Every year, thousands of people end up in the hospital not because their condition got worse, but because two medications they were taking clashed in ways no one saw coming. One person takes warfarin for a blood clot and starts a new antibiotic. Within days, their blood thins too much. Another drinks grapefruit juice with their statin, not knowing it turns a safe dose into a dangerous one. These aren’t rare accidents. They’re drug interactions - and they’re one of the most preventable causes of harm in modern medicine.
What Exactly Is a Drug Interaction?
A drug interaction happens when something changes how a medication works in your body. It’s not just about two pills mixing. It can be a food, a supplement, an herbal remedy, or even a health condition you have. The result? The drug might become too strong, too weak, or cause side effects you didn’t expect.There are three main types:
- Drug-drug interactions: When one medication affects another. This is the most common type, making up about 80% of serious cases.
- Drug-food/drink interactions: When what you eat or drink changes how the drug is absorbed or broken down. Grapefruit juice is the classic example.
- Drug-condition interactions: When your existing health problem changes how a drug behaves. For example, kidney disease can cause certain drugs to build up to toxic levels.
These aren’t just theoretical risks. They’re real, measurable dangers. In the U.S., drug interactions lead to over 1.3 million emergency room visits and 350,000 hospital stays every year. That’s more than many common infections. And it’s not just about being hospitalized - an estimated 106,000 deaths each year are linked to preventable drug reactions, many of them caused by interactions.
How Do Drug Interactions Actually Work?
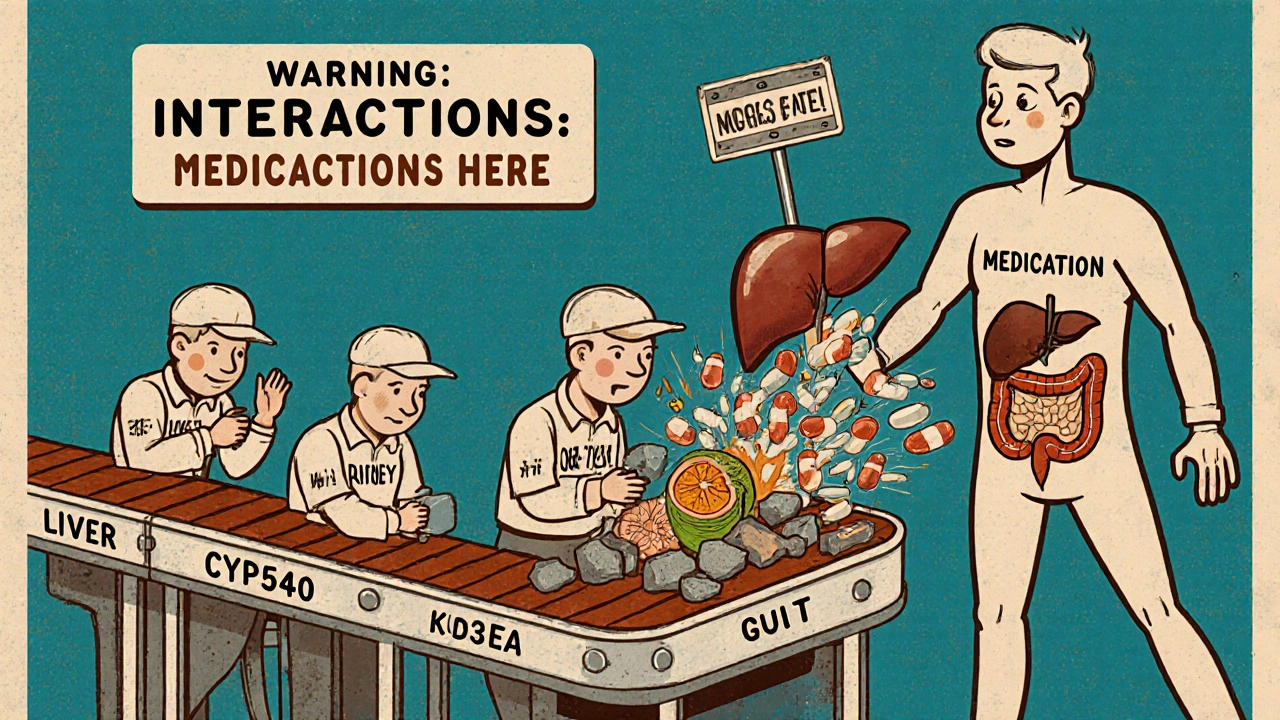
It helps to think of your body like a factory. Medications are workers that need to get to the right place, at the right time, in the right amount. Interactions mess with that process in two main ways.Pharmacokinetic interactions change how your body handles the drug - where it goes, how fast it’s broken down, or how it’s cleared out. The most common player here is a group of liver enzymes called CYP450. CYP3A4 alone processes about half of all prescription drugs. If another substance blocks or speeds up this enzyme, the drug’s level in your blood can skyrocket or crash.
Take simvastatin, a cholesterol-lowering drug. If you take it with fluconazole (an antifungal), CYP3A4 gets blocked. That causes simvastatin levels to jump up to 2,000%. That’s not just a small increase - it’s enough to cause rhabdomyolysis, a life-threatening muscle breakdown that can lead to kidney failure.
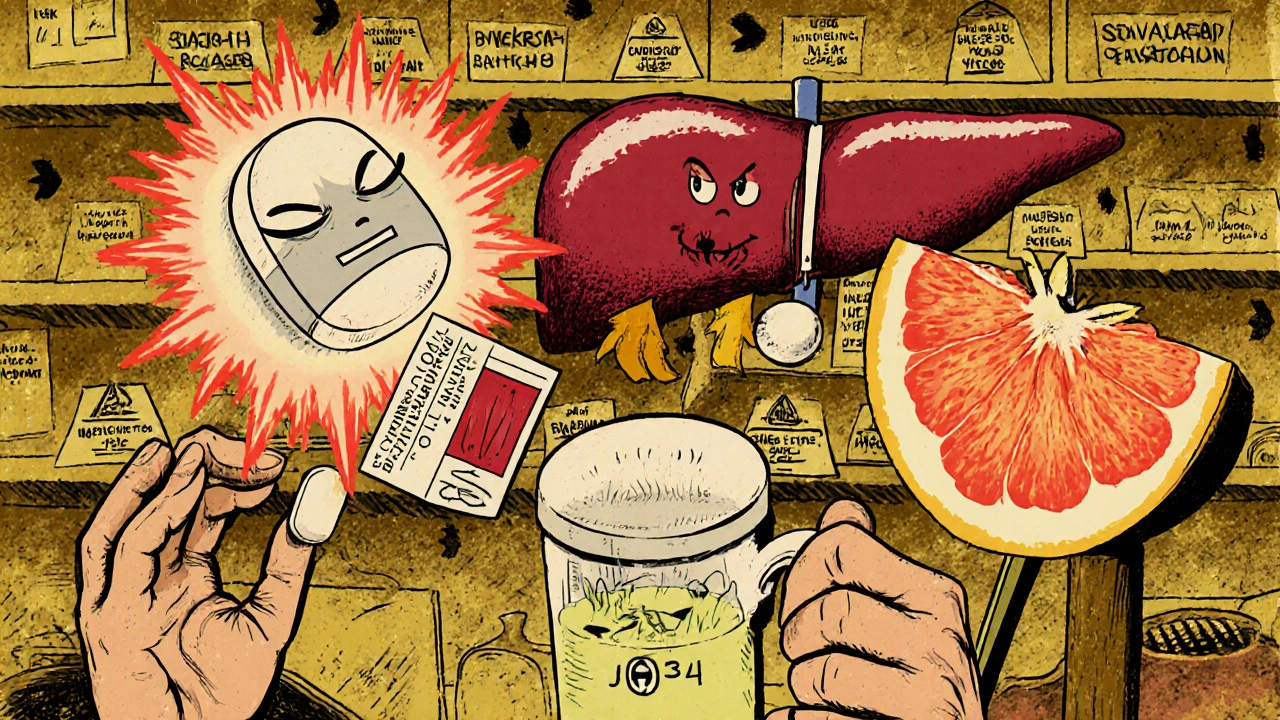
Another classic is grapefruit juice. It contains compounds called furanocoumarins that shut down CYP3A4 in your gut. That means more of the drug enters your bloodstream before your liver can break it down. For statins like simvastatin or atorvastatin, that can mean 300-600% higher blood levels. One patient in a 2023 FDA report was hospitalized after drinking grapefruit juice daily with simvastatin - he had no symptoms until he developed muscle pain and dark urine. By then, his kidneys were already failing.
Pharmacodynamic interactions are about what the drug does at its target site. Two drugs might have the same effect - like two sedatives - and together they cause extreme drowsiness or even breathing problems. Or they might cancel each other out. For example, NSAIDs like ibuprofen can make diuretics less effective by making your body hold onto salt and water. Beta-blockers can block the same receptors that asthma inhalers use, making them useless during an attack.
Which Medications Are Most Likely to Cause Problems?
Not all drugs are created equal when it comes to interactions. Some are like ticking time bombs.- Warfarin (Coumadin): This blood thinner has over 600 known interactions. Antibiotics, antifungals, even cranberry juice can throw off your INR (a blood test that measures clotting). One Reddit thread with 147 user stories showed 68% of people had dangerous spikes in INR after starting a new antibiotic.
- Digoxin (Lanoxin): Used for heart failure and irregular heartbeat. It interacts with over 300 drugs. Diuretics that lower potassium can make digoxin toxic. Antibiotics like clarithromycin can spike its levels.
- Levothyroxine (Synthroid): For hypothyroidism. If you take it with calcium, iron, or even coffee, your body absorbs less of it. That means your thyroid levels stay low, even if you’re taking the right dose.
- Anticoagulants like Xarelto and Eliquis: These newer blood thinners still have dozens of interactions, especially with antifungals and certain antibiotics. Patient reviews on Healthgrades show Xarelto has over 1,200 interaction complaints - the highest of any drug in its class.
Even over-the-counter meds can be risky. Painkillers like ibuprofen or naproxen can interfere with blood pressure drugs. Cold medicines with pseudoephedrine can raise blood pressure in people already on heart meds. And don’t forget supplements - St. John’s wort can make birth control, antidepressants, and even some cancer drugs stop working.
Who’s at the Highest Risk?
You might think this only affects older adults - and you’d be right. But it’s not just age. It’s complexity.People over 65 take an average of 4.7 prescription medications daily. That’s a lot of chances for things to go wrong. In fact, they account for 45% of serious interaction events, even though they make up only 16% of the population. A 2022 AARP survey found that 42% of Medicare beneficiaries had at least one harmful interaction.
People with five or more chronic conditions are even more vulnerable - 68% of them experience at least one significant interaction. Why? Because each condition brings its own set of drugs. A person with heart disease, diabetes, arthritis, depression, and high cholesterol might be on 10 or more medications. That’s a minefield.
And here’s the scary part: most of these interactions happen because care is fragmented. You see a cardiologist, a rheumatologist, a psychiatrist - each prescribes what they think is best. But no one looks at the whole picture. A 2022 study found that 34% of patients leaving the hospital had at least one undocumented interaction risk because their doctors didn’t know what else they were taking.
How to Protect Yourself
The good news? Almost all of these are preventable. You don’t need to be a doctor to stay safe.- Keep a complete, updated list of everything you take: prescriptions, over-the-counter meds, vitamins, herbs, and supplements. Include the dose and how often you take it. Keep it on your phone and in your wallet.
- Use one pharmacy. Pharmacists are trained to catch interactions. When all your meds come from one place, they can run a full check every time you pick something up. In the U.S., pharmacists resolve 3.5 million drug-related problems each year - 22% of those are interactions.
- Ask two questions every time you get a new prescription: "Can this interact with anything else I’m taking?" and "Is there a food or drink I should avoid?" Don’t assume your doctor knows your full list - many don’t.
- Take meds at least 2 hours apart from supplements or foods that interfere. For example, take levothyroxine on an empty stomach, then wait two hours before eating or taking calcium.
- Use trusted tools. The FDA-approved GoodRx Drug Interaction Checker, Medscape’s free tool, or the NIH’s LiverTox database are reliable. Avoid random websites - many are incomplete or outdated.
There’s also the Beers Criteria - a list of 54 high-risk medications and interactions for older adults. If you’re over 65, ask your doctor if your meds are on it. Studies show using this list cuts adverse events by 27%.
The Bigger Picture: Why This Isn’t Just Your Problem
Drug interactions aren’t just a personal risk - they’re a system failure. The U.S. spends $528 billion a year on medication-related problems. $30 billion of that is from avoidable hospital visits and ER trips caused by interactions.Even the technology meant to protect us isn’t perfect. While 89% of U.S. hospitals have electronic systems that flag interactions, only 42% give real-time, severity-based alerts. Too many systems just say "possible interaction" without telling you if it’s dangerous or harmless.
And here’s something most people don’t know: pharmaceutical companies don’t test for most interactions before a drug hits the market. Only 25% of clinically significant interactions are found in clinical trials. That’s because trials exclude older patients, those with multiple conditions, or people taking other meds. So the real-world risks only show up after millions of people start using the drug.
That’s why post-marketing surveillance is critical. The FDA’s new Drug Interaction Knowledgebase (DIKB) is a step forward - it’s a machine-readable database with 12,000+ validated interactions. But it’s still early days. The future lies in personalized medicine: using your genes to predict how you’ll react. The FDA already includes pharmacogenetic info for over 350 drugs. By 2026, testing for CYP450 variants could become standard for high-risk meds.
Final Thought: You’re the Last Line of Defense
Doctors, pharmacists, and algorithms can help - but they can’t know everything. Only you know what you’re really taking, how you’re feeling, and what you’ve eaten or drunk that day. If something feels off - dizziness, muscle pain, unusual bruising, or just a sense that "this isn’t right" - speak up. Bring your list. Ask again. Push for clarity.Medication safety isn’t about avoiding drugs. It’s about using them wisely. And that starts with understanding that no pill exists in isolation. Every tablet, capsule, or injection is part of a complex web - and you hold the key to keeping it safe.
What are the most common drug interactions?
The most common and dangerous drug interactions involve blood thinners like warfarin, cholesterol drugs like simvastatin, and heart medications like digoxin. Warfarin interacts with over 600 substances, including antibiotics, antifungals, and even cranberry juice. Simvastatin combined with grapefruit juice or certain antifungals can cause life-threatening muscle damage. Diuretics and NSAIDs like ibuprofen often reduce each other’s effectiveness, while antidepressants and St. John’s wort can cancel each other out.
Can food really affect how my medicine works?
Yes, and grapefruit juice is the most well-known example. It blocks enzymes in your gut that break down certain drugs, causing much higher levels in your blood. This can turn a safe dose of a statin into a toxic one. Other foods matter too: leafy greens can interfere with warfarin, dairy can block thyroid meds, and alcohol can make sedatives or painkillers dangerously strong. Always ask what to avoid with your new prescription.
Are over-the-counter meds and supplements safe to mix with prescriptions?
No, not necessarily. Many people assume OTC drugs and supplements are harmless, but that’s not true. Ibuprofen can raise blood pressure in people on ACE inhibitors. Calcium and iron supplements can block absorption of thyroid medication. St. John’s wort can make birth control, antidepressants, and even some cancer drugs ineffective. Always include every supplement and OTC drug on your medication list - even if you think it’s "just a vitamin."
Why do I need to use one pharmacy for all my prescriptions?
Pharmacists are trained to spot dangerous combinations that doctors might miss. When you use one pharmacy, they build a full profile of your meds and check every new prescription against your entire list. If you go to different pharmacies, each one only sees part of your picture - and that’s when dangerous gaps happen. Using a single pharmacy can reduce your risk of an interaction by up to 40%.
What should I do if I think I’m having a drug interaction?
Stop taking the medication immediately and call your doctor or pharmacist. Don’t wait for symptoms to get worse. Signs of a serious interaction include unexplained bruising or bleeding (with blood thinners), muscle pain or weakness (with statins), extreme drowsiness, confusion, rapid heartbeat, or swelling. Keep your full medication list handy - it will help them act faster. If symptoms are severe, go to the ER.
Are drug interactions more common in older adults?
Yes. People over 65 take an average of 4.7 prescription medications daily, and their bodies process drugs more slowly. They’re also more likely to have multiple chronic conditions, each requiring its own meds. This creates a perfect storm for interactions. In fact, older adults experience drug interactions at three times the rate of younger people. The Beers Criteria - a list of high-risk meds for seniors - is designed specifically to help reduce this risk.
Can electronic health records prevent drug interactions?
They help, but they’re not foolproof. Most hospitals and clinics have systems that flag possible interactions, but only 42% give clear, severity-based alerts. Many just say "possible interaction" without telling you if it’s dangerous or not. Plus, if your meds aren’t fully entered - like if you forget to mention a supplement - the system won’t catch it. Your own list is still the most reliable tool.


Comments
Look, I get it, drugs interact. Big surprise. But let’s be real-most people aren’t taking 10 meds at once. This whole post reads like a pharmacy pamphlet written by someone who’s never met a human being. I take two pills a day, one for blood pressure and one for cholesterol. I drink grapefruit juice every morning. Never had a problem. Maybe the real issue is that doctors prescribe too much crap in the first place. Stop scaring people into thinking every pill is a landmine. Most of us are fine.
The data here is technically accurate but fundamentally misleading. 1.3 million ER visits? Sure. But how many of those were due to noncompliance, self-medication, or patients not disclosing supplements? The system is broken because patients lie, doctors don’t listen, and pharmacists are overworked. Blaming the drugs or the interactions is like blaming cars for traffic accidents caused by drunk drivers. The real problem is human behavior, not pharmacology. Also, 106,000 deaths? That’s less than 0.03% of all prescription users. Don’t turn a statistical blip into a national crisis.
soooo i took my levothyroxine with coffee once bc i was in a rush and then my doctor was like "why are your levels still low" and i was like "uhhh" lol. now i wait 2 hours. also i stopped taking st johns wort after i got my period like 3x in a month. turns out it messes with birth control?? who knew?? anyway i’m just saying… read the damn pamphlet. it’s not that hard. also i use goodrx now. it’s free. use it.
my grandma died because they gave her a new heart med and didn’t check what else she was on. she was on warfarin and they gave her some new antibiotic and she started bleeding out in her sleep. they didn’t even know she was on it. that’s not a "drug interaction" that’s a crime. why do they even let people prescribe if they don’t even ask what you’re taking? i mean come on. my mom’s on 7 meds and i have to be the one to keep the list because no one else cares. this isn’t science, it’s negligence.
This is such an important post and I’m so glad someone took the time to write it clearly. I used to think OTC meds were harmless too-until I started taking ibuprofen for my arthritis and my blood pressure went through the roof. My pharmacist caught it before I ended up in the hospital. Seriously, use one pharmacy. Keep a list. Ask the two questions. It’s not hard, and it could save your life. You’re not being paranoid-you’re being smart. Keep spreading this info!
Oh wow. A 2,000% increase in simvastatin levels? How did anyone survive the 20th century? Did people just randomly take statins with antifungals and then die quietly in their recliners? And let’s not forget the 106,000 deaths-surely those were all people who didn’t read the tiny print on the bottle, right? Or maybe they were just too lazy to Google "drug interaction"? Honestly, if you can’t figure out that grapefruit juice + statin = bad, maybe you shouldn’t be allowed to own a pill organizer. I’m just saying.
The CYP450 system is a fascinating biochemical pathway, but the author’s reductionist framing ignores the complexity of polypharmacy in real-world clinical settings. The pharmacokinetic mechanisms are well-documented, yet the article fails to address pharmacogenomic variability across populations-particularly the differential expression of CYP3A4*22 and CYP2C9*3 alleles in non-Caucasian cohorts. Without acknowledging this, the entire risk assessment framework is ethnocentric and statistically flawed. Also, the FDA’s DIKB is still in beta. It’s not a database-it’s a prototype.
Why are we letting foreign drug companies dictate our medicine? Look at this-U.S. patients are dying because some lab in India or China didn’t test interactions properly. We’ve got the best scientists in the world. Why aren’t we making our own meds? And why do we trust some app on a phone to tell us what’s safe? I take my pills the way my grandpa did-no apps, no juice, no supplements. Just the doctor’s script and water. Maybe we need to go back to basics instead of overcomplicating everything with tech and fear-mongering.
While the empirical data presented is compelling, one must consider the epistemological limitations of Western biomedicine in addressing polypharmacy. In Ayurvedic tradition, drug-food interactions are understood through the lens of doshic balance-not enzyme inhibition. The reduction of pharmacological activity to CYP450 pathways is a colonial imposition on holistic health systems. Furthermore, the assertion that "you are the last line of defense" places undue burden on the individual while absolving institutional negligence. Perhaps the real solution lies not in personal vigilance, but in systemic reform of pharmaceutical oversight and equitable access to pharmacogenetic screening.