
- Drug name (brand and generic if you know it)
- Dose (e.g., 10 mg, 5 mL)
- How often (e.g., once daily, twice a day)
- Why you take it (e.g., "for blood pressure")
- When you started
Carry this list with you to every doctor’s visit, ER trip, or pharmacy pickup. Even if you think they already know, show it. Most errors happen when providers don’t have the full picture. And update it every time you start or stop a medicine.
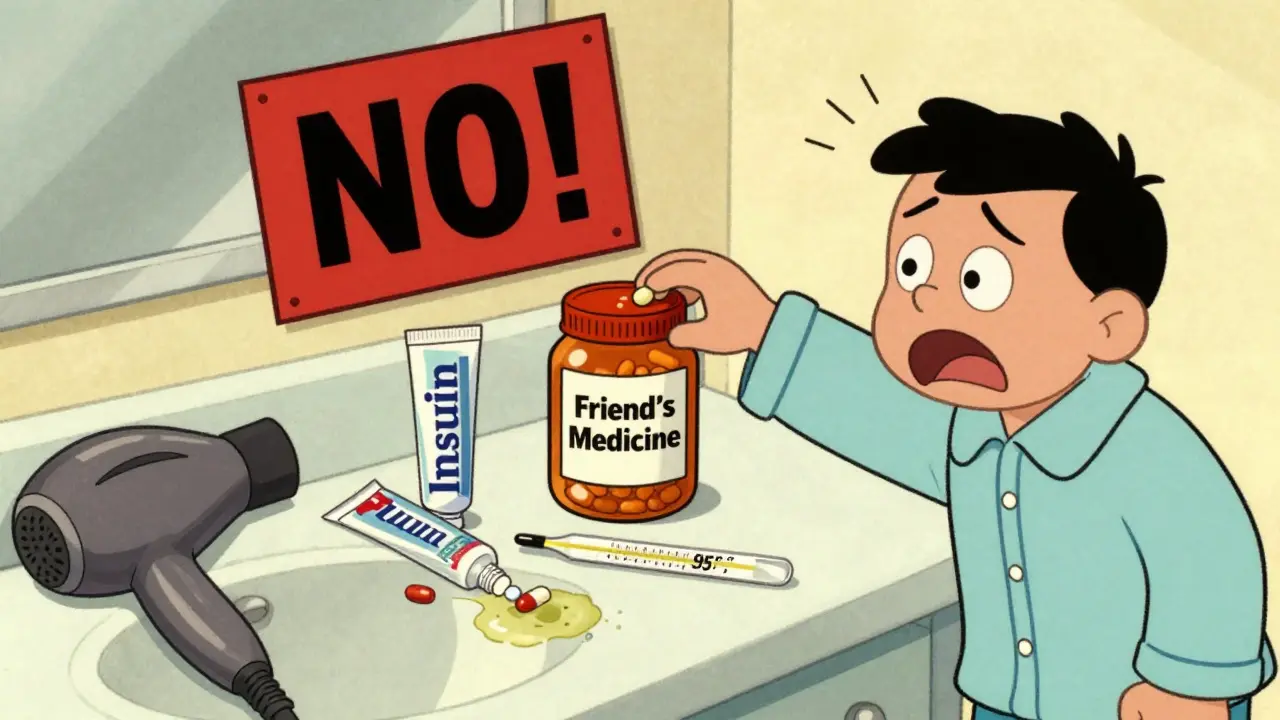
Storage Matters-More Than You Realize
Medicines aren’t like cereal. They don’t last forever, and they don’t like heat or moisture.
Insulin? Must be refrigerated until first use. After that, it can stay at room temperature for up to 28 days. Heat ruins it. If you leave it in the car on a hot day, it won’t work.
Most pills? Store them below 86°F (30°C), away from the bathroom. Humidity turns tablets into mush. Keep them in a cool, dry drawer, not above the sink.
Check expiration dates. The FDA says 18% of medication errors come from using expired drugs. Antibiotics and liquid medicines degrade faster. If it smells weird, looks discolored, or feels sticky, don’t take it. Ask your pharmacist to replace it.
Never Share Medicines-Even If You Have the Same Symptoms
"My friend took this for her headache and it worked. Maybe it’ll help me?" That’s a dangerous thought.
What works for one person can harm another. A pill that helps your friend’s migraine might cause a dangerous drop in blood pressure for you. Or you could be allergic to an ingredient you didn’t know was in it.
The FDA says sharing prescriptions causes 8% of emergency visits for drug reactions. That’s not rare. That’s preventable. If you need medicine, get your own prescription. Don’t borrow. Don’t give.
Ask Questions-Even If You Feel Silly
Most people don’t ask enough. A 2022 study found that patients who asked at least three questions about a new medicine had 34% fewer side effects in the first month.
Here are three questions you must ask every time you get a new prescription:
- What should I do if I miss a dose? Only 22% of patients ask this. But it’s critical. Some medicines need to be taken as soon as you remember. Others should be skipped. Getting it wrong can be dangerous.
- How should I store this? 40% of medications have special storage needs. If you don’t know, you might ruin it.
- What side effects should I watch for? Only 65% of pharmacy consultations cover this. Know what’s normal (like mild nausea) and what’s not (like swelling, chest pain, or trouble breathing). Call your doctor if you’re unsure.
Also ask: "Is this a generic version?" and "Will this interact with my other medicines?" Pharmacists are trained to answer these. Don’t be shy.

Use Tools to Stay on Track
Remembering when to take five different pills every day is hard. That’s why apps like Medisafe and MyMeds exist. A 2022 study showed they improve adherence by 28% for first-time users.
These apps let you:
- Scan the barcode on your bottle to auto-fill details
- Set reminders with sound and vibration
- Get alerts if you’re due for a refill
- Track side effects and share reports with your doctor
Even a simple phone alarm works. Set one for morning, noon, and night. Put your pills in a pill organizer with labeled compartments. Don’t rely on memory.
What to Do When Something Goes Wrong
Even with the best care, mistakes happen. If you think you took the wrong dose, or you feel strange after taking a new medicine:
- Don’t panic. Don’t take another dose.
- Call your pharmacist. They’re available during business hours and often after hours too.
- If you have serious symptoms-trouble breathing, swelling, chest pain, confusion-go to the ER or call emergency services.
- Write down what happened: what you took, when, how much, and how you felt. This helps doctors help you faster.
Report errors. If you got the wrong medicine from the pharmacy, tell them. If a label was unclear, let the FDA know through their MedWatch program. Your report could help someone else avoid the same mistake.
Final Thought: This Is Your Health-Take Control
Medication safety isn’t complicated. It’s about paying attention. It’s about asking. It’s about writing things down. It’s about not assuming anything.
It takes most people two to three weeks to build a solid routine. You won’t get it perfect right away. That’s okay. Just keep improving. Every time you double-check a label, ask a question, or use your pill organizer, you’re lowering your risk. And that’s not just smart. It’s life-saving.



Comments
bro i just took my blood pressure pill with coffee because i was in a rush and now my heart feels like it’s trying to escape my chest. thanks for the reminder lol
this is literally the most important post i’ve read this year 🙏. i used to think meds were just little pills you swallow and forget. now i carry my list in my wallet. my grandma’s life changed because of this. 🌱💊
I can’t believe how many people don’t check expiration dates. I had a friend take expired antibiotics last year-she ended up in the hospital with a C. diff infection. It’s not just about being careful-it’s about being alive.
so like... i live in india and we just buy pills off the street sometimes because the pharmacy is 20km away and we dont have time. also my cousin gave me his migraine pills once and i took em and it worked so... yknow? maybe the system is broken? but also i guess you're right? idk man
this is just another government pamphlet dressed up as advice. people don’t need more rules. they need better access to doctors. fix that first.
i never knew you couldn’t store pills in the bathroom. i’ve been keeping my ibuprofen next to the shower for 5 years. should i be worried? 😅
lol i shared my zoloft with my sister when she was sad and she said it made her feel like a robot. so... maybe don't do that? just saying
the six rights? please. i’ve been taking meds for 15 years and i’ve never needed a checklist. you treat patients like children. adults know what they’re doing
this is why america is falling apart. people can’t even take a pill right. we need to stop coddling everyone with pamphlets and start teaching responsibility in school
i use medisafe and it’s a game changer. i used to forget my thyroid med for weeks. now it pings me and i even get a little confetti animation. yes. i cry every time. 🥲
if you’re taking vitamins, you’re already doing it wrong. you don’t need supplements unless you’re a malnourished toddler. and if you’re taking someone else’s meds? you’re not just careless-you’re selfish.
I’ve worked in rural clinics in Uttar Pradesh for 12 years. People here often take half a pill because they can’t afford the full dose. The real issue isn’t ignorance-it’s poverty. No checklist fixes that. But this post? It’s a start.
i used to be a nurse. let me tell you, 90% of these mistakes? they’re from people who refuse to read the label. i once had a guy take his insulin like it was soda. he thought it was a flavor. i’m not joking. this isn’t rocket science. why do we keep making it harder?
i just realized i’ve been taking my blood thinner at night instead of morning and i’ve been doing it for 2 years. oh god
i’m from the uk and we get our meds in those little blister packs with the days printed on them. it’s so much easier. maybe the us should try that? just a thought 💬